Back to Journals » Open Access Journal of Contraception » Volume 10
Contraceptive Options Following Gestational Diabetes: Current Perspectives
Authors Turner AM , Donelan EA, Kiley JW
Received 19 April 2019
Accepted for publication 4 September 2019
Published 22 October 2019 Volume 2019:10 Pages 41—53
DOI https://doi.org/10.2147/OAJC.S184821
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Igal Wolman
Ashley M Turner, Emily A Donelan, Jessica W Kiley
Department of Obstetrics and Gynecology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA
Correspondence: Jessica W Kiley
Department of Obstetrics and Gynecology, Northwestern University Feinberg School of Medicine, 250 E. Superior St., Suite 05-2168, Chicago, IL 60611, USA
Tel +1 312 695-4458
Fax +1 312 472-0511
Email [email protected]
Abstract: Gestational diabetes mellitus (GDM) complicates approximately 7% of pregnancies in the United States. Along with risk factors related to pregnancy, women with a history of GDM also have an increased risk of developing type 2 diabetes mellitus later in life. These women require special consideration when discussing contraception and other reproductive health issues. GDM carries a category 1 rating in the US Medical Eligibility Criteria for all contraceptive methods, which supports safety of the various methods but does not account for effectiveness. Contraceptive options differ in composition and mechanisms of action, and concerns have been raised about possible effects of contraception on metabolism. Clinical evidence is limited to suggest that hormonal contraception has significantly adverse effects on body weight, lipid, or glucose metabolism. In addition, the majority of evidence does not suggest a relationship between development of type 2 diabetes mellitus and use of hormonal contraception. Data are limited, so it is challenging to make a broad, general recommendation regarding contraception for women with a history of GDM. A woman’s history of GDM should be considered during contraceptive counseling. Discussion should focus on potential medical comorbidities and the implications of GDM on future health, with special consideration of issues including bone health, obesity, cardiovascular disease, and thrombosis risk. Providers must emphasize the importance of reliable, highly effective contraception for women with GDM, to optimize the timing of future pregnancies. This approach to comprehensive counseling will guide optimal decision-making on contraceptive use, lifestyle changes, and planning of subsequent pregnancies.
Keywords: contraception, diabetes, postpartum birth control, metabolic syndrome
Introduction
After many years without change, the unintended pregnancy rate in the United States dropped from 51% in 2008 to 45% in 2011. Increased contraceptive use was a major factor driving the decline.1 In particular, use of long-acting reversible contraception (LARC) gained popularity during that time period.2 However, unintended pregnancy remains a major public health issue, particularly in the postpartum period and in women with chronic medical conditions. Rapid repeat pregnancies are associated with poor obstetric outcomes including preterm birth, fetal growth restriction, and potentially congenital anomalies.3,4 A short inter-pregnancy interval, typically defined as another pregnancy conceived within 12–24 months of delivery, also confers an increased risk of maternal morbidity, including obesity and gestational diabetes.5,6 Women with chronic medical conditions require pre-conception care and preparation for pregnancy, as their conditions and the medications used to treat them warrant attention when planning pregnancy.
Gestational diabetes mellitus (GDM) is a state of abnormal carbohydrate metabolism which develops during pregnancy. Approximately 7% of all US pregnancies in 2009 were complicated by diabetes, with 86% of those women having GDM. Maternal risks with GDM include higher risks of preeclampsia, shoulder dystocia, and cesarean delivery. Fetal and neonatal complications include increased rates of macrosomia, hypoglycemia and hyperbilirubinemia, and birth trauma. These women have an increased risk of developing type 2 diabetes mellitus (T2DM) later in life.7
Women with a history of GDM are a special population to consider when discussing postpartum contraception and pregnancy risks. Published literature estimates that up to 70% of women with a history of GDM will develop diabetes within 22–28 years after pregnancy. Additionally, certain groups may develop subsequent diabetes at an accelerated rate.8
Up to 60% of Latin American women with GDM develop overt diabetes within 5 years after pregnancy.9 Effective contraception is therefore imperative in the postpartum period to plan or avoid future pregnancy. Contraceptive use allows time for medical optimization to improve future pregnancy outcomes. In women who have completed childbearing, prevention of an additional pregnancy may reduce the risk of subsequent T2DM by one-third.10
Birth control method selection depends on factors such as medical comorbidities, current medication use, patient preference, cost, and desire for future fertility. Health care providers must emphasize the importance of pregnancy planning and contraception when caring for women with a history of GDM. Providers should consider issues including the effects of hormonal contraception on weight gain, lipid profiles, insulin sensitivity, glucose metabolism, and ultimately development of T2DM. This review serves as a guide for patient-centered counseling when choosing a method of contraception.
