Back to Journals » Clinical Ophthalmology » Volume 17
Cooling Anesthesia for Intravitreal Injections – A Review
Authors Chandrasekaran PR , Aziz AA , Khan H, Khanani AM
Received 15 September 2022
Accepted for publication 11 November 2022
Published 13 January 2023 Volume 2023:17 Pages 197—207
DOI https://doi.org/10.2147/OPTH.S388327
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Priya R Chandrasekaran,1 Aamir A Aziz,2 Hannah Khan,2 Arshad M Khanani2,3
1Department of Medical Retina, Uvea and Neuro-Ophthalmology, Lotus Eye Hospital, Salem, Tamil Nadu, India; 2University of Nevada, Reno School of Medicine, Reno, NV, USA; 3Sierra Eye Associates, Reno, NV, USA
Correspondence: Arshad M Khanani, Email [email protected]
Abstract: Intravitreal (IVT) injections are the most common procedure performed in retinal clinics today. It has revolutionized the treatment of neovascular age-related macular degeneration (nAMD), diabetic macular edema, macular edema due to veinous occlusive disease and other forms of exudative maculopathy. Though IVT injections prevent vision loss, the discomfort at the time of the injection has been troublesome to patients. This has led to patients missing their regular and routine dosage of treatment. Various modes of pre-injection anesthetic methods have been tried but in vain. Lidocaine-based topical anesthesia, in the form of pledgets, topical gel or subconjunctival lidocaine injection, has been the standard of care (SOC) for IVT injections worldwide. This article highlights the role of cooling anesthesia in reducing pain, anxiety and discomfort associated with needle penetration at the time of injection. PubMed and MedLine search were related to anesthesia for intravitreal injections, cooling anesthesia, mechanism of cooling anesthesia, COOL-1 trial, COOL-2 trial, results of COOL-1 trial and ultrarapid cooling anesthesia.
Keywords: intravitreal injections, anesthetic methods, cooling anesthesia, COOL-1 trial, COOL-2 trial
Introduction
Intravitreal (IVT) injections are the mainstay of treatment for neovascular age-related macular degeneration (nAMD), diabetic macular edema and macular edema due to veinous occlusive disease. Patients in a survey study completed a questionnaire to grade the distress score felt during stages of IVT injection procedure. Needle entry was associated with the most anxiety among patients and was considered the most unpleasant step.1
Various methods of anesthesia have been used prior to giving IVT injections in patients. These include topical anesthetic agents (TA) in the form of drops, pledgets, gel forms and subconjunctival anesthetic agents.2 TA drops block cell membrane depolarization by reducing the cell membrane permeability of sodium ions in affected cells and thus halting pain signaling in cornea, conjunctiva and sclera. The most common TA agents that are used include proparacaine hydrochloride (HCL), tetracaine HCL and less commonly lidocaine. Formulations of tetracaine and lidocaine aims at a pH between 7.6 and 7.8 to aid in tear film penetration while proparacaine has benzalkonium chloride to aid in the same.2,3 The effect lasts for nearly 15 minutes taking effect from 15 to 20 seconds after application. TA drops cause burning sensation and long-term use leads to reduced corneal sensation causing keratitis, corneal opacity and vision loss.2,4 TA gel forms include 0.5% tetracaine HCL gel, lidocaine HCL and preservative-free lidocaine HCL gel. Gel anesthetics stay in the eye for a longer duration without getting diluted by tears unlike TA drops. Local anesthetic (LA) gel forms are well tolerated.2 However, LA gel forms were associated with high rates of endophthalmitis when given prior to povidone-iodine for IVT injections.5,6
Following application of topical anesthetics, TA pledgets are applied with pressure on the intended injection site ranging from 20 seconds to 1 minute. TA pledgets produced similar pain scores with no adverse events reported compared to other modes of anesthetic use.2,7–9 Subconjunctival injections can cause subconjunctival hemorrhages, which worsen following IVT injections. In all forms of anesthesia, the pain was well tolerated with the most distressing step being needle insertion.2
LA can be divided into Esther and amide types based on the structure of their intermediate chain. Allergy to LA is more common with the Esther group, particularly associated with the constituent methylparaben (a bacteriostatic preservative) or hyaluronidase (enhances the spread of anesthetic agent and speeds up action) or metabisulfite (a stabilizer for sympathomimetic agents) used in the anesthetic preparation.10 Periorbital allergic contact dermatitis and sight-threatening periorbital swelling due to Esther anesthetic types have been reported following peribulbar anesthesia.10,11 The metabolite p-aminobenzoic acid (PABA – from Esther anesthetics and methylparaben) is believed to be antigenic causing sensitization of T-lymphocytes and this leads to cell-mediated immunity on second exposure.10,12 The cross-reaction between Esther anesthetic group and methylparaben can cause anaphylaxis due to cross-reaction and hence preservative free amide group anesthetic can be used.10,13
Table 1 shows results of studies using various anesthetic modalities for intravitreal injections.
