Back to Journals » Open Access Journal of Contraception » Volume 13
Contraceptive Utilization and Unmet Need for Contraception Among Women Undergoing Treatment for Tuberculosis in Addis Ababa, Ethiopia: a Cross-Sectional Study
Authors Solomon S , Yitayew B , Kebede A
Received 10 November 2021
Accepted for publication 27 March 2022
Published 8 April 2022 Volume 2022:13 Pages 29—38
DOI https://doi.org/10.2147/OAJC.S348811
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Semaria Solomon,1,* Berhanu Yitayew,2,* Abebaw Kebede3
1Department of Microbiology, Immunology and Parasitology, St. Paul’s Hospital Millennium Medical College (SPHMMC), Addis Ababa, Ethiopia; 2College of Health Science, Debre Berhan University (DBU), Debre Berhan, Ethiopia; 3TB/HIV Research Directorate, Ethiopian Public Health Institute (EPHI), Addis Ababa, Ethiopia
*These authors contributed equally to this work
Correspondence: Semaria Solomon, P.O.Box: 25181/1000, Addis Ababa, Ethiopia, Email [email protected]
Introduction: Pregnancy can pose a risk to women on tuberculosis (TB) treatment with a threat to the wellbeing of the mother and fetus. Physiological and stress-related effects result when pregnancy occurs during TB illness and while on treatment. Hence, this study aimed to assess contraceptive utilization, unmet need among women on TB treatment, and integration of family planning (FP) services with TB clinics in Addis Ababa, Ethiopia.
Methods: A facility-based cross-sectional study was conducted using an interviewer-administered questionnaire. A total of 316 women aged 18– 49 who were on TB treatment were enrolled. Contraceptive utilization rate, unmet need, and integration of FP and TB services were determined. Logistic regression models were conducted to identify factors associated with contraceptive utilization.
Results: Among women on TB treatment 49 (41.9%) were using contraceptives. Out of contraceptive users, 10 (34.5%) used contraceptives to limit and 18 (62.1%) used to space. Only parity had a significant association with contraceptive utilization. Women who had 1– 3 children were less likely to use contraception than those who had ≥ 4 children. Among women who were married or sexually active, 12 (18.9%) had an unmet need. Of the study participants, 144 (45.6%) had been informed about FP services at the TB clinics.
Conclusion: The contraceptive utilization rate in the current study (41.9%) is slightly higher than the national prevalence (36.2%) yet it is still low. Furthermore, the unmet need (18.9%) was lower than the national report for the general population (22%). Educating women about the risk of getting pregnant while visiting the health facility for TB medication will help to improve their chances of better recovery and avoid medication side effects on the fetus. TB guidelines can consider providing FP counseling when initiating treatment to provide women with the power of information to make deliberate decisions.
Keywords: TB, contraceptive, unmet need
Background
Tuberculosis (TB) often affects the young productive and fertile segment of society.1 Furthermore, if pregnancy occurs with TB, it has serious maternal and neonatal complications including increased risk of maternal morbidity, cesarean delivery, preterm birth, low birth weight, and as well as perinatal death.2 Likewise, TB is listed among the conditions associated with increased risk for adverse health events as a result of pregnancy.3 Pregnant women with active TB should be treated, even in the first stage of pregnancy. Although the first-line drugs used in the initial treatment regimen for TB cross the placenta, they do not appear to have harmful effects on the fetus. The problem is pronounced if the mother develops Multi-Drug Resistance-Tuberculosis (MDR-TB) in which the regimens become more toxic. Drugs such as Streptomycin, Kanamycin, Amikacin, Capreomycin, and Fluoroquinolones are contraindicated during pregnancy.4 Globally in 2011, 216,500 active TB cases were reported among pregnant mothers of which the majority were in Africa and Southeast Asia.5 However sufficient data is lacking on the exact numbers of women getting pregnant while on TB medication.
