Back to Journals » Clinical Ophthalmology » Volume 15
Contralateral Eye Study of Topography Guided versus Q Value Adjusted Photorefractive Keratectomy in Myopia and Myopic Astigmatism
Authors Gad RE , Hosny M , Ahmed RA, Sherif AM , Salah Eldin Y
Received 3 January 2021
Accepted for publication 15 March 2021
Published 23 April 2021 Volume 2021:15 Pages 1735—1749
DOI https://doi.org/10.2147/OPTH.S300232
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Rania E Gad,1 Mohamed Hosny,2 Rania A Ahmed,2 Ahmed M Sherif,2 Yehia Salah Eldin2
1Ophthalmology Department, Helwan University, Cairo, Egypt; 2Ophthalmology Department, Cairo University, Cairo, Egypt
Correspondence: Rania E Gad
Department of Ophthalmology, Helwan University, Ain Helwan, PO Box 11795, Cairo, Egypt
Email [email protected]
Purpose of the Study: To compare visual outcome, higher order aberrations (HOAs) of topography guided and Q value adjusted ablation in the fellow eye of patients undergoing photorefractive keratectomy (PRK) for the correction of myopia and myopic astigmatism.
Methods: Prospective randomized controlled interventional clinical study. The eyes of 52 patients undergoing PRK for myopia and astigmatism were included, that is, 104 eyes in total. In each patient, eyes were randomly allocated to group I: one eye received topography guided PRK using Contoura ablation software, or group II: the other eye received Q value adjusted PRK using Custom Q ablation software.
Follow-Up: Six months.
Results: At the end of 6 months, LogMAR UDVA was − 0.04 ± 0.12 and − 0.05 ± 0.11 (p = 0.688), while LogMAR CDVA was − 0.06 ± 0.09 and − 0.06 ± 0.1 in group I and group II, respectively (p = 0.972). Both groups showed a progressive oblate shift with time. This oblate shift was insignificantly less in group I by Topolyzer at 6mm, 15° and 30° at 6 months (p = 0.102, p = 0.138, p = 0.245, respectively). Topolyzer identified a significant difference between the change in coma and trefoil in both groups at 6 months (p< 0.001 and p = 0.001, respectively). This was caused by the significant worsening of coma in group II (p< 0.001) and the significant improvement of trefoil in group I (p = 0.007). No significant difference was found between groups in the change of ISV or ABR (p = 0.955 and 0.982, respectively). Ablation depth is a significant predictor of ΔQ at 6mm, 15° and 30° (p = 0.009, 0.039 and 0, respectively). No significant difference was found in the Strehl ratio or contrast sensitivity, although they were insignificantly better in group I (p = 0.785 and p = 0.745, respectively).
Conclusion: TG PRK and CQ PRK yielded similar results regarding UDVA, CDVA, MRSE, safety, predictability and contrast sensitivity. Both groups showed a progressive oblate shift, which was less in the TG group but the difference was statistically insignificant. TG PRK showed significantly improved trefoil HOA as compared to CQ PRK.
Keywords: topography, Q value, photorefractive keratectomy, myopia, astigmatism
Introduction
Conventional excimer laser ablation patterns used in the correction of myopia and/or astigmatism can reduce quality of vision that is attributed to the induced optical aberrations. Spherical aberration, caused by the oblate shift, seems to be the most prevalent of these optical aberrations. Therefore, aspheric ablation profiles and wavefront analysis were studied in an attempt to minimize the induced optical aberrations.1,2
The Q value is a shape factor used to characterize the amount of corneal asphericity numerically and its importance was described in earlier studies on PRK.3 The Custom Q ablation allows the surgeon to define the target Q factor. The only pre-operative data this treatment needs, other than the patient’s refraction, is the mean corneal asphericity.4
On the other hand, topography guided ablation reshapes the corneal irregularities into an ideal curve. Hence, it is primarily used to treat irregular astigmatism in post-LASIK eyes.5,6 However, it has also proven its safety and efficacy in myopia and astigmatism in virgin corneas.7
In this study, topography guided PRK, a customized ablation based on corneal topography, is compared to Custom Q PRK, a non-individualized aspheric treatment.