 |
Table 1 Results of studies using various anesthetic modalities for intravitreal injections |
This review article addresses the need for such an anesthetic that will lessen patient’s anxiety at the most crucial step and reduce pain score. Hence, cooling anesthesia might mitigate the above concerns of the patient and prove to be effective. Figure 1 shows RecensMedical cooling device utilized for IVT treatment. This review highlights the results and advantages from the trials so far.
 |
Figure 1 OCU-COOL® Cooling ocular anesthetic device utilized for intravitreal injection treatment for retinal diseases. Image courtesy of RecensMedical. |
Method of Literature Search
PubMed and MedLine searches were utilized to find articles related to anesthesia for intravitreal injections, cooling anesthesia, mechanism of cooling anesthesia, COOL-1 trial, COOL-2 trial, results of COOL-1 trail and Ultrarapid cooling anesthesia.
Ultra-Rapid Non-Pharmacological Cooling Anesthesia for IVT Injections (NCT02872012)
This open-label randomized interventional study assessed to the effectiveness of cooling anesthesia (CA) prior to IVT injections. This study used a hand-held CA device given to a focal area to reduce pain caused by IVT injections. It is a portable device with a single-use disposable tip utilizing thermoelectric cooling to a 4mm × 4mm area on the surface of the eye. Twenty-two patients (44 eyes) were randomly given ultra-rapid CA with various temperatures at different time points in one eye and SOC lidocaine in the fellow eye prior to IVT injection.23,24
The CA group was divided into 5 arms:
- -5 °C for 10 seconds
- -5 °C for 20 seconds
- -7 °C for 20 seconds
- -10 °C for 10 seconds
- -10 °C for 20 seconds
The primary outcome was to measure subjective pain at the time of IVT injection using a visual analog scale (VAS) which ranged from 0 to 10, with zero being no pain and 10 being severe pain.23,24
The secondary outcome was to measure post injection pain and discomfort 4 hours after IVT injection and adverse events as reported by the patients 7 days after the injection.23,24
- All sexes more than 18 years of age.
- Bilateral disease of the macula either due to diabetic macular edema or exudative macular degeneration.
- Those who received at least 1 previous IVT injection.
- Those who were willing to give informed consent.
- Unilateral macular disease.
- Those who were not willing to give informed consent.
- Those who had preexisting episcleral, scleral or conjunctival defects.
The Procedure
Before the beginning of the actual procedure, proparacaine drop was instilled into the eye. In the SOC anesthesia arm, 3 sets of cotton-tipped pledgets containing 4% lidocaine for 1 to 2 minutes with each set was placed in the eye or 3.5% lidocaine gel was placed for 3 minutes. Eyelid speculum was placed after cleaning the eyelids and betadine was applied to the conjunctival area for nearly 15 seconds. Before administering the injection, 3mm to 4mm from the limbus, betadine was applied for another 15 seconds.24
In the CA arm, proparacaine was instilled prior to procedure. Betadine was applied after placing the lid speculum for nearly 15 seconds and CA device was placed after checking the desired temperature for each patient and using a timer. IVT injection was given after confirming a distance of 3mm to 4mm from the limbus and after application of another drop of betadine to the injection site. The procedural time frame was recorded for each patient. Paired t-test was used to compare the means between the eyes, standard error of the mean (SEM) and range were used for mean and a p-value <0.05 was considered statistically significant.24
For the primary outcome, pain was assessed using VAS:
- Immediately after the injection
- 4 hours after injection24
For the secondary outcome, biomicroscopic examination was done:
- Before the injection
- Within 30 minutes of receiving the injection
- 24 hours after the injection
- At 7 days after the injection24
The ocular side effects that were looked for using biomicroscopic examination:24
- Subconjunctival hemorrhage (SCH)
- Conjunctival hyperemia
- Conjunctival injection
- Corneal keratopathy
- Anterior chamber reaction
- Hypotony
Table 2 gives details of grading of ocular side effects.24
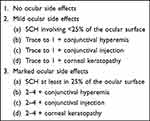 |
Table 2 Grading of ocular side effects as used in the study24 |
Results
The mean age of patients in the study was 71 years, of which 73% were females and 27% were males. IVT were given for both exudative age-related macular degeneration and diabetic macular edema and both aflibercept and bevacizumab were given. The mean number of intravitreal injections given previously was 29.24
There were no ocular side effects in 68% of the CA group and 56% of the SOC group, minimal side effects were observed in 32% of the CA group and 44% of the SOC group in 24 hours. Severe or marked side effects were not found in any patient in either group in 24 hours.24
Patients that were followed after day 7 in both groups did not report any adverse events.