Family planning (FP) is a means of providing safe motherhood and reproductive right which has an important role in preventing unwanted pregnancy and reducing fertility rate.6 Similarly, women identified as having an unmet need include those who express a desire to postpone their next birth for more than two years (spacing) as well as those who wish to have no more children (limiting).7 It can be also defined as women who are sexually active, who are fertile but are not using any contraceptives. For example, lactating women in amenorrhea during the first 6 months post-partum are considered unfertile, and as such, cannot have unmet need. There should be special provisions made for women planning to bear children while on TB treatment with counseling of the risks involved of the two occurring together. This involves providing her all the existing evidence to help her make informed decisions. A high risk patient may prefer to either avoid pregnancy altogether to enhance her health or delay pregnancy until therapy is completed.3 Further research is required for women on TB treatment around appropriate service delivery means to assess, integrate, and enhance uptake of FP services among clients.
There is a data gap in Ethiopia so far on the use and unmet need for contraception among TB patients. Assessing the unmet demand for FP methods among women and addressing the need is a critical element in enabling the sexual and reproductive rights of TB patients. This will also enable synergy between communicable diseases and reproductive and sexual health services. We aim to assess the contraceptive utilization, unmet need, and integration of FP in TB clinics among women on TB treatment.
Methods
A cross-sectional study was conducted at five health centers (HCs) and one TB referral hospital (St. Peter’s TB Specialized Hospital) in Addis Ababa, Ethiopia from March to November 2016. Addis Ababa is the capital city of Ethiopia. It has a total population of 4,793,699 according to the 2020 World Population Review.8 At the time of the study, there were 47 HCs and 41 public and private hospitals. St. Peter’s TB Specialized Hospital is the only public TB referral hospital in the city and was purposefully included for the study whereas the HCs were selected by systematic random sampling of every 10th HC based on alphabetical ordering among all the existing HCs in each Sub-city of Addis Ababa. Study participants were women on TB treatment in the TB clinics within the reproductive age group (18–49 years). The sample size was determined using the standard formula for sample size determination taking 29% Contraceptive Prevalence Rate (CPR) of the 2011 EDHS report, 95% confidence interval, and a precision of 5%. A random sampling technique was used to select study participants from the registry of patients on TB treatment at the treatment centers that had bacteriologically confirmed TB diagnosis. All women coming to the TB treatment were approached to attain a total of 316 patients with the standard formula for sample size calculation. TB confirmed women of reproductive age were included in the current study with a response rate of 100% from March to November 2016. Data were collected using structured questionnaires that were pretested and validated. The questionnaire was developed in English and translated into the local language (Amharic) and translated back to English to check for consistency. The questionnaires were pretested in the same participants to avoid measurement errors. Data were collected by nurses trained on the purpose of the study and on how to administer and complete the questionnaire verbally (that took about 8 minutes on average to complete). After the explanation of the purpose of the study, participants provided signed informed consent to participate and were enrolled when they come to HCs for TB medication by the data collectors. Institutional Review Board (IRB) approval was obtained from SPHMMC and communicated with a permission letter to each study site.
The data were entered into Epi Info version 7 and exported to SPSS version 20 software for analysis. Frequencies and cross-tabulations were used to summarize descriptive statistics of the data and tables and graphs were used for data presentation. Univariate logistic regression was used primarily to check for variables that have an association with the dependent variable individually. Furthermore, variables were entered into multiple logistic regressions for controlling the possible effect of confounders and finally, the variables which had a significant association with contraceptive utilization were assessed by using OR with 95% CI. Variables with a p-value of ≤ 0.05 in the multivariate analysis were considered to have a significant association with contraceptive utilization. Modern contraceptive is defined as a product or medical procedure that interferes with reproduction from acts of sexual intercourse excluding the traditional, natural, and physiological methods.9 Modern contraceptive utilization in this study was defined as the percentage of women currently using any of these methods of contraception among all women (i.e., those aged 18 to 49) who are married, in a union, and sexually active single women. Similarly, the in-union group includes women living with their partner in the same household and who are not married according to the marriage laws or customs of a country. While the unmet need is taken to be the percentage of married, in-union, single, and sexually active women of reproductive age who want to stop or postpone childbearing but who report that they are not using any method of contraception to prevent pregnancy.