Patients and Methods
This study was a prospective randomized controlled clinical study. In each patient, one eye was randomly assigned for topography-guided (TG) PRK (group I) and the other for custom-Q (CQ) PRK (group II) for correction of myopia and/or astigmatism. Simple randomization was done.
This study was conducted following approval by the Research Ethics Committee, Cairo University, Faculty of Medicine (N-85-2017) and within the tenets of the Declaration of Helsinki (clinical trials registration ID [NCT03291873] at clinicaltrials.gov). Written informed consent was obtained from each subject undergoing the procedure and stated that their unidentified data will be used for scientific publication.
Patients were included in this study if they were over 18 years of age with stable myopia (up to −6.5) with or without astigmatism (up to −4.75). Exclusion criteria were previous refractive surgery, established or forme-fruste keratoconus, macular or retinal disease, autoimmune disease, pregnancy and lactation.
The preoperative examination for each patient included UDVA, CDVA, manifest and cycloplegic refraction, slit lamp biomicroscopy, tonometry and dilated fundoscopy. Corneal tomography was performed using a CSO Sirius Scheimpflug camera combined with Placido corneal topography (CSO, Florence, Italy). Three high quality scans were obtained.
Corneal topography using a Topolyzer Vario (Wavelight AG, Erlangen, Germany) was performed on all patients preoperatively. At least 4, and up to 8, good quality images were taken of each eye. Repeatability of the Topolyzer and Sirius images was considered acceptable with a coefficient of variance of ≤ 1% and reliable with an intraclass correlation coefficient (ICC) of ≥0.8.
In group I, the topography maps, together with pupil size and position, were exported to the T-CAT Contoura software (Wavelight AG, Erlangen, Germany). The amount and axis of the cylinder used were determined by manifest refraction and not the topographic cylinder.
In group II, the manifest refraction data was used and Custom Q software (Wavelight AG, Erlangen, Germany) was used to plan the treatment.
The target Q was set according to a nomogram considering the patient’s age: a target Q of −0.46 for patients older than 35 years, a target Q of −0.4 for patients 30 to 35 years and a target Q of −0.3 for patients younger than 30. In some eyes where the preoperative Q (obtained from the Topolyzer images) was more negative (more prolate corneas) than the target Q, the target Q was left the same as preoperatively.
No adjustment of sphere was done in either group.
Operative Steps
The operating surgeon for all cases was one of two (YS or MH). The epithelium was removed using a blunt spatula followed by ablation utilizing the Alcon/Wavelight EX 500 platform (Wavelight AG, Erlangen, Germany). Mitomycin C 0.02% was used in all eyes. Topical steroids were tapered gradually over the period of one month while topical lubricants were used for 3 months.
Fifty-eight patients were enrolled in this study. Only in 53 patients were good quality, reproducible images obtained by the Topolyzer. In the 5 patients who failed to obtain reproducible topography maps, both eyes underwent CQ PRK and were excluded.
In one patient from the TG group, postoperative images on all visits were of poor quality; therefore, this patient was excluded. Fifty-two patients (104 eyes) were followed up for 6 months.
Follow-Up
Postoperatively, UDVA, CDVA and corneal topography using Topolyzer were assessed on each visit, at 1, 3 and 6 months. The Topolyzer measured the Q value of the anterior corneal surface through a 6mm aperture on the cornea and at 15° and 30°degrees peripherally from the corneal apex. ΔQ is the difference between postoperative Q and preoperative Q. Aberration coefficients of astigmatism, coma, trefoil and spherical aberrations were measured by the Topolyzer. The aberration coefficient (ABR) was calculated from the Zernike analysis output of the Topolyzer. If there are no abnormal corneal aberrations, ABR is 0; otherwise, ABR becomes 1.0 or greater. The index of surface variance (ISV) measured by the Topolyzer gives the deviation of individual corneal radii from the mean value. It is elevated in all types of irregularity of the corneal surface (≥37 abnormal, ≥41 pathological).