Table 3 gives details of the pain scores at the time of injection in both CA and SOC groups. SOC eyes were grouped with the fellow eyes receiving CA and were randomized to each CA dosage group.24
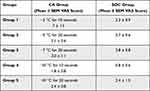 |
Table 3 Details of the Pain Scores at the Time of Injection in Both CA and SOC Groups. SOC Eyes Were Grouped with the Fellow Eyes Receiving CA and Were Randomized to Each CA Dosage group24 |
Pain control was similar in both SOC and CA groups from duration 2–5 (−5°C for 20 seconds to −10°C for 20 seconds, P = 0.3 – > 0.9). The mean ± SEM difference of injection pain in both the groups with the duration of – 5°C for 10 seconds was the largest (4.7 ± 1.8) but was not statistically significant (P = 0.1). Mean ± SEM VAS scores for the combined SOC arms after IVT injection was 2.3 ± 0.4 and that of CA groups 4 and 5 was 2.2 ± 0.6.24
Table 4 gives details of the pain scores 4 hours after IVT in SOC and CA groups.24
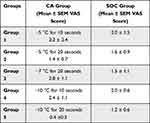 |
Table 4 Details of the Pain Scores 4 Hours After IVT in SOC and CA groups24 |
Within each group, post-injection pain scores measured 4 hours after IVT injection were similar between CA within each group and SOC groups (P = 0.3–0.8). The mean ± SEM for combined SOC arms and combined –10°C. A 4 hours post IVT injection were 1.6 ± 0.4 and 1.2 ± 0.5 (P = 0.56), post-injection pain score in group 5 (−10°C for 20 seconds) in CA was the least, mean ± SEM post-injection pain score difference between combined SOC (n = 22) and group 5 of CA (n = 5) was 1.2 ± 0.5 that was statistically significant (P = 0.02), mean ± SEM IVT injection time was 395 ± 40 seconds in those in SOC and that of CA was 124 ± 5 seconds (P < 0.0001).24
COOL-1 Trial (NCT03732287) – RecensMedical
The purpose of this study was to evaluate the safety and efficacy of cooling anesthesia for IVT injections using a novel device. The study also evaluated the effects of temperature and duration of application on subjective pain after the injection. This was a non-randomized, open-label intervention trial that had 3 arms, listed below.25,26
The primary outcome measure was to assess subjective pain (24 to 48 hours after the injection) using a Numeric Rating Scale (NRS), the range being 0 to 10, 0 being the least and 10 being severe/unbearable pain and adverse events as measured by complete slit-lamp examination (both anterior and posterior segment examination after 30 minutes of having the injection).25,26
The secondary outcome measure was to measure the response of the patient to needle penetration during IVT injection and the time taken from the beginning of anesthesia to IVT injection.25,26
The inclusion criteria include:26
- Men and women >18 years old.
- Those who are undergoing IVT injections in one or both eyes with ranibizumab or aflibercept using a 30-gauge needle as part of their normal standard of care.
- Those who have received a minimum of 3 IVT injections before the study.
- Those who are willing and signing the written informed consent form.
The exclusion criteria include:26
- Presence of scleromalacia.
- Presence of conjunctival, episcleral or scleral defects.