Result
Socio-Demographic Characteristics of Women on TB Treatment in Addis Ababa, Ethiopia
A total of 316 TB confirmed women of reproductive age were included in the current study. The median age of the respondents was 28±6.839. The majority of women were from urban areas (81.3%). About 51.8% had secondary education or higher and 23.6% had elementary education. The average monthly income was about 46 $ per month with a 54.4% unemployment rate. The majorities (55.1%) of the participants were single and 29.4% were married, the remaining were separated, divorced, or widowed. Of the total, at the time of the study, 71.5% were not in a union. Among the study participants, 62% had no children, while 30.7% had one to three children. During the data collection, 5(1.6%) were found to be pregnant. The rest were not pregnant (97.8%) or not confirmed (undecided) (0.6%) (Table 1).
 |
Table 1 Sociodemographic Characteristics and Contraceptive Utilization Among Women on Tuberculosis Treatment in Selected Health Facilities in Addis Ababa, Ethiopia (N=309)* |
Contraceptive Utilization of Women on TB Treatment in Addis Ababa, Ethiopia
The utilization of contraceptives among women on TB treatment was 41.9%, 95% CI (32.5–50.4). From the total married women (93), 28 were currently using contraceptives of which 10 (35.7%) were using to limit by either wanting no more children or wanting later. All the rest 18 (64.3%), were using to space. The majority of contraceptive users were using equally Implant or IUD followed by injection, oral contraceptive, and tubal ligation (Figure 1). When participants were asked if they ever used a contraceptive, 32.6% were using contraceptives previously. Contraceptive utilization among referred rural women was 9(18.8%). In the univariate logistic regression analysis, age was significantly associated with contraceptive utilization (P=0.01). Twenty-eight (32.2%) married and 17 (9.8%) single women were using contraceptives. In the univariate logistic regression analysis, marital status is significantly affecting contraceptive utilization. Nonetheless, as married women might not be with their partners at the study time due to their TB status, the study participants were divided into two groups, in union and not in a union. It was found that the majority of women in a union were more likely to use modern contraceptive than women who were not currently in a union during the study, 28 (33.3%), and 22 (9.8%) respectively in univariate logistic regression analysis. Likewise, women having 1–3 children were less likely to use modern contraceptives than those who had ≥4 children (Table 1).
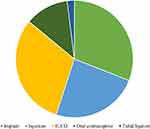 |
Figure 1 Type of contraceptive used among women on TB treatment in selected health facilities in Addis Ababa, Ethiopia. |
In the univariate logistic regression analysis age group, union, parity, knowledge of women where FP services are available, and closeness of FP service providing places were significantly associated with modern contraceptive utilization. Taking these factors however, in multivariate analysis, only parity had a statistically significant association with contraceptive utilization (AOR=0.796, 95% CI (0.260, 0.244, p=0.001). Women who had 1–3 children less likely used contraception than those who had ≥4 children (Table 2). However, education status, occupation, and monthly income were not significantly associated with contraceptive utilization (Table 1).
 |
Table 2 Bivariate and Multivariate Logistic Regression Among Women on Tuberculosis Treatment in Selected Health Facilities in Addis Ababa, Ethiopia (N=309) |
Unmet Need for Contraceptive Utilization Among Women on TB Treatment in Addis Ababa, Ethiopia
Unmet need for contraceptives was determined among married and sexually active single women. The prevalence of pregnancy among TB patients was 2% (6/316). Among married women who were not using contraceptives, 6 women were pregnant or postpartum amenorrheic (period not returned since last live birth in the last 2 years). Four women wanted current pregnancy, while one postpartum amenorrheic woman wanted last birth at that time indicating she had no unmet need. There was one pregnant woman who wanted the pregnancy later, making her have an unmet need for spacing. Participants who were not using contraceptives, not pregnant or postpartum amenorrheic were 58 women. Infecund women are those who married 5+ years ago, had no children in the past 5 years, and never used contraception. In the present study, 35 women were infecund and did not have an unmet need. While there were 23 fecund women of which 11 wanted a child within 2 years while the 12 had unmet contraceptive needs. The unmet need determination included both married and sexually active single women. The prevalence of unmet need in the current study was found to be 18.9% (Figure 2) according to the revised unmet need.10 No variable was significantly associated with the unmet need among women on TB treatment.