Total RMS, RMS astigmatism, RMS coma, RMS spherical aberrations and Strehl ratio (the ratio between the peak luminous intensity of the point spread function (PSF) of the optical system under examination and the peak generated by a flat wavefront through the same pupil − the ratio decreases as the aberration increases) were measured using CSO Sirius tomography (CSO, Florence, Italy) at 1, 3 and 6 months.
To assess quality of vision, contrast sensitivity using the Cambridge low contrast sensitivity chart was tested at 6 months.
Primary outcomes included UDVA, CDVA, refractive cylinder and MRSE at 1, 3 and 6 months. The change in Q value (6mm, 15°and 30°) and the change in higher order aberrations (HOAs) were identified by the Topolyzer.
Secondary outcomes included: correlation of ΔQ in the CQ group with preoperative Q, target Q, change in Q, K1, K2, age and ablation depth. Change in Q at 6mm, total RMS, RMS astigmatism, RMS coma and RMS spherical aberrations were measured by corneal tomography using a Sirius Scheimpflug camera (CSO, Florence, Italy) and assessment of quality of vision.
Statistical Analysis
SPSS (Statistical Package for the Social Sciences) version 26 (IBM Corp., Armonk, NY, USA) was used. Comparisons between quantitative variables were done using the non-parametric Mann–Whitney test. For comparison of serial measurements within each patient, the non-parametric Friedman test and Wilcoxon signed rank test were used. Comparisons between quantitative variables were done using the non-parametric Kruskal–Wallis and Mann–Whitney tests.
Correlations between quantitative variables were done using Spearman's correlation coefficient. Linear regression analysis was done to detect independent predictors of ΔQ. An exact test was used instead when expected frequency was less than 5. P-values of ˂0.05 were considered statistically significant.
Results
This study included 52 patients – 24 males (46.2%) and 28 females (53.8%). The mean age of the patients was 26.71 ± 6.75 years (range: 18–43 years). Demographic data and surgical eyes are shown in Table 1.
 |
Table 1 Age, Gender and Surgical Eyes in Both Groups |
At one-month follow-up, all 52 patients (100%) presented; 92.3% of patients from the TG group (48/52) and 90.3% of patients from the CQ group (47/52) completed the 6-month follow-up. (One patient had enhancement in the CQ adjusted eye two months after surgery and was thus excluded from the 3- and 6-month follow-ups.)
There was no statistically significant difference between the 2 groups in terms of preoperative pachymetry, K1, K2, Q value, sphere or cylinder, as shown in Table 2.
 |
Table 2 Preoperative Topographic and Refractive Data in the 2 Groups |
In the TG group, the mean difference between the measured topographic cylinder and the refractive cylinder in axis was 14.29° ± 20.02° (range: 0–118 °) and the mean difference in power was −0.46 ± 0.49 D (range: −2.34–0.27 D).
In the CQ group, the mean target Q was −0.4 ± 0.09 and the difference between the target Q and the preoperative Q was −0.06 ± 0.09.
The mean estimated ablation depth was 55.05 ± 17.13μ (range: 20.17–99.39 μ) in the TG group and 53.08 ± 18.61 μ (range: 13.47–96.68 μ) in the CQ group (p = 0.628).
Refractive Outcomes
No significant difference was found between the 2 groups in LogMAR UDVA, or LogMAR CDVA at 1, 3 or 6 months postoperatively, as shown in Table 3.
 |
Table 3 Comparison of UDVA, CDVA, Cylinder and MRSE Between the 2 Groups |
Forty-five eyes (95.7%) from the CQ group had < 0.25 D cylinder at 6 months compared to 42 eyes (87.5%) from the TG group (p ˃ 0.05).
The postoperative MRSE was significantly lower in the CQ group compared to the TG group at 3 months (p = 0.046) but at 6 months no significant difference was observed.
Safety
Of the 104 eyes, 6.3% lost 1 or more lines of CDVA in the TG group compared to 6.4% of the CQ group. The CDVA was 0.0 LogMAR (20/20) or better in 93.9% of eyes in the TG group and in 93.6% in the CQ group.
Efficacy
The percentage of patients achieving LogMAR UCVA of −0.10 (20/16) or better was 48% in the TG group and 46.3% in the Q value adjusted group.