- Less than 18 years of age.
- Not willing to give informed consent.
- Received less than 3 injections in the study eye.
- Dry eye disease not responding to artificial tears but requiring cyclosporine drops or other prescription drugs.
- History of endophthalmitis following injection in the past.
- History of uveitis, vitrectomy or retinal detachment in either eye.
COOL-1 Study
This prospective, open-label and dose-escalation study used a handheld precision cooling device to evaluate its safety. The study used three ascendent doses of the cooling anesthesia device (CAD):
- -10°C for 20 seconds.
- -15°C for 15 seconds.
- -15°C for 20 seconds and it was a single-visit dose-escalation study. Each study of two study sites assessed 2/3 treatment doses, with a common dose of −10°C for 20 seconds between the two sites.25,26
After getting consent, patients were assessed for pain score of 0 to 10.
- At the time of injection and 5 minutes after intravitreal injection.
- Slit-lamp biomicroscopy and indirect ophthalmoscopy 30 ± 15 minutes after the injection for adverse effects.
- Phone call after 24 to 48 hours after the injection to assess the pain.25,26
The Procedure
The procedure included application of 0.5% proparacaine to the injection site at the corneal limbus after applying speculum or manual opening of lids and betadine to the conjunctival surface. Scleral indentation was noted after applying the cooling device adjacent to the corneal limbus. Intravitreal injection was applied to the scleral indentation area 30 seconds after applying the cooling device and using a 30-gauge ½ inch needle. The device used was a reusable hand-held battery device after obtaining regulatory The precision of the device was close to ± 2°C. The cooling temperature of the device did not change even after 1000 uses between 10°C and 27°C.26
The injection procedure included application of 0.5% proparacaine as the initial step followed by lid speculum or manual opening of the lids, application of betadine to the injection site, cooling device placement adjacent to corneal limbus for 10 to 20 seconds and wait for transient scleral indentation, giving IVT injection within the scleral indentation area and within 30 seconds of giving anesthesia using a 30-gauge ½ inch needle after second application of betadine.26
Results
The study comprised 55.8% (24) men and 44.2% (19) women whose mean age at screening was 70.8 ± 13.8. Patients received IVT for neovascular age-related macular degeneration, vein occlusion, diabetic macular edema and diabetic retinopathy. The mean number of previous injections was 22.6 ± 12.7.26
As far as the safety profile is concerned, one patient experienced a grade 1 adverse event (Common Terminology Criteria for Adverse Events) in group 5 (−10°C for 20 seconds), which was a vasovagal response most likely due to the cooling event and resolved without treatment. There was no other ocular adverse event (conjunctival or scleral thinning, corneal abrasion or endophthalmitis) or any serious adverse events.26
The mean ± SD NRS pain score during the application of CA was 2.7 ± 2.15 in -100C for 20 seconds group, 2.75 ± 1.64 in – 150C for 15 seconds group and 3.89 ± 3.0 in – 150C for 20 seconds group respectively. The mean ± SD NRS pain score at the time of IVT was 3.7 ± 2.5 in -100C for 20 seconds group, 2.5 ± 1.7 in – 150C for 15 seconds group and 4.3 ± 1.8 in – 150C for 20 seconds group respectively with P = 0.13. The mean ± SD NRS pain score 5 minutes after injection was 1.2 ± 1.3 in -100C for 20 seconds group, 1.2 ± 2.1 in – 150C for 15 seconds group and 1.1 ± 1.1 in – 150C for 20 seconds group respectively with P = 0.27. The mean ± SD NRS pain score 24-48 hours after the IVT was 0.1 ± 0.3 in -100C for 20 seconds group, 0.6 ± 1.4 in – 150C for 15 seconds group and 0.1 ± 0.4 in – 150C for 20 seconds group respectively with P = 0.53.26
There was no statistically significant difference pairwise at the time of injection in the groups but significant difference among the 3 groups in aggregate (P = 0.047) at the time of injection, no statistical difference 5 minutes and 24 to 48 hours post-injection among the groups (0.676 and 0.32 respectively). P values were 0.13, 0.27 and 0.53, respectively, in all three groups at the time of injection, 5 minutes and 24–48 hours post IVT injection, statistically significant pain scores at the time of injection and 5 minutes post injection (P =0.00008, 0.003 and 0.005, respectively) in groups −10°C for 20 seconds, - 15°C for 15 seconds and −15°C for 20 seconds, statistically significant difference in the 5 minutes post-injection and in −10°C for 10 seconds and –15°C for 15 seconds only (P = 0.00001, 0.018 respectively). Average procedural time was 2.05 minutes with an SD of 1.75 minutes.26
COOL-2 Trial (NCT03956797) – RecensMedical
This study was designed to evaluate the long-term safety and efficacy of cooling anesthesia for IVT using a CAD for macular degeneration (51%), diabetic macular edema (28%), macular edema due to veinous occlusive disease (19%) and myopic choroidal neovascularization (2%). This is a completed, non-randomized, open-label, interventional dose–escalation study using differing temperatures and duration to assess the long-term safety and efficacy of cooling anesthesia over a series of six injections.27–29
In the first arm, the CAD at −15°C was applied for 10 seconds and in the other arm, the CAD at −15°C was applied for 15 seconds.