 |
Figure 2 Unmet need among married women on tuberculosis treatment in selected health facilities in Addis Ababa, Ethiopia. |
Family Planning Services in TB Clinic
During their TB treatment, 144 (45.6%) reported having been told about FP services. All of these were referred for FP services in the health facility. The majority 74.4% (235/316) knew where they can get modern contraceptives and 91% (213/235) of the respondents reported that these places were close to their homes (within a 2km radius). Among the 144 women that were informed about FP services during their TB treatment, 18.6% (26/144) were using a contraceptive. This was relatively higher than those who were not informed about FP during anti-TB treatment. Of the women told about FP services at the HC or referred for FP in the HC, 20% (28/118) and 19.5% (23/118) used contraceptives, respectively. Nonetheless, there was no significant difference in contraceptive utilization. Out of 213 study participants who knew where to get modern contraceptive, 20.2% (43/213) were using contraceptives which is significantly higher than those who did not know where to get the contraceptive (3/15). The closeness of FP clinic to home had a significant association (p=0.017) for the utilization of contraceptives in the univariate logistic regression analysis (Table 3).
 |
Table 3 FP Services Linkage in TB Clinic Among Women on Tuberculosis Treatment in Selected Health Facilities in Addis Ababa, Ethiopia (N=309) |
Discussion
Many girls and women in developing countries who do not want to get pregnant lack access to contraceptives, information, and services which, for many, will cost them their lives.11 Considering the duration, severity of illness, and treatment effect, patients on TB treatment should be well informed before getting pregnant. To prevent this there is a platform for FP at the TB clinics. There is limited work on contraceptive utilization studies among women on TB treatment and this report tries to provide information by determining the contraceptive utilization rate, unmet need, and FP services within the TB clinics in Addis Ababa. In this study contraceptive utilization among women was found to be 41.9% which is slightly higher than the national rate, 36.2% in the general population. However, according to the EDHS of 2016, the general contraceptive rate in Addis Ababa was 50% which is higher than our finding.12 For the general population studies in East Africa (40%), the United Republic of Tanzania (40.6%) and Madagascar (46%) reported their corresponding figures.13 The finding is lower than the world prevalence (64%), Europe (69%), Asia (68%), Northern Africa (53%), Southern Africa (64%), Zimbabwe (66%), Rwanda (53.5%) and Kenya (57.4%).13 Whereas, the current finding is higher than the African continent (33%) and Subsaharan Africa (28%) among female adolescents.13 This could be due to different health service seeking behavior, socio-cultural inclinations, and differences in the health service delivery system. Similarly, our finding is higher than the prevalence of Gonder and Bahir Dar towns (34.3%) among street women in Ethiopia.14 This could be that street women do not visit HCs more often than women on TB treatments who are visiting HCs daily for Directly Observed Therapy (DOTs). As a result, they could have better awareness and practice about FP than other women in the community.
Although a relatively higher percentage of rural residents utilize contraceptives than urban, no significant difference was observed. The high contraceptive prevalence rate among rural residents might be due to a small number of rural participants in the study. The finding is inconsistent with the report by Lakew et al.15 In our study, women from both urban and rural settings visited HC to get TB treatment having similar access to health services provided by health facilities. As the 2015 UN economics and social affairs report on the type of contraceptives, female sterilization, and IUCD are the two most common methods used by married or in-union women worldwide, 19% of married or in-union women relied on female sterilization and 14% used IUCD. Short-term methods are less common, 9% of women used pills, 8% relied on male condoms and 5% used injectable.13 Similarly in the current study, the majority of women were equally using IUCD or Implant followed by injection, oral contraceptive, and tubal ligation.