Of patients in the TG group, 77.2% achieved LogMAR UCVA of 0.00 (20/20) or better compared to 86.7% in the CQ group.
Predictability
Of eyes in the CQ group, 100% were within 0.5 D of emmetropia, compared to 93.8% of eyes in the TG group. The difference between groups was non-significant (p = 0.242).
Stability
Stability was similar in both groups (p > 0.05), with 11 eyes (21.2%) in the TG group and 9 eyes (17.3%) in the CQ group having an MRSE change of more than 0.5D over 1, 3 and 6 months postoperatively.
Q Value
In the TG group, ΔQ 15° shows an initial prolate shift at 1 month, as shown in Figure 1. This shift was only temporary and both groups showed a statistically significant oblate shift at 6 months compared to preoperatively in all 3 areas of measurement, as shown in Tables 4 and 5. This oblate shift was smaller in the TG group compared to the CQ group in the 3 areas of measurement, but with p-values of > 0.05, as shown in Table 6.
 |
Table 4 Q Value by Topolyzer in TG Group |
 |
Table 5 Q Values by Topolyzer in CQ Group |
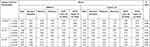 |
Table 6 Comparison of ΔQ at 1, 3 and 6 Months Between the 2 Groups |
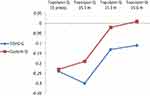 |
Figure 1 Q value at 15° in the 2 groups. Abbreviations: preop, preoperative; m, month/s. |
It was noted that the rate of progressive postoperative oblate shift was more gradual from 3 to 6 months in both groups (as shown in Figure 1).
Corneal Aberrations, ABR and ISV
The aberration coefficient of astigmatism significantly decreased at 6 months in both groups, as shown in Tables 7 and 8. No significant difference was found between the decrease in both groups at 6 months, as shown in Table 9 and Figure 2A.
 |
Table 7 Corneal Aberrations by Topolyzer in TG Group |
 |
Table 8 Corneal Aberrations by Topolyzer in CQ Group |
 |
Table 9 Comparison of Percentage Change in Corneal Aberrations in Both Groups |
TG PRK induced a statistically insignificant decrease in coma at 6 months, as shown in Table 7, unlike the significant increase in coma in the CQ group at 6 months, as shown in Table 8. A statistically significant difference was found between the changes in both groups at 6 months, as shown in Table 9 and Figure 2B.
TG PRK caused a statistically significant decrease in trefoil at 6 months, as shown in Table 7, compared to the insignificant increase in trefoil in the CQ group, as shown in Table 8. A statistically significant difference was found between the changes in both groups at 6 months, as shown in Table 9 and Figure 2C.
Spherical aberrations were significantly increased in both groups at 6 months, as shown in Tables 7 and 8. TG PRK caused a smaller increase in spherical aberrations than CQ PRK at 6 months, but the difference was not statistically significant, as shown in Table 9 and Figure 2D.
A statistically significant increase in ABR in both groups was found at 6 months (p = 0.001 and 0.003, respectively).
An increase in ISV at 6 months was not statistically significant in either groups (p > 0.05).
There were no statistically significant differences between the groups in terms of the increase in ABR or ISV, as shown in Table 10.
 |
Table 10 Change in ABR and ISV from Preoperative Values in the 2 Groups at the 3 Follow-Up Visits |
Predictors of ΔQ in CQ Group
In the CQ group, a significant positive correlation was found between ΔQ (in all 3 areas of measurement) with age and the estimated ablation depth. No significant correlation was found with the target Q or the change in Q (target – preoperative Q), as shown in Table 11.
 |
Table 11 Correlation Between ΔQ and Various Factors in CQ Group |
Estimated ablation depth in the CQ group was found to be a statistically significant predictor of ΔQ on performing linear regression of age and ablation depth, as shown in Table 12.
 |
Table 12 Linear Regression Analysis for Independent Predictors of ΔQ in CQ Group |
In the CQ group, each patient had a different target Q according to the nomogram used based on patient’s age. Q 6mm at 6 months was significantly higher (more oblate cornea) in 30–35 year old patients compared to those younger than 30 years, as shown in Tables 13 and 14.