Clinical Guidelines
In 2010, the US Centers for Disease Control (CDC) published the first US Medical Eligibility Criteria for Contraceptive Use (US MEC). The document gives clinical guidelines for choosing a contraceptive method, depending on patient characteristics and medical conditions. The guidelines use an evidence-based, four-tiered category system that provides recommendations for the appropriateness of each contraceptive for women with various medical conditions. Table 1 depicts the US MEC categories and definitions. The US MEC assumes that no other comorbid conditions or risk factors are present, so the highest category rating should be applied for women with more than one condition. The goal of these guidelines is to remove unnecessary medical barriers to accessing and using contraception and to provide guidance for clinicians. The US MEC was updated in 2016.11
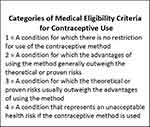 |
Table 1 Reproduced from: Curtis KM, Tepper NK, Jatlaoui TC, et al US Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep 2016;65:1.104 |
History of GDM carries a category 1 rating for all contraceptive methods in otherwise healthy women regardless of age. However, the US MEC does not account for availability, effectiveness and efficacy of the methods, only safety. For example, barrier methods (i.e., condoms) are category 1 for all medical conditions but have a relatively high failure rate of 12–18%.12,13 Therefore, patients should be counseled on all methods of contraception for which they are medically eligible, and effectiveness should be a key aspect of that counseling. Figure 1 shows available contraceptive methods and effectiveness.
For women with GDM, the MEC recommendations for both GDM and for the postpartum state are relevant. During the first 21 days following delivery, all estrogen-containing contraceptives are contraindicated due to increased risk for thrombotic events. Between 21–42 days postpartum the decision to initiate combined hormonal contraception (CHC) depends on additional risk factors for thrombosis and breastfeeding status. Many women with GDM have risk factors for thrombosis, which include age 35 years or older, previous thromboembolism, thrombophilia, immobility, transfusion at delivery, body mass index (BMI) ≥30 kg/m2, postpartum hemorrhage, recent cesarean delivery, preeclampsia, or smoking.14 After 42 days postpartum, all women can use CHC regardless of breastfeeding status or pregnancy-related thromboembolic risk factors. Non-pregnancy related risk factors such as age, smoking, thrombophilia, or previous thromboembolism, and other coexisting conditions may confer independent contraindications to CHC.15 Progestin-only contraception may be initiated at any time after delivery, including immediate postpartum intrauterine device or subdermal implant placement.15 In the immediate postpartum period, it is important not only to consider a history of GDM, but also breastfeeding status and thrombosis risk factors.
Metabolic Effects Of Hormonal Contraception
A considerable body of research reports on the effects of hormonal contraception on weight gain and lipid and carbohydrate metabolism, although study methodology and results are rather mixed. Understanding a contraceptive’s effects on metabolism is especially important in overweight and obese women and in those susceptible to cardiovascular disease and insulin resistance, such as women with prior GDM.