Assessing the reasons why women do not prefer to use FP methods is critical in designing programs that could improve the quality of the service, with particular attention given to counseling of women on FP for those on chronic illnesses who could be exposed to unintended and risky pregnancies. In the current study, the majority of women reported that not having sex is a major factor for not using contraceptives. Similarly in a report by Guttmacher Institute, significant proportions of married women with an unmet need gave exposure-related reasons for nonuse. They believed they were not at risk of getting pregnant, most often either because they were breastfeeding or not having sex frequently. They reported among women who were never married, infrequent sexual activity was by far the most common reason for not using contraceptives.16 On the contrary, other scholars reported that never given birth, religious influence, fear of side effects, and desire to have a child were the main reasons why women are not using contraceptives.17
Women who had 1–3 children were less likely to use contraceptives. These women might not have reached the maximum birth limit or might desire to have another child. This could be for the reason that women who reached the maximum birth limit are more likely to use contraceptive. The finding is inline with the report in North Shoa.17 Nonetheless, this finding is inconsistent with unpublished data by Sita S, 2003 who reported women with an ideal family size to have a lower need for FP services.18
Considering age to assess contraceptive utilization, the majority (58%) were in the age group of 23–33. This is in line with the report by Ashford et al, who showed that contraceptive use was higher among women 20–34 years of age. However, the association of contraceptive utilization and age was insignificant in the multivariant analysis. The majority of women were told about where they can get modern contraceptives during their treatment follow up. Almost all of these women were informed about where they can get the service. This shows that the integration of contraceptive services, such as counselling of patients on FP at TB clinics, is a good approach for FP service delivery although a significant difference was not observed. On a study of contraception for high-risk patients, regular counseling might be needed for the women on treatment as they may wish to discontinue methods due to actual or perceived side effects that may be associated with their chronic medical condition, or due to their co-morbidity.3 The closeness of FP service providing places to home was also an important factor for contraceptive utilization. Almost all of the contraceptive user women reported FP outlets were close to their homes. Similarly, the report by Ashford et al showed that contraceptive utilization was higher among women, living within walking distance from a health facility.19
Significant number of women in the current study were infecund. This could be associated with extrapulmonary tuberculosis (pelvic tuberculosis) although confirmatory diagnosis is required. Previously it has been reported that majority of women admitted at infertility unit were AFB positive in endometrium compared to the control groups.20
Worldwide in 2015, 12% of married or in-union women are estimated to have had an unmet need for family planning. The level was much higher, 22% in the least developed countries. Many of the latter countries are in sub-Saharan Africa, which is also the region where the unmet need was highest (24%), double the world average in 2015.13 In Ethiopia, the unmet need for the general population was 22%.12 In the current study, the prevalence of unmet need was found to be 18.9% among married and sexually active single women on TB treatment, this is lower than the general population due to the difference in the repeated health facility visits among the two groups. In countries such as Kenya, Madagascar, Malawi, and Zambia, a decline in unmet need has corresponded with an increase in FP for the general population.13 In this study too, a high contraceptive utilization (41.9%) corresponds to a lower unmet need finding.
Nationally unmet need for FP declined from 25% in 2011 to 22% in 2016.12 According to the 2011 EDHS report, there is variation in unmet need prevalence by region, ranging from a low of 10.6% in Addis Ababa to 29.9% in Oromia.21 Our result’s discrepancy with the report from Addis Ababa could be that the study’s participants were residing in combinations of urban and rural areas (referrals). However, the current finding is comparable to the UN report among married or in-union women in Africa 22% and East Africa 24%.13 TB treatment centers can consider their services to identify and address those in need of FP service. This can be upscaled to the different HCs providing TB treatment to address high-risk patients by asking them about their FP preferences at their commencement of treatment benchmarking from HIV patients during their initiation of ART services. Although women on TB treatment were informed about FP services at the TB clinic, there is no formal integration of the two services for follow-up of outcome. However, a women’s visit to obtain TB treatment could be a good contact point to inform and provide FP services to providing the best available care and also recording outcomes. Further work needs to focus on filling the data gap on women taking TB medication and their contraceptive needs with regards to providing the right counseling. Drug impacts on the fetus should be explored at different points of pregnancy to help with the mother’s informed decision on delaying pregnancy. The stress and psychological impacts of the pregnancy occurring with TB should be investigated to help protect the mother from pressure.
Conclusion
The contraceptive utilization among TB patients was 41.9% which was slightly higher than the national rate. The unmet need (18.9%) in this study was lower than the national report. Women who had no children were more likely to use contraceptives. There is evidence that while the current focus of FP and reproductive health programs is on supporting the well-being of individuals, meeting an unmet need in collaboration with TB management can serve broader agendas such as reducing the pressures of co-occurrences and child and maternal mortality, ultimately reducing unintended pregnancies on societies that are high-risk patients. Integrating family planning services and counseling in TB clinics and access of FP services for women with other chronic health conditions is critical to mitigate maternal morbidity and mortality.
