Back to Journals » Clinical Ophthalmology » Volume 10
Corneal endothelial changes after accelerated corneal collagen cross-linking in keratoconus and postLASIK ectasia
Authors Badawi A
Received 23 May 2016
Accepted for publication 20 July 2016
Published 30 September 2016 Volume 2016:10 Pages 1891—1898
DOI https://doi.org/10.2147/OPTH.S113412
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Amani E Badawi
Department of Ophthalmology, Mansoura University, Mansoura, Egypt
Purpose: The purpose of this study was to evaluate the effects of accelerated cross-linking (CXL) on corneal endothelium in keratoconus and postlaser-assisted in situ keratomileusis (LASIK) ectasia.
Design: This study is a prospective nonrandomized controlled study.
Setting: This study was conducted in Mansoura Ophthalmic Center (Mansoura University) and Al-Mostakbal Ophthalmic Center, Mansoura, Egypt.
Methods: In total, 40 eyes with progressive keratoconus and 10 eyes with postLASIK ectasia were subjected to an accelerated CXL (10 mW/cm2 for 9 minutes). Qualitative and quantitative analyses of the corneal endothelial cells were conducted before CXL and 3, 6, and 12 months after CXL by using a specular microscope (Tomy EM-3000).
Results: There was a significant reduction in endothelial cell count particularly at 3 and 6 months postCXL. In addition, the coefficient of variance was also statistically significantly higher at 3 and 6 months postoperatively than the preCXL value. There was a slight change in the percentage of hexagonal cells.
Conclusion: The use of accelerated CXL (10 mW/cm2 for 9 minutes) has a transient negative impact on endothelial cell density and/or endothelial morphology.
Keywords: keratoconus, postLASIK ectasia, accelerated cross-linking, corneal endothelium
Introduction
Corneal endothelium is a delicate layer of the cornea that maintains corneal deturgescence and transparency through regulating fluid and solute transport between the aqueous and corneal stroma.1 Endothelial cell analysis is one of the methods that is used to assess the health of the cornea, especially after surgical intervention2 and is also one of the major criteria that are used to assess the long-term outcomes of any corneal surgery.3
Keratoconus (KC) is a degenerative disorder characterized by corneal thinning and secondary ectasia with irregular astigmatism.4 Postlaser-assisted in situ keratomileusis (LASIK) ectasia is a visually devastating complication with reported incidence ranging from 0.04% to 0.6%.5 First, a study on the use of cross-linking in KC was conducted in 2003, which was considered a promising treatment to halt the progress of KC.6 Then, further studies have evaluated the safety of the standard CXL mode with some modifications.7–10 However, only a few reports on the outcome of accelerated cross-linking in KC patients and postLASIK are available in the medical literature.11,12
The aim of this study was to evaluate the effects of accelerated CXL on corneal endothelium in KC and postLASIK ectasia, concerning the safety of the time and irradiation intensity settings that are currently in use.
Patients and methods
This is a prospective study carried out on patients attending Mansoura Ophthalmic Center (Mansoura University) and Al-Mostakbal Ophthalmic Center during the period from May 2013 to March 2015. Patients who did not come for follow-up visits were excluded.
Inclusion criteria
The following were the inclusion criteria in this study:
- Topographic and tomographic evidence of KC (Grade I and Grade II Amsler–Krumeich classification) or postLASIK ectasia (maximum K reading <54 D)
- With documented clinical worsening and instrumental progression by an increase of 1.0 D or more in maximum K reading and reduction of the thinnest point of pachymetry 10 μm or more, at least >3–6 months of follow-up
- Minimal corneal thickness >400 μm
- Completely clear cornea with the absence of any other ocular or systemic disease
- Aged 18–30 years
Exclusion criteria
The following conditions were the exclusion criteria in this study:
- Corneal thickness of <400 μm at the thinnest point
- History of herpetic keratitis, concurrent corneal infections, or concomitant autoimmune diseases
- Severe dry eye, acute hydrops, severe allergic conjunctivitis, and diffuse central corneal opacity
- Recent contact-lens users
- Advanced KC
- Glaucoma, cataract, or vitreoretinal disorders
- Pregnancy or lactating
- Mental illness
Preoperative examination
Standard slit lamp examination, uncorrected distance visual acuity and corrected distance visual acuity measurement, dilated fundus examination using noncontact Volk 90 lens, and indirect ophthalmoscope were conducted before treatment. Corneal tomography was performed by using Scheimpflug camera (Oculus Pentacam®; Oculus Optikgerate GmbH, Wetzlar, Germany), and corneal thickness measurement was taken by using Scheimpflug camera and was confirmed by a noncontact specular microscope (Tomy EM-3000; Tomy USA, E-Mohawk Lane Phoenix, AZ, USA). Corneal endothelial cell analysis was also carried out by using the noncontact specular microscope.