The primary outcome measure was to measure pain using a visual analog scale (VAS) with 0 being least and 10 being most severe pain.
The secondary outcome was to look for27–29
- Patient movement during injection and particularly during needle penetration (1 - mild movement and 2 - marked movement).
- Time taken to perform the entire IVT procedure.
- Anesthetic preference by the patient by the end of 24 to 48 hours – standard of care or cooling anesthesia.
- Pain during follow-up – 24 to 48 hours after IVT injection using VAS score.
The inclusion criteria27–29
- Men and women >18 years old.
- Those who are undergoing IVT injections in one or both eyes with ranibizumab or aflibercept using a 30-gauge needle as part of their normal standard of care.
- Those who have received a minimum of 3 IVT injections before the study.
- Those who are willing and signing the written informed consent form.
The exclusion criteria include27–29
- Presence of scleromalacia.
- Presence of conjunctival, episcleral or scleral defects.
- Less than 18 years of age.
- Not willing to give informed consent.
- Received less than 3 injections in the study eye.
- Dry eye disease not responding to artificial tears but requiring Restasis or other prescription drugs.
- History of endophthalmitis following injection in the past.
- History of uveitis, vitrectomy or retinal detachment in either eye.
- Those who participated in COOL-1 trial are also eligible to participate in the study.
Table 5 gives the interim results.27–29
 |
Table 5 The Interim results27–29 |
Discussion
Use of IVT injections for various retinal diseases have increased exponentially in the last few years. Various theories of freeze damage have been speculated to be due to hypertonicity of intra- and extracellular fluids, physical destruction at the site by the extracellular ice crystals, attainment of minimum cell volume, cell protein damage, rapid water loss leading to membrane rupture, ischemic necrosis and production of autoantibodies predominantly in vitro. It has been shown that cryo causes complete tissue destruction at the center where there is recovery in the periphery. Reversible conduction block happens when cold is applied to peripheral nerves either by direct cooling of few segments or complete immersion of the entire tissue. This in turn is dependent upon the duration of exposure and the temperature attained in the tissues. There is breakdown of myelin sheath with disintegration of axons and Wallerian degeneration occurs with perineurium and epineurium remaining intact. Nerve regeneration not only depends on the temperature reached but also on the degree of hypoxia, buildup of metabolites, histamine release and its action and finally inactivation of enzymes due to cold exposure. The reappearance of sensory and motor activity is dependent on the rate of nerve regeneration and the distance between cryo lesion and end organ. Studies have speculated the temperature drop to −20°C for adequate pain relief that produces only a brief interruption of conduction of nerve impulses.30
Various factors are associated with increased pain score during intravitreal injections including being female, patients not undergoing anterior chamber paracentesis and those who had more waiting time.31
Several studies have shown the size of the needle influences pain during IVT injection, whereas few studies have indicated small needle size is associated with less pain. Other studies found no association between pain and needle size. Beveled incisions caused decrease reflux and 29-gauge and 30-gauge needles reduced pain.32 Other studies found no association between pain 29-gauge and 30-gauge needles and pain.33 Advantages such as scleral damage and reduced vitreous reflux, but no pain reduction, were seen with 33-gauge needles. Other factors are believed to cause more pain than the actual size of the needle.34