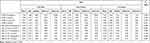 |
Table 13 Comparison of the 3 Age Groups in CQ Group |
 |
Table 14 P-value Between the 2 Age Groups in CQ Group |
HOAs and Strehl Ratio by Combined Placido Disc and Scheimpflug Camera Corneal Tomography
There was no statistically significant difference in the percentage of change in total RMS, RMS astigmatism and RMS spherical aberrations between the groups, but the increase in RMS for coma was significantly higher in the CQ group at 1, 3 and 6 months, as shown in Table 15.
 |
Table 15 Percentage Change of RMS and Strehl Ratio at 1, 3 and 6 Months: Comparison Between the 2 Groups |
The median percentage increase (improvement) of the Strehl ratio was slightly higher in the TG group; however, no significant difference between the groups was found at 6 months, as shown in Table 15.
Contrast Sensitivity
At 6 months, the difference in contrast sensitivity between the TG group (195.79 ± 86.65 C/S [range: 70–44]) and CQ group (184.38 ± 72.29 C/S [range: 78–400]) was not statistically significant (p = 0.745).
Complications
One month after surgery, 5 eyes in the TG group and 6 eyes in the CQ group had grade 1 haze that disappeared by 6 months in all eyes. One patient had enhancement in the CQ adjusted eye 2 months after surgery, thus was excluded from 3- and 6-month follow-ups.
Discussion
Topography guided ablation was primarily used for irregular astigmatism and retreatments in severely aberrated corneas with decreased CDVA for which even refraction is unreliable,8,9 then started to gain popularity for the treatment of virgin corneas.10
Custom Q ablation induces a controlled amount of spherical aberration to increase the depth of focus, while maintaining the prolate shape of the cornea.11
In the present study we found no significant difference between TG PRK and CQ PRK in UDVA, CDVA or MRSE at 1.3 or 6 months postoperatively, similar to the results of Hamza et al, who compared TG LASIK to CQ LASIK at 3 months.4
In the present study, 93.8% of eyes in the TG group were within 0.5 D of emmetropia. TG ablation in virgin eyes using manifest refraction is more predictable than TG ablation using topography neutralizing techniques in post-refractive surgery eyes. The latter resulted in 75% of eyes within 0.5 D of emmetropia.11 Of the eyes of the CQ group in our study, 100% were within 0.5 D of emmetropia. Target Q was changed according to a nomogram and no adjustment of sphere was done.
Studies have reported different ways to increase predictability in CQ ablation. Some have recommended adjustment in the refractive nomogram when changing the target Q.12,13 Others have recommended keeping the target Q unchanged from its preoperative values.14 In our study we neither kept the target Q unchanged nor made any adjustments in the refractive nomogram, and we still had 100% of the cases within 0.5 D of emmetropia in the CQ group.
The ISV, a clue to regularization of the anterior corneal contour, was reported to improve significantly after TG LASIK in irregular corneas, and increase insignificantly after TG PRK in irregular corneas.15 This was similar to the results in our 2 groups, where the ISV increased insignificantly, probably due to the healing process and epithelial remodeling after PRK, besides the fact that we included regular corneas in virgin eyes in contrast to the irregular corneas in those studies.
Koller et al reported that CQ LASIK causes less oblate shift than wavefront guided LASIK. The difference was statistically significant only within the inner 3.5 mm of the cornea (Q10 and 15 degrees from the apex of the cornea).16 However, in our study, the CQ group produced a more oblate shift compared to the TG group.
Different studies have reported the time needed for epithelial thickness stabilization after PRK. Some reported that it can take years for corneal thickness to return to preoperative levels.17 However, the rate of the highest increase in thickness was reported to be between 1 and 3 months, with no significant change during 3 to 6 months.18,19 Likewise, in the present study, although Q values (oblate shift) continued until 6 months, the rate of increase was more gradual from 3 to 6 months.
Koller et al reported a linear relation between amount of oblate shift and that of myopic correction.1,16 Our results confirm the significant positive correlation between oblate shift and ablation depth in the CQ group. Ablation depth continues to be a significant predictor of oblate shift even when using an ablation profile that controls the intended Q shift. The correlation between the oblate shift and both target Q and change in Q was not statistically significant.