Collagen cross-linking technique
All patients were examined under sterile conditions in the operating room of Al-Mostakbal Ophthalmic Center, Mansoura, Egypt. After applying topical anesthetic eye drops of benoxinate hydrochloride 0.4% (Benox 4%; Eipico Inc., Cairo, Egypt), the epithelium was mechanically scraped within the central 8 mm diameter area by using a Beaver Blade® (Beaver-Visitec International, Inc. Waltham, MA, USA). Then, riboflavin ophthalmic solution, that is, 0.1% riboflavin, saline with hydroxypropyl methylcellulose (VibeX Rapid™; Avedro Inc., Waltham, MA, USA) was applied every 2 minutes for 10 minutes until the stroma was completely saturated. Ultraviolet A (UVA) irradiation was achieved at an irradiance of 10 mW/cm2 and a 370 nm wavelength for 9 minutes with a constant energy dose of 5.4 J/cm2 at 5 cm distance from the cornea under the continuous light mode using a commercially available UVA irradiation system, CBM Vega 10-mW X-Linker (VEGA CSO, Srl Via degli Stagnacci, 12/E 50018, Scandicci, Firenze, Italy). During irradiation, riboflavin solution was applied at the rate of one drop for every 2 minutes to ensure saturation.
Postoperative care and follow-up
Patients received moxifloxacin hydrochloride ophthalmic solution 0.5% (Vigamox®; Alcon Laboratories, Inc., Fort Worth, TX, USA) five times daily for 1 week. A bandage soft contact lens was applied until reepithelialization was complete. Then, patients received topical steroid antibiotic drops tobramycin and dexamethasone (Tobradex®; Alcon Laboratories, Inc.) four times daily for 1 week and then tapered off for the next 3 weeks; and carboxymethylcellulose sodium 0.5% eye lubricant (Refresh Tears®; Allergan, Inc., Dupont Drive, Irvine, CA, USA) six times daily for 1 month. The first follow-up was done 1 day postoperatively, for 3 days in order to confirm complete epithelial healing and contact lens removal, and then after 1 week and 1, 3, 6, and 12 months.
Endothelial cells evaluation
In order to analyze the effects of using CXL parameters on corneal endothelial cells both preoperatively and 3, 6, and 12 months postoperatively, endothelial cell density (ECD), the percentage of coefficient of variance (CV) of hexagonal cells (6A), average cell size, maximum cell size, and minimum cell size were measured with a noncontact specular microscope (Tomy EM-3000; Tomy USA) at Mansoura Ophthalmic Center, and the results were compared. The measurement was taken from the central cornea. Endothelial cell photographs were collected by using the automatic-mode low-flash intensity and were analyzed later. At least three measurements were taken to improve intersession repeatability of the device.
The present study was conducted and adhered to the Declaration of Helsinki. The Ethics Committee, Faculty of Medicine, Mansoura University, reviewed and approved the study (approval number, R/16.03.55). The nature of the procedure and its possible consequences were clarified to the participants, and written informed consents were obtained from all of them before conducting the study.
Data analysis
Data were tabulated, coded, and then analyzed using the computer program Statistical Package for Social Science, Version 17.0 (SPSS Inc., Chicago, IL, USA), in order to obtain the descriptive data and analytical statistics.
Descriptive data
Descriptive statistics were calculated in the following forms:
- Mean ± standard deviation
- Frequency (number-percent)
Analytical statistics
In order to compare the statistical data among different groups, the significance of difference was tested using repeated-measures analysis of variance that is used to compare among more than two groups by repeatedly measured numerical (parametric) data followed by post hoc least significant difference test.
Results
In total, 40 eyes of 24 patients (13 females, 54.2%; and eleven males, 45.8%) with Grade I and Grade II KC (according to Amsler–Krumeich classification) and ten eyes of eight patients (six females, 75%; and two males, 25%) with postLASIK ectasia were included in this study. The mean age of KC eyes was 22.54±3.07 years, and the mean age of postLASIK eyes was 24.54±3.07 years (Table 1). All patients were followed-up for a period of at least 1 year (mean follow-up: 18.2 months; standard deviation: ±6.5 months; range: 13–25 months). Six patients (eleven eyes: ten KC eyes and one postLASIK eye) did not complete the postoperative follow-up, and therefore, they were excluded from this study.