Data Sharing Statement
Data available from the research undertaking are available with the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The research was ethically approved by St. Paul’s Hospital Millennium Medical College and St. Peter’s TB Specialized Hospital. Signed informed consent was obtained from each participant. This study complies with the Declaration of Helsinki.
Acknowledgment
St Paul’s Hospital Millennium Medical College is acknowledged for providing full funding. Study participants’ dedication to the research is appreciated. Abebaw Kebede is supported by a training program from NIH/Fogarty International Center Global Infectious Diseases grant D43TW009127. Pre-Publication Support Service (PREPSS) supported the development of this manuscript by providing pre-publication peer-review and copy editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Full financial support of the study was obtained from St. Paul’s Hospital Millennium Medical College.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health. 2014;2(6):e323–e33. doi:10.1016/S2214-109X(14)70227-X
2. Sobhy S, Babiker ZOE, Zamora J, Khan KS, Kunst H. Maternal and perinatal mortality and morbidity associated with tuberculosis during pregnancy and the postpartum period: a systematic review and meta‐analysis. BJOG. 2017;124(5):727–733. doi:10.1111/1471-0528.14408
3. Cwiak C, Cwiak C. Contraception for high risk patients. Semin Perinatol. 2020;44:151268. doi:10.1016/j.semperi.2020.151268
4. CDC. TB treatment and pregnancy; 2020 [
5. Sugarman J, Colvin C, Moran AC, Oxlade O. Tuberculosis in pregnancy: an estimate of the global burden of disease. Lancet Global Health. 2014;2(12):e710–e6. doi:10.1016/S2214-109X(14)70330-4
6. UN, editor International conference on population and development programme of action. International conference on population and development; 1994.
7. Westoff CF, Bankole A. The potential demographic significance of unmet need. Int Fam Plan Perspect. 1996;22:16–20. doi:10.2307/2950797
8. WPR. World population review; 2020. Available from: https://worldpopulationreview.com/world-cities/addis-ababa-population.
9. Hubacher D, Trussell J. A definition of modern contraceptive methods. Contraception. 2015;92(5):420–421. doi:10.1016/j.contraception.2015.08.008
10. Analytical D. Revising unmet need for family planning; 2012.
11. Cohen SA. London Summit puts family planning back on the agenda offers new lease on life for millions of women and girls. Guttmacher Policy Rev. 2012;15(3):20–24.
12. EDHS. 2016 Demographic and health survey key findings. CSA; 2016.
13. UN. Trends in contraceptive use worldwide 2015; 2015.
14. Megabiaw B. Awareness and utilization of modern contraceptives among street women in North-West Ethiopia. BMC Women’s Health. 2012;12(1):31. doi:10.1186/1472-6874-12-31
15. Lakew Y, Reda AA, Tamene H, Benedict S, Deribe K. Geographical variation and factors influencing modern contraceptive use among married women in Ethiopia: evidence from a national population based survey. Reprod Health. 2013;10(1):52. doi:10.1186/1742-4755-10-52
16. Sedgh G, Hussain R, Bankole A, Singh S. Women with an unmet need for contraception in developing countries and their reasons for not using a method. Occas Rep. 2007;37:5–40.
17. Mohammed A, Woldeyohannes D, Feleke A, Megabiaw B. Determinants of modern contraceptive utilization among married women of reproductive age group in North Shoa Zone, Amhara Region, Ethiopia. Reprod Health. 2014;11(1):13. doi:10.1186/1742-4755-11-13
18. Sita S. Assessment of the magnitude and determinants of unmet need for family planning among currently married women in urban and periurban community in Hawassa, southern Ethiopia. Addis Abeba Universty; 2003.
19. Sedgh G, Ashoford LS, Hussain R. Unmet need for contraception in developing countries: examine women’s reasons for not using a method. The Guttmacher Institute; 2016.
20. Banu J, Begum S, Fatima P. Association of pelvic tuberculosis with tubal factor infertility. MMJ. 2009;18(1):52–55.
21. EDHS. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistics Agency and ORC Macro; 2011.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