Effects Of Contraception On Weight Gain
Many women perceive weight gain as a concerning side effect of hormonal contraception, and it is often cited as a reason for avoiding or discontinuing contraceptives.16,17 Weight gain and postpartum weight loss are particular concerns for women with a history of GDM, since the risk of GDM is associated with higher body mass index.18
Weight gain and the relationship to contraception is difficult to study for a variety of reasons. Weight gain is a developmentally normal part of adolescence and women tend to gain weight over time.19 There are some ethical challenges to performing randomized, placebo-controlled trials with hormonal contraception. Additionally, there no standard definition of a clinically significant weight change, so a magnitude of weight gain or loss that is clinically significant to researchers may differ from what is relevant to women.17
Many studies have evaluated weight gain with CHC, but no causal association is evident. The majority of studies did not show significant weight gain in CHC users compared to non-users or those using other forms of hormonal contraception.20,21
A 2014 Cochrane Review reported on 49 trials evaluating weight in contraceptive users. The review included studies on combined oral contraceptives, contraceptive patch, and the contraceptive vaginal ring. Only four trials used a placebo or no-intervention group, and no increase in body weight was noted. The vast majority of studies comparing different hormonal formulations of CHCs showed no clinically significant differences in weight between groups. The weight gain that was noted was similar to known patterns of age-related weight gain. Additionally, in 51 comparisons of the same estrogen and progestin types with different doses, only one comparison showed a possible difference in weight between groups. Overall the current evidence remains insufficient.17
Progestin-only contraceptives, particularly depot medroxyprogesterone acetate (DMPA), are commonly linked with weight gain by providers and patients. A 2016 Cochrane Review on progestin contraceptives and weight gain included many studies on DMPA. In the studies that compared DMPA to CHC users, no significant difference in weight gain was noted, although one study did show a significant increase in total body fat with adolescent users of DMPA.22 In the studies comparing DMPA to non-hormonal contraception, data suggested an increase in weight for DMPA users, with a gain of 2–3 kilograms measured over 3 years of use. Of the 16 studies that examined DMPA, three showed an association between weight gain or increased body fat composition. The authors determined the quality of the evidence to be overall low quality.23
A potential concern is use of DMPA in women (both adolescent and adult) who are already overweight or obese at the time of initiation. Some data suggest that overweight or obese patients may gain more weight than normal-weight users of DMPA.24,25 Additionally, postpartum DMPA users were more prone to weight gain if they were overweight or obese before pregnancy, compared with normal-weight women. Postpartum patients using DMPA with a BMI of 26–35 kg/m2 had a weight gain of 11.48 pounds compared to patients with a BMI of 21–25 kg/m2 at one year postpartum. Also, when comparing DMPA users with women who had a postpartum tubal sterilization procedure in the highest BMI group, women using DMPA had a 3.28 pound greater weight gain after one year. DMPA may not be ideal in such women, and other methods of contraception should be considered if appropriate.26,27
The data on the effect of the levonorgestrel intrauterine system (LNG-IUS) on body mass remains unclear. Two studies evaluating body weight with use of the LNG-IUS reported a change in body mass composition (increase in fat mass) without a significant change in weight. One of these studies compared the LNG-IUS and copper intrauterine device (Cu-IUD) over 12 months of use. Women in both groups experienced weight gain, the magnitude of which was similar between groups. The LNG-IUS group exhibited a 2.5% gain in fat mass and a loss of lean mass compared with controls.28 In contrast, other studies evaluating weight gain alone with LNG-IUS compared to Cu-IUD showed no significant increase in weight with the LNG-IUS.29,30
Two trials on progestin-only pills report no significant weight change. One study compared 6-month weight gain in users of norethisterone and levonorgestrel (LNG) pills. The other reported no significant differences in weight change and BMI with desogestrel compared with no hormonal method, although the progestin group showed an increase in fat mass.31,32 Little information is available on weight change with use of the norethindrone tablet, which is the predominant progestin-only pill used in the US
Scant evidence exists on weight change with the etonogestrel (ENG) subdermal implant, the implant contraceptive currently marketed in the United States. One recent prospective study examined body weight and composition of users of the Cu-IUD, LNG-IUS, and ENG implant. The investigators showed no significant difference in body weight or composition between groups over 12 months in 149 women.33 Another study compared DMPA, LNG-IUS, and ENG implant users with Cu-IUD users, and after adjusting for age and race no differences in weight change were noted.29 These results contrast with those of an earlier study showing a 4.1kg increase in weight over 12 months with the ENG implant when compared to a Cu-IUD.34 Evidence on the LNG subdermal implant is also mixed, with two studies comparing the LNG implant to Cu-IUD showing a significant increase in weight and studies comparing the LNG implant to DMPA showed no significant difference in weight between groups.23
Overall, limited evidence exists to suggest a clinically significant weight gain amongst users of progestin-only contraception or combined hormonal contraception. Hormonal contraception should not be avoided in most adult women due to concern for weight gain.