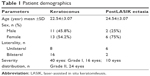  | Table 1 Patient demographics |
In KC patients, mean baseline ECD was 2,633.40±283.10 cell/mm2. Three months after the procedure, it was 2,456.65±236.07 cell/mm2 (P=0.000); at 6 months, it was 2,589.55±253.42 cell/mm2 (P=0.029); and at 12 months, it was 2,610.00±271.18 cell/mm2 (P=0.001). The difference between the baseline and 12 months postoperative values was significant at P<0.001 (Table 2). The calculated endothelial cell loss rate was 6.7% at 3 months and reduced to 1.67% and 0.89% at 6 and 12 months, respectively.
On the other hand, in postLASIK patients, mean preoperative ECD was 2,698.40±189.11, and this value changed to 2,630.00±193.09 at 3 months, 2,700.20±190.49 at 6 months, and 2,700.60±185.31 at the end of 1 year. The difference between the baseline and 12 months postoperative values was also highly significant with P<0.001 (Table 2). The calculated endothelial cell loss rate was 2.53% at 3 months with recovery at the end of 1 year to reach a value close to the preoperative one.
The mean baseline coefficient of variation (polymegethism) in KC eyes was 35.03±7.13. Three months after the procedure, it was 45.85±8.80 (P=0.000); at 6 months, it was 36.60±5.61 (P=0.644), and at 12 months, it was 35.65±5.30 (P=1.000). The difference between preoperative and 12 months postoperative values was significant at P<0.001 (Table 3). In postLASIK patients, this value changed significantly from 26.60±1.58 preoperatively to 38.40±6.48, 33.80±4.02, and 32.60±3.50 at 3, 6, and 12 months, respectively (Table 3).
The mean percentage of hexagonal cells (pleomorphism) in KC eyes increased insignificantly 12 months after surgery (55.654%±9.89%) compared with the preoperative value (54.48%±11.39%; P=1.000). The difference between baseline mean percentage and 1 year postoperative values was insignificant at P=0.049. On the other hand, in postLASIK, it changed from (59.80%±4.29%) preoperatively to (57.00%±8.14%) at 1 year (P=1.000). The difference between preoperative and 12 months postoperative values was significant at P<0.001 (Table 4).
In KC eyes, the mean average cell size significantly increased from 335.35±30.94 μm to 389.43±37.84 μm (P=0.000) at 3 months. Then, it decreased statistically insignificantly to 355±27.81 μm at 1 year. The difference between the preoperative and 12 months postoperative values was significant at P<0.001. However, it was statistically significantly higher after CXL in postLASIK eyes. It changed from 344.20±16.94 μm preoperatively to 353.00±21.67 μm (P=0.002) at the end of 1 year (Table 5).
The mean maximum cell size in KC eyes increased significantly from baseline value 962.25±236.19 μm to 1,360.50±393.33 μm at 3 months with significant recovery to reach a value close to preoperative value at the end of follow-up (907.73±189.38 μm). In postLASIK patients, the analysis of variance test is not significant (P>0.05; Table 6). The mean minimum cell size in both KC and postLASIK eyes showed insignificant changes (Table 7).
Table 8 summarizes the results of corneal thickness changes. There was a statistically significant reduction in thinnest pachymetry at the end of 1-year follow-up in both KC and postLASIK eyes.
Discussion
One considerable limitation of accelerated CXL is its impact on the corneal endothelium. Several previous studies have reported contradictory results on corneal endothelial cells after using standard CXL.13–17 However, only few published clinical studies are currently available which evaluate the effects of accelerated CXL on the corneal endothelium by calculating different parameters. The present study evaluated the effects of accelerated CXL on corneal endothelium density, the percentage of hexagonal cells, and CV.