Moisseiev et al evaluated correlation between pain associated with bevacizumab injection given for age-related macular degeneration, macular edema due to diabetic retinopathy and vein occlusions and neovascularization due to proliferative diabetic retinopathy and its location site and observed that there was no correlation between patient age, number of injections, sex, different indications, and pain scores. Pain scores were analyzed in superior, inferior, temporal, and nasal quadrants. Pain scores were also analyzed by further grouping them into superonasal and superotemporal quadrants in each eye and inferonasal and inferotemporal quadrants in each eye. This in turn was categorized into upper right, upper left lower right and lower left quadrants. The mean pain score was 17.4 ± 17.1 and there was a decrease in pain score in the inferonasal and lower left quadrants.35 The same authors evaluated the pain score between dexamethasone and bevacizumab injections and observed that the mean pain score was 20.8 ± 20.3. There was no correlation between pain scores and patient sex, number of injections or indications for injections or between dexamethasone (P=0.837 for DME and P=0.304 for ME due to vein occlusions) and bevacizumab injections. However, higher VAS scores were seen in older patients (P=0.017) and pseudophakic eyes (32.3 ± 23.0 vs 15.6 ± 16.8, P=0.005).36 Massamba et al evaluated pain score using ranibizumab and observed that the pain scores were higher in the left eye and in the superior temporal quadrant and there was no correlation between pain scores and age, sex, or indications.37
Smith et al performed ultra-rapid focal cooling of rabbit eyes at temperatures between +20°C and –40°C on a 4mm × 4mm surface area for 10 seconds and 30 seconds and in all quadrants, with 1 treatment in each quadrant. There were no histopathological signs of ocular toxicity at –30°C for 30 seconds but mild occasional limbal inflammation at −35°C and −40°C, respectively.38 Besirli et al in his study showed that those receiving CA for −10°C had results comparable to SOC than the first three groups where −5°C and −7°C caused generation of intrinsic heat that may have caused incomplete anesthetic effect. The authors concluded that colder temperatures and longer duration produced anesthetic effect comparable to SOC.24
The COOL-1 study showed that there was no statistical difference in pain scores among groups at the time of injection, 5 minutes after injection and 24–48 hours later. The use of single drop of topical 0.5% proparacaine used before placing the CA device added additional benefit by anesthetizing the ocular surface initially and paving way for rapid and adequate anesthetic effect for the injection. This is considered much faster than other types of anesthesia for IVT such as lidocaine gel or subconjunctival lidocaine. However, the confounding contribution from topical 0.5% proparacaine towards the NRS pain scores cannot be overlooked.26 These findings were consistent with reduced pain scores following prolonged duration of exposure (12 minutes with topical tetracaine gel or 6 minutes with subconjunctival lidocaine).39
Conclusion
Cooling anesthesia may provide an efficient, efficacious, and safe anesthesia strategy prior to intravitreal injections. Multiple early-stage trials have clearly shown the potential of cooling anesthesia prior to intravitreal injections for retinal diseases. These results have so far shown that cooling anesthesia would mitigate the pain, apprehension and possibly hypersensitivity or anaphylaxis associated with certain groups and compounds used as additives. However, further randomized controlled trials are required to prove the efficacy and safety of cooling anesthesia compared to the current standard of care anesthetic strategies for patients undergoing intravitreal injections.
Disclosure
This review is not supported by RecensMedical. Dr. Khanani is a consultant for RecensMedical and has equity in the company. There is no bias for any cooling technology as this is just a review. The authors report no other conflicts of interest in this work.