Effects Of Contraception On Lipid Metabolism
It is generally accepted that progestins in hormonal contraception, particularly the more androgenic ones, negatively impact lipid profiles, while estrogens impart a favorable effect. Progestins increase low density lipoprotein (LDL) and triglycerides (TG) and lower high-density lipoprotein (HDL) levels, whereas estrogens increase HDL and very low-density lipoproteins (VLDL) and decrease LDL.35,36
Newer progestins, such as desogestrel, drospirenone, or dienogest may produce a more favorable effect on lipids due to their less androgenic properties. The effects include an increase in HDL without a significant change in LDL levels.37,38 Data suggest that oral contraceptive formulations containing desogestrel and drospirenone increase HDL levels, and formulations containing gestodene or norgestimate decrease LDL levels. Formulations containing LNG demonstrated an adverse effect on lipid profile, and some data suggest a dose-dependent effect, with fewer adverse effects with lower LNG dose.36
One randomized trial reported similar effects on lipid profile in overweight and obese women using oral contraceptives containing ethinyl estradiol plus LNG, compared those using ethinyl estradiol plus desogestrel. The changes in lipid profile in the study population were similar to those reported in previous studies of normal-weight women.39 Another study, which compared the ethinyl estradiol and etonogestrel vaginal ring to an oral contraceptive containing LNG and ethinyl estradiol, reported a more favorable lipid profile with the vaginal ring.40 Brief review of these data may lead to assumptions that CHC users should avoid formulations with LNG, but the data are mixed, and negative effects of LNG on the lipid profile are likely transient.41
Some could postulate that without the protective effects of estrogen, progestin-only contraceptives would worsen lipid profiles. To the contrary, the data on progestin-only pills suggest no significant change in LDL or HDL levels.42 These data are reassuring, although no studies have reported on the effects of norethindrone alone on lipid profile. Norethindrone is currently the only progestin-only oral contraceptive available in the US
Studies on DMPA and lipid metabolism report mixed findings of either worsening of lipids or no change.43 In one study, LDL to HDL ratio increased in the first six months of use, then returned to baseline after one year.44 Despite these potential effects on lipids, no evidence suggests that DMPA use increases the risk of development of cardiovascular disease,45,46 which is the clinically-significant endpoint.
Studies on the ENG implant demonstrate either no change or an improvement in lipid profile. In one study of adolescent implants users, LDL and triglyceride levels decreased while HDL levels rose, all positive changes in regards to cardiovascular disease.47 Another study showed a decrease in HDL levels in healthy adult women, but levels remained in the normal range.48 A small case series reported no changes in lipid profile in eight obese women using the ENG implant.49
Based on the results of several studies, the LNG-IUS confers no significant effect on lipid profiles. One study compared LNG-IUS users to Cu-IUD users and found no difference in lipid levels.50 The results of other studies are consistent with these findings and also reported similar cholesterol levels in LNG-IUS users and non-users.51,52 Data also support similar effects in obese women.49
Effects Of Contraception On Insulin Sensitivity And Glucose Metabolism
Synthetic progestins are structurally similar to testosterone and traditionally believed to produce androgenic side effects. Metabolic effects include reduced tissue insulin sensitivity and glucose tolerance. These effects may be related to dose and differing androgenicity of various progestins.53–56 Newer generations of progestins were developed to limit androgenic side effects, particularly effects on lipoproteins and insulin sensitivity.36,57 Synthetic estrogens may have the opposite effect on insulin sensitivity,58,59 and recent CHC formulations were developed containing estrogen molecules closely resembling natural forms of estrogen. These products, containing estradiol or estradiol valerate, could theoretically improve the safety of CHC, but robust clinical data are not yet available.36