Standard CXL irradiance protocols use UVA energy of 3 mW/cm2 for 30 minutes in association with the application of hydrophilic riboflavin 0.1%. This causes a considerable and relatively acute decline in UVA light of up to 95% and therefore, a resultant irradiance of the endothelium was only 0.15 mW/cm2 (=0.27 J/cm2) with corneal thickness of ≥500 μm.18
According to the Bunsen–Roscoe law of reciprocity, in order to reduce the exposure time of the procedure, a higher intensity of the UVA fluence is required, with a similar overall effect and similar subthreshold cytotoxic endothelial UVA dosage.19 Consequently, treatment at 3 mW/cm2 for 30 minutes is equivalent to that at 9 mW/cm2 for 10 minutes.20
Current treatment protocols use UVA energy at an irradiance of 10 mW/cm2 for 9 minutes and at a 5 cm distance from the cornea, with an application of VibeX Rapid™ (0.1% riboflavin, saline with hydroxypropyl methylcellulose solution) every 2 minutes for 10 minutes before irradiation and one drop every 2 minutes during the irradiation. Now, there are different commercial devices with ultrafast settings such as 18 mW/cm2 for 5 minutes or even 43 mW/cm2 for 2 minutes. Despite the availability of all of these settings, still verification of clinical efficacy and safety are not possible for further studies.20
Significant changes in ECD, CV, and hexagonality were noted after accelerated CXL (10 mW/cm2 for 9 minutes; Figure 1). Nevertheless, increases in ECD in postLASIK eyes at the end of follow-up were not statistically significant when comparing the values preoperatively and 6 months postoperatively. In KC eyes, a considerable decrease in ECD (6.7%) was found at 3 months postprocedure, which gradually improved at 6 months and reached 0.89% at 12 months. On the other hand, the calculated endothelial loss in the postLASIK eyes was less (2.53% at 3 months and improved to reach a value close to preoperative values with a minimal increase at 12 months after CXL). The difference between the values of two groups was significant.
It was known that endothelial cells did not get divided, and therefore, the ECD increased as a result of pre- and postoperative sample errors.21 In addition, it might be attributed to the rearrangement of cells, which might have hidden the actual harm of the endothelial cells.22 Considering the changes in polymegethism (CV), it was statistically significantly higher for 3 months after surgery compared with the preoperative data in both KC and postLASIK eyes. In KC eyes, CV values increased toward the preoperative values at 6 and 12 months. In contrast, in postLASIK eyes, CV was statistically significantly higher for 6 and 12 months after surgery.
The results of the present study were consistent with the results of other two recent studies, although there were some differences in the irradiance parameters. First, Cingü et al23 found significant endothelial cell changes in both density (ECD) and morphology (CV and 6A) following accelerated CXL (18 mW/cm2 for 5 minutes). The substantial obvious changes were observed at the first week and the first month, and then, corneal endothelial count returned to the baseline values at 6 months, whereas 6A and CV returned to their base values only at 3 months.23 The second study24 used more intensive UVA irradiance (30 mW/cm2 for 3 minutes) and reported that changes did not return to its base value. The statistically significant changes in endothelial cell count and coefficient of variance were persistent until the end of 1-year follow-up.24 In contrast, other studies had assumed that accelerated CXL had inconsiderable impacts on the value of ECD and 6-month follow-up of 23 patients with progressive KC treated by accelerated CXL (9 mW/cm2 for 10 minutes) revealed insignificant endothelial cell changes (P=0.082).25 Another comparative study between standard CXL (3 mW/cm2 for 30 minutes) in one eye of 21 patients and accelerated CXL (7 mW/cm2 for 15 minutes) in the fellow eye provided a similar result on the safety of both accelerated and standard CXL on the corneal endothelium.26
Contradictory results were observed in the aforementioned studies because the different protocols of UVA energies were used in those studies; currently, no agreed single protocol is available for accelerated CXL. A more number of randomized clinical trials are required to evaluate each method.
In the present study, there was a significant reduction in the thinnest corneal thickness in both groups (KC and postLASIK ectasia) at 3 months postoperatively, which gradually increased afterward with persisting significant thinning at 1 year, compared with preoperative values. A similar behavior was reported in previous studies on the standard CXL27 or the accelerated CXL.28 This reduction in corneal thickness might be attributed to structural and anatomic collagen fibrils changes with rearrangement of the corneal lamellae or keratocyte apoptosis theory.29 In addition, corneal ischemia was also found as one of the possible causes.30 Although there was a significant decrease in the corneal thickness, no direct statistically significant correlation was found between the endothelium loss and the thinnest corneal thickness. It seems that there are parameters other than the corneal thickness that would be considered as a cause of change in the number of corneal endothelial cells. Using the aforementioned treatment parameters (power at 10 mW/cm2 for 9 minutes with a constant energy dose of 5.4 J/cm2), the results from the current study confirmed early postCXL endothelial changes in both ECD and CV with late recovery. One of the important issues is to find the causes of the changes occurred, although overall safety measurements were maintained.