References
1. Tailor R, Beasley R, Yang Y, Narendran N. Evaluation of patients’ experiences at different stages of the intravitreal injection procedure - what can be improved? Clin Ophthalmol. 2011;5(5):1499–1502. doi:10.2147/OPTH.S24358
2. Han J, Rinella NT, Chao DL. Anesthesia for intravitreal injection- A systematic review. Clin Ophthalmol. 2020;14(14):543–550. doi:10.2147/OPTH.S223530
3. Page MA, Fraunfelder FW. Safety, efficacy, and patient acceptability of lidocaine hydrochloride ophthalmic gel as a topical ocular anesthetic for use in ophthalmic procedures. Clin Ophthalmol. 2009;3(3):601–609. doi:10.2147/opth.s4935
4. Bryant JS, Busbee BG, Reichel E. Overview of ocular anesthesia: past and present. Curr Opin Ophthalmol. 2011;22(3):180–184. doi:10.1097/ICU.0b013e328345974c
5. Miller JJ, Scott IU, Flynn HW Jr, Smiddy WE, Newton J, Miller D. Acute-onset endophthalmitis after cataract surgery (2000–2004): incidence, clinical settings, and visual acuity outcomes after treatment. Am J Ophthalmol. 2005;139(6):983–987. doi:10.1016/j.ajo.2005.01.025
6. Boden JH, Myers ML, Lee T, Bushley DM, Torres MF. Effect of lidocaine gel on povidone-iodine antisepsis and microbial survival. J Cataract Refract Surg. 2008;34(10):1773–1775. doi:10.1016/j.jcrs.2008.05.056
7. Yau GL, Jackman CS, Hooper PL, Sheidow TG. Intravitreal injection anesthesia–comparison of different topical agents: a prospective randomized controlled trial. Am J Ophthalmol. 2011;151(2):333–337. doi:10.1016/j.ajo.2010.08.031
8. Blaha GR, Tilton EP, Barouch FC, Marx JL. Randomized trial of anesthetic methods for intravitreal injections. Retina. 2011;31(3):535–539. doi:10.1097/IAE.0b013e3181eac724
9. Davis MJ, Pollack JS, Shott S. Comparison of topical anesthetics for intravitreal injections: a randomized clinical trial. Retina. 2012;32(4):701–705. doi:10.1097/IAE.0b013e31822f27ca
10. Dance D, Basti S, Koch DD. Use of preservative-free lidocaine for cataract surgery in a patient allergic to “caines”. J Cataract Refract Surg. 2005;31(4):848–850. doi:10.1016/j.jcrs.2004.09.059
11. Walters G, Georgiou T, Hayward JM. Sight-threatening acute orbital swelling from peribulbar local anesthesia. J Cataract Refract Surg. 1996;25(3):444–446. doi:10.1016/S0886-3350(99)80097-2
12. Eggleston ST, Lush LW. Understanding allergic reactions to local anesthetics. Ann Pharmacother. 1996;30(7–8):851–857. doi:10.1177/106002809603000724
13. Balestrieri P, Ferguson JE 2nd. Management of parturient with a history of local anesthetic allergy. Anesth Analg. 2003;95(50):1489–1490. doi:10.1213/01.ANE.0000058843.24914.C7
14. Kozak I, Cheng L, Freeman WR. Lidocaine gel anesthesia for intravitreal drug administration. Retina. 2005;25(8):994–998. doi:10.1097/00006982-200512000-00007
15. Sanabria MR, Montero JA, Losada MV, et al. Ocular pain after intravitreal injection. Curr Eye Res. 2013;38(2):278–282. doi:10.3109/02713683.2012.758290
16. Rifkin L, Schaal S. Factors affecting patients’ pain intensity during in office intravitreal injection procedure. Retina. 2012;32(4):696–700. doi:10.1097/IAE.0b013e3182252ad3
17. Ornek N, Apan A, Ornek K, Gunay F. Anesthetic effectiveness of topical levobupivacaine 0.75% versus topical proparacaine 0.5% for intravitreal injections. Saudi J Anaesth. 2014;8(2):198–201. doi:10.4103/1658-354X.130713
18. Friedman SM, Margo CE. Topical gel vs subconjunctival lidocaine for intravitreous injection: a randomized clinical trial. Am J Ophthalmol. 2006;142(5):887–888. doi:10.1016/j.ajo.2006.06.033
19. Karabas VL, Ozkan B, Kocer CA, Altintas O, Pirhan D, Yuksel N. Comparison of two anesthetic methods for intravitreal ozurdex injection. J Ophthalmol. 2015;2015:861535. doi:10.1155/2015/861535
20. Kaderli B, Avci R. Comparison of topical and subconjunctival anesthesia in intravitreal injection administrations. Eur J Ophthalmol. 2006;16(5):718–721. doi:10.1177/112067210601600
21. Andrade GC, Carvalho AC. Comparison of 3 different anesthetic approaches for intravitreal injections: a prospective randomized trial. Arq Bras Oftalmol. 2015;78(1):27–31. doi:10.5935/0004-2749.20150008
22. Shiroma HF, Nunes RP, Farah ME, et al. Safety and efficacy of various concentrations of topical lidocaine gel for intravitreal injection. Expert Opin Drug Saf. 2014;13(10):1299–1303. doi:10.1517/14740338.2014.947261