This finding contradicts Koller et al's assumption that, by increasing the prolateness of the target Q, the oblate shift will be further diminished.16 However, Chen and Stojanovic reported that more prolate Q-targets will not necessarily diminish the remaining oblate shift found in CQ ablation,20 which explains our results. This is attributed to a decrease in effective radiant laser energy towards the periphery, reflection losses,20 corneal biomechanical responses and epithelial and stromal remodeling after surface ablation.21
CQ ablation enables near and distance vision by increasing depth of focus, hence its use in correction of presbyopia, without excessive reduction in the quality of vision.16 This explains why our CQ group showed significantly worsened postoperative coma while the TG PRK group showed a statistically insignificant improvement of coma. The CQ group showed a statistically insignificant worsening of trefoil in contrast to the TG group that showed significantly improved trefoil. This created the statistically significant difference between the groups in coma and trefoil.
Our results were different from the findings of Hamza et al, who reported non-significant differences between TG LASK and CQ LASIK in terms of total RMS, coma, trefoil and spherical aberrations.4
Contrast sensitivity was smaller in the CQ group, but the difference was statistically insignificant. No statistically significant difference in Strehl ratio was found between the 2 groups at any follow-up. However, intragroup analysis proved that it increased significantly from the preoperative data in both groups (17.98% increase in the TG group [p = 0.033] and 11.96% increase in the CQ group [p < 0.001] at 6 months.
These findings may support what other authors have concluded, that is, that the quality of vision produced by oblate corneas is mostly similar to that produced by prolate ones, due to the interrelation of multiple factors affecting the subjective evaluation of quality of vision.16,22
To the best of our knowledge, this is the first contralateral study comparing TG and CQ PRK. We conclude that topography guided utilizing manifest cylinder and Q value adjusted PRK without adjustment of manifest sphere yielded similar results regarding VA and quality of vision in cases of myopia or astigmatism. However, a progressive oblate shift was noted with time in both groups, thus larger sample sizes and longer follow-up periods are recommended to confirm these findings. A limitation of our study was the relatively short follow-up period (6 months).
Data Sharing Statement
Unidentified data are available for 5 years upon an e-mail request to the corresponding author.
Disclosure
The authors acknowledge no financial interest or grant support received in relation to the study. The authors report no conflicts of interest in this work.
References
1. Applegate RA, Howland HC. Refractive surgery, optical aberrations, and visual performance. J Refract Surg . 1997;13(3):295–299.
2. Gatinel D, Malet J, Hoang-Xuan T, Azar DT. Analysis of customized corneal ablations: theoretical limitations of increasing negative asphericity. Invest Ophthalmol Vis Sci. 2002;43:941–948.
3. Patel S, Marshall J, Fitzke FW, Gartry DS. The shape of the corneal apical zone after excimer photorefractive keratectomy. Acta Ophthalmol (Copenh). 1994;72(5):588–596. doi:10.1111/j.1755-3768.1994.tb07184.x
4. Hamza I, Assaf A, Tarek M, Naggar E. Q value based ablation profile versus topography-guided LASIK: a Contralateral Comparative Study. J Hosp Med. 2018;71:2470–2476.
5. Stulting RD, BS Fant, Bond W, et al.; TCAT study group. Results of topography-guided laser in situ keratomileusis custom ablation treatment with a refractive excimer laser. J Cataract Refract Surg. 2016;42(1):11–18. doi:10.1016/j.jcrs.2015.08.016.
6. Manns F, Ho A, Parel J-M, Culbertson W. Ablation profiles for wavefront-guided correction of myopia and primary spherical aberration. J Cataract Refract Surg. 2002;28:766–774.