The higher UVA intensity radiation might lead to the nerve plexus damage and, thus, destroy the endothelial pump performance. The subbasal nerve plexus secretes transported neuropeptides such as calcitonin-gene-related peptide and substance P, which play a supporting role in facilitating the transmission of signals through the Na/K-ATPase pumps in corneal endothelium.31
These corneal endothelial changes mean that the endothelium might be damaged, but might not be totally lost or dead. Therefore, the recovery occurred when the undamaged endothelium slides in and replaces the function in the area of the damaged endothelium. The time by which the postCXL healing process appeared to be complete was known. It might parallel the healing after photorefractive keratectomy.32 The current outcome on corneal endothelium is a potentially substantial consequence of the procedure that deserves further long-term randomized controlled studies.
Limitations
The limitations of this study included the nonrandomized study design, the small sample size, the short follow-up time; and lack of comparison between conventional CXL methods. However, repeated-measures analysis of variance test helped to detect the changes in this small sample study.
Summary
Qualitative and quantitative analysis of the corneal endothelial cells after accelerated CXL (10 mW/cm2 for 9 minutes) in KC eyes showed a significant reduction in ECD by 6.7% at 3 months, 1.67% at 6 months, and then recovery to reach 0.89% at 12 months, whereas it was only 2.53% at 3 months in postLASIK eyes with recovery after 3 months. CV was statistically significantly higher for 3 months after surgery compared with preoperative data in both KC and postLASIK. The hexagonal cells percentage (pleomorphism) in KC and postLASIK eyes showed least effects.
Conclusion
In conclusion, the use of accelerated CXL (10 mW/cm2 for 9 minutes) had a negative impact on ECD and/or endothelial morphology. The existing results confirmed that there was an obvious evidence that the accelerated CXL had significant effects on corneal endothelium, even with a continued safe restoration. The treatment guidelines of accelerated CXL must be followed to reduce its toxic effects.
Disclosure
The author reports no conflicts of interest in this work.
References
Pron G, Ieraci L, Kaulback K. Medical Advisory Secretariat, Health Quality Ontario. Collagen cross-linking using riboflavin and ultraviolet-a for corneal thinning disorders: an evidence-based analysis. Ont Health Technol Assess Ser. 2011;11(5):1–89. | ||
McCarey BE, Edelhauser HF, Lynn MJ. Review of corneal endothelial specular microscopy for FDA clinical trials of refractive procedures, surgical devices, and new intraocular drugs and solutions. Cornea. 2008;27(1):1–16. | ||
Kubaloglu A, Koytak A, Sari ES, Akyol S, Kurnaz E, Ozerturk Y. Corneal endothelium after deep anterior lamellar keratoplasty and penetrating keratoplasty for keratoconus: a four-year comparative study. Indian J Ophthalmol. 2012;60(1):35–40. | ||
Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319. | ||
Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110(2):267–275. | ||
Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen cross-linking for the treatment of kertatoconus. Am J Ophthalmol. 2003;135(5):620–627. | ||
O’Brart DP, Kwong TQ, Patel P, McDonald RJ, O’Brart NA. Long-term follow-up of riboflavin/ultraviolet A (370 nm) corneal collagen cross-linking to halt the progression of keratoconus. Br J Ophthalmol. 2013;97(4):433–437. | ||
Hayes S, Kamma-Lorger CS, Boote C. The effect of riboflavin/UVA collagen cross-linking therapy on the structure and hydrodynamic behaviour of the ungulate and rabbit corneal stroma. PLoS One. 2013;8(1):e52860. | ||
Richoz O, Mavrakanas N, Pajic B, Hafezi F. Corneal collagen cross-linking for ectasia after LASIK and photorefractive keratectomy: long-term results. Ophthalmology. 2013;120(7):1354–1359. | ||
Tariq AA, O’Brart DPS, O’Brart AL, Meek KM. An investigation of trans-epithelial stromal Riboflavin absorption with Ricrolin TE® (Riboflavin 0.1% with trometamol and sodium EDTA) using spectrophotometry. J Cataract Refract Surg. 2012;38(5):884–889. | ||