23. Cryo anesthesia for intravitreal injections. Available from: https://clinicaltrials.gov/ct2/show/NCT02872012.
24. Besirli CG, Smith SJ, Zacks DN, et al. Randomized safety and feasibility trial of ultra-rapid cooling anesthesia for intravitreal injections. Ophthalmol Retina. 2020;4(10):979–986. doi:10.1016/j.oret.2020.04.001
25. Cooling anesthesia for intravitreal injection (COOL-1). Available from: https://clinicaltrials.gov/ct2/show/NCT03732287.
26. Chao DL, Rinella NT, Khanani AM, Wykoff CC, Kim GH. Cooling anesthesia for intravitreal injection: results of the prospective open-label dose-ranging COOL-1 trial. Clin Ophthalmol. 2021;10(15):4659–4666. doi:10.2147/OPTH.S336653
27. Long term safety of cooling anesthesia for intravitreal injection (COOL-2). Available from: https://clinicaltrials.gov/ct2/show/NCT03956797.
28. Long term safety of cooling anesthesia for intravitreal injection (COOL-2). Available from: https://ichgcp.net/clinical-trials-registry/NCT03956797.
29. Dalton, M. Cooling Anesthesia a Safe, Effective Alternative to Subconjunctival Lidocaine Modern Retina. Available from: https://www.modernretina.com/view/cooling-anesthesia-a-safe-effective-alternative-to-subconjunctival-lidocaine.
30. Evans PJD. Cryoanalgesia – the application of low temperatures to nerves to produce anesthesia or analgesia. Anesthesia. 1981;36(11):1003–1013. doi:10.1111/j.1365-2044.1981.tb08673.x
31. Shin SH, Park SP, Kim YK. Factors associated with pain following intravitreal injections. Korean J Ophthalmol. 2018;32(3):196–203. doi:10.3341/kjo.2017.0081
32. Rodrigues EB, Grumann A, Penha FM, et al. Effect of needle type and injection technique on pain level and vitreous reflux in intravitreal injection. J Ocul Pharmacol Ther. 2011;27(2):197–203. doi:10.1089/jop.2010.0082
33. Haas P, Radler CF, Wimpissinger B, Malina M, Binder S. Needle size in intravitreal injections – pain evaluation of a randomized clinical trial. Acta Ophthalmol. 2016;94(2):198–202. doi:10.1111/aos.12901
34. Asten FV, Middendorp HV, Verkerk S, et al. Are intravitreal injections with ultrathin 33-g needles less painful than the commonly use 30g needles? Retina. 2015;35(9):1778–1785. doi:10.1097/IAE.0000000000000550
35. Moisseiev E, Regenbogen M, Bartfeld Y, Barak A. Evaluation of pain in intravitreal bevacizumab injections. Curr Eye Res. 2012;37(9):813–817. doi:10.3109/02713683.2012.681335
36. Moisseiev E, Regenbogen M, Rabinovitch T, Barak A, Lowenstein A, Goldstein M. Evaluation of pain during intravitreal ozurdex injections vs intravitreal bevacizumab injections. Eye. 2014;28(8):980–985. doi:10.1038/eye.2014.129
37. Massamba N, Elluard M, Agoune W, et al. Assessment of ocular pain following ranibizumab intravitreal injection. Acta Ophthalmol. 2015;93(3):e231–232. doi:10.1111/aos.12531
38. Smith S, Kim G, Pipe KP, Besirli C. Preclinical safety study of ultra-rapid non-pharmacologic anesthesia for intravitreal injections. ARVO annual meeting abstract July 2018; 2018. Available from: https://iovs.arvojournals.org/article.aspx?articleid=2690581.
39. Cohen SM, Billiris-Findlay K, Eichenbaum DA, Pautler SE. Topical lidocaine gel with and without subconjunctival lidocaine injection for intravitreal injection: a within-patient study. Ophthalmic Surg Lasers Imaging Retina. 2014;45(4):306–310. doi:10.3928/23258160-20140709-06
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