7. Tan J, Simon D, Mrochen M, Por YM. Clinical results of topography based customized ablations for myopia and myopic astigmatism. J Refract Surg. 2012;28(11):S829–36. doi:10.3928/1081597X-20121005-04
8. Du C, Yang Y, Shen Y, Wang Y, Dougherty PJ. Bilateral comparison of conventional versus topographic-guided customized ablation for myopic LASIK with the NIDEK EC-5000. J Refract Surg. 2006;22(7):642–646. doi:10.3928/1081-597X-20060901-04
9. Reinstein DZ, Archer TJ, Gobbe M. Combined corneal topography and corneal wavefront data in the treatment of corneal irregularity and refractive error in LASIK or PRK using the Carl Zeiss Meditec MEL 80 and CRS-Master. J Refract Surg. 2009;25(6):503–515. doi:10.3928/1081597X-20090512-04
10. Motwani M. The use of Wavelight® Contoura to create a uniform cornea: the LYRA protocol. Part 3: the effect of higher-order corneal aberrations on refractive astigmatism. Clin Ophthalmol. 2017;11:897–905. doi:10.2147/OPTH.S133839
11. Lin DT, Holland SR, Rocha KM, Krueger RR. Method for optimizing topography-guided ablation of highly aberrated eyes with the ALLEGRETTO WAVE Excimer Laser. J.Refract.Surg. 2008;24(4):S439–S445. doi:10.3928/1081597X-20080401-22
12. Huang H, Yang J, Bao H, Chen S, Xia B, Zou J. Retrospective analysis of changes in the anterior corneal surface after Q value guided LASIK and LASEK in high myopic astigmatism for 3 years. BMC Ophthalmol. 2012;18:12–15.
13. Zhang Z-W, Niu W, Ma M, Jiang K, Ke B. Time course of Q value after myopic laser-assisted in situ keratomileusis. Chinese Med Sci J. 2011;26(3):141–145. doi:10.1016/S1001-9294(11)60038-2
14. Faria-Correia F, Ambrosio JR, Mendes JF, Cummings AB. Custom manipulation of corneal asphericity. The Q Factor. In: Cummings AB, Sinjab M, editors. Customized Laser Vision Correction.
15. Jankov MR, Panagopoulou SI, Tsiklis NS, Hajitanasis GC, Aslanides LM, Pallikaris LG. Topography-guided treatment of irregular astigmatism with the WaveLight excimer laser. J Refract Surg. 2006;22(4):335–344. doi:10.3928/1081-597X-20060401-07
16. Koller T, Iseli H, Hafezi F, Mrochen M, Seiler T. Q-factor customized ablation profile for the correction of myopic astigmatism. J Cataract Refract Surg. 2006;32(4):584–589. doi:10.1016/j.jcrs.2006.01.049
17. Patel SV, Erie JC, McLaren JW, Bourne WM. Confocal microscopy changes in epithelial and stromal thickness up to 7 years after LASIK and photorefractive keratectomy for myopia. J Refract Surg. 2007;23(4):385–392. doi:10.3928/1081-597X-20070401-11
18. Chen X, Stojanovic A, Liu Y, Chen Y, Zhou Y, Utheim TP. Postoperative changes in corneal epithelial and stromal thickness profiles after photorefractive keratectomy in treatment of myopia. J Refract Surg. 2015;31(7):446–453. doi:10.3928/1081597X-20150623-02
19. Sedaghat MR, Momeni-Moghaddam H, Gazanchian M, et al. Corneal epithelial thickness mapping after photorefractive keratectomy for myopia. J Refract Surg. 2019;35(10):632–641. doi:10.3928/1081597X-20190826-03
20. Chen X, Stojanovic A Corneal optical regularization and biomechanical stabilization in keratoconus and irregular astigmatism by use of topography-guided custom ablation and corneal cross-linking [Ph D thesis] Norway: University of Oslo, SynsLaser Kirurgi; June 2016:84–87.
21. Kezirian G, Stonecipher K. Subjective assessment of mesopic visual function after laser in situ keratomileusis. Ophthalmol Clin North Am. 2004;17(2):211–224. doi:10.1016/j.ohc.2004.03.004
22. Mastropasqua L, Toto L, Zuppardi E, et al. Photorefractive keratectomy with aspheric profile of ablation versus conventional photorefractive keratectomy for myopia correction: six-month controlled clinical trial. J Cataract Refract Surg. 2006;32(1):109–116. doi:10.1016/j.jcrs.2005.11.026
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