Tomita M, Mita M, Huseynova T. Accelerated versus conventional corneal collagen crosslinking. J Cataract Refract Surg. 2014;40(6):1013–1020. | ||
Kymionis GD, Tsoulnaras KI, Grentzelos MA, et al. Evaluation of corneal stromal demarcation line depth following standard and a modified-accelerated collagen cross-linking protocol. Am J Ophthalmol. 2014;158(4):671–675. | ||
Kymionis GD, Diakonis VF, Kalyvianaki M, et al. One-year follow-up of corneal confocal microscopy after corneal cross-linking in patients with post laser in situ keratosmileusis ectasia and keratoconus. Am J Ophthalmol. 2009;147(5):774–778. | ||
Gokhale NS. Corneal endothelial damage after collagen cross-linking treatment. Cornea. 2011;30(12):1495–1498. | ||
Kymionis GD, Portaliou DM, Diakonis VF, Kounis GA, Panagopoulou SI, Grentzelos MA. Corneal collagen crosslinking with riboflavin and ultraviolet-A irradiation in patients with thin corneas. Am J Ophthalmol. 2012;153(1):24–28. | ||
Bagga B, Pahuja S, Murthy S, Sangwan VS. Endothelial failure after collagen cross-linking with riboflavin and UV-A: case report with literature review. Cornea. 2012;31(10):1197–1200. | ||
Sharma A, Nottage JM, Mirchia K, Sharma R, Mohan K, Nirankari VS. Persistent corneal edema after collagen cross-linking for keratoconus. Am J Ophthalmol. 2012;154(6):922–926. | ||
Spörl E, Schreiber J, Hellmund K, Seiler T, Knuschke P. Studies on the stabilization of the cornea in rabbits (in German). Ophthalmologe. 2000;97(3):203–206. | ||
Schumacher S, Oeftiger L, Mrochen M. Equivalence of biomechanical changes induced by rapid and standard corneal cross-linking, using riboflavin and ultraviolet radiation. Invest Ophthalmol Vis Sci. 2011;52(12):9048–9052. | ||
Richoz O, Hammer A, Tabibian D, Gatzioufas Z, Hafezi F. The biomechanical effect of corneal collagen cross-linking (CXL) with riboflavin and UV-A is oxygen dependent. Transl Vis Sci Technol. 2013;2(7):6. | ||
Amoozadeh J, Aliakbari S, Behesht-Nejad AH, Seyedian MA, Rezvan B, Hashemi H. Confocal microscopy of corneal stroma and endothelium after LASIK and PRK. J Refract Surg. 2009;25(10):S963–S967. | ||
Trocmé SD, Mack KA, Gill KS, Gold DH, Milstein BA, Bourne WM. Central and peripheral endothelial cell changes after excimer laser photorefractive keratectomy for myopia. Arch Ophthalmol. 1996;114(8):925–928. | ||
Cingü AK, Sogutlu-Sari E, Cinar Y, et al. Transient corneal endothelial changes following accelerated collagen cross-linking for the treatment of progressive keratoconus. Cutan Ocul Toxicol. 2014;33(2):127–1231. | ||
Bhandari V, Lohia M, Reddy JK, Haritha. Effect of accelerated corneal collagen cross linking (CXL) on corneal endothelium. Adv Ophthalmol Vis Syst. 2015;3(1):00074. | ||
Cınar Y, Cingü AK, Turkcu FM, et al. Accelerated corneal collagen cross-linking for progressive keratoconus. Cutan Ocul Toxicol. 2014;33(2):168–1671. | ||
Kanellopoulos AJ. Long term results of a prospective randomized bilateral eye comparison trial of higher fluence, shorter duration ultraviolet A radiation, and riboflavin collagen cross linking for progressive keratoconus. Clin Ophthalmol. 2012;6:97–101. | ||
Vinciguerra P, Albè E, Trazza S, Seiler T, Epstein D. Intraoperative and postoperative effects of corneal collagen cross-linking on progressive keratoconus. Arch Ophthalmol. 2009;127(10):1258–1265. | ||
Mita M, Waring GO 4th, Tomita M. High-irradiance accelerated collagen crosslinking for the treatment of keratoconus: six-month results. J Cataract Refract Surg. 2014;40(6):1032–1040. | ||
Greenstein SA, Shah VP, Fry KL, Hersh PS. Corneal thickness changes after corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011;37(4):691–700. | ||
Holopainen JM, Krootila K. Transient corneal thinning in eyes undergoing corneal cross-linking. Am J Ophthalmol. 2011;152(4):533–536. | ||
Arita R, Arita M, Kawai M, Mashima Y, Yamada M. Evaluation of corneal endothelial pump function with a cold stress test. Cornea. 2005;24(5):571–575. | ||
Mohan RR, Hutcheon AE, Choi R, et al. Apoptosis, necrosis, proliferation, and myofibroblast generation in the stroma following LASIK and PRK. Exp Eye Res. 2003;76(1):71–87. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.