A 2014 Cochrane Review examined the effects of hormonal contraception in both healthy women and women at greater risk of metabolic disorders. Thirty-one trials were included, with the majority reporting on CHC. In general, no marked differences in carbohydrate metabolism were noted, as measured by comparison of glucose or insulin levels, response to glucose challenge, and glycosylated hemoglobin levels. Only one trial stratified participants by body weight, and more than half of the trials excluded women who were overweight or obese, which could make these results less generalizable to women with a history of GDM given their increased propensity for obesity. The review reported no evidence of clinically important changes in carbohydrate metabolism with hormonal contraception, although analysis was limited by heterogeneity in the CHC formulations studied and in study methodology.60
Some data suggest a relationship between DMPA and insulin resistance. A retrospective case-control study among Navajo women demonstrated that women who had used DMPA were more likely to develop diabetes than those who had used CHCs, even after adjustment for BMI. This risk was associated with length of use, but interpretation of findings is limited by study design.61 Another study of DMPA showed that glucose levels began to increase after three months of use and reached maximum levels at 12 months. Although this increase was significant, it did not reach the lower cutoff levels for impaired glucose tolerance or diabetes in any users.62
The effects of the ENG implant on carbohydrate metabolism have been reported in several studies. One reported no differences in carbohydrate metabolism in implant and Cu-IUD users. Insulin and glucose, oral glucose tolerance test, and hemoglobin A1c levels were unaffected though one year of use. Another study evaluated metabolic parameters in ENG implant and LNG implant users. The area under the curve for glucose and insulin levels increased during oral glucose challenge in both groups. There was a statistically significant increase in hemoglobin A1c in ENG implant users over 24 months, but these results are not clinically significant in healthy users.63 Another study showed an increase in fasting glucose from 85mg/dL to 88mg/dL at three years in implant users, a clinically insignificant change.64 Neither of these studies included women with a BMI > 30. In contrast to these studies, which included healthy women, one study reported on metabolic effects of the LNG-IUS and ENG implant in obese women. Results included higher fasting glucose levels and decreased insulin sensitivity among ENG implant users compared with LNG-IUS to the point of pre-diabetes in some women.49
Few studies exist regarding the LNG-IUS and carbohydrate metabolism, and these studies show inconsistent effects on insulin sensitivity and glucose metabolism. One study demonstrated higher rates of impaired fasting glucose in patients using the LNG-IUS, although only in patients with higher baseline levels.52 Another study examined the effects of transdermal estrogen and LNG-IUS in post-menopausal women. Transdermal estrogen increased insulin sensitivity, but this effect was reversed when combined with LNG-IUS.65 A study on glucose metabolism in women with type 1 diabetes using the LNG-IUS compared with those using the Cu-IUD found no differences in fasting glucose or insulin levels, hemoglobin A1c, or daily insulin dosing at six weeks or six months of use.66 Thus, results are mixed on effects of the LNG-IUS on carbohydrate metabolism.
Effects Of Contraception On Bone Mineral Density
In 2004 the FDA added a “black box” warning to the DMPA labeling, recommending caution beyond 2 years of use. The warning was founded on concerns that prolonged use could result in significant, potentially permanent loss of bone mass, correlated with longer duration of use. This statement is based on data that shows a loss of bone mineral density (BMD) of 0.5–3.5% at the hip and spine after 1 year of use, 5.7–7.5% loss after 2 years of use and 5.2–5.4% after 5 years of use. However, most studies with a duration of use of 2–5 years and follow up of 5 years after discontinuation showed that BMD was substantially or fully reversible upon discontinuation of this contraceptive method. While some observational studies suggest a higher fracture risk in women using DMPA, interpretation is limited by poor study design. It is therefore unknown if these BMD changes are clinically significant. Given the possible impact on unplanned pregnancies of limiting DMPA use, especially in vulnerable populations, the World Health Organization (WHO) convened in 2005 to evaluate the scientific evidence. The panel concluded that there should be no restriction on duration of DMPA use in women age 18–45. The American College of Obstetricians (ACOG) supports this recommendation.67
Women with a history of GDM have an increased risk of developing T2DM in the long term. The impact of T2DM on bone health is an often under-appreciated complication of the disorder. T2DM is associated with an increase in BMD but has also been associated with an increased risk of bone fractures. The risk of fractures is thought to be unrelated to BMD and instead related to lower bone quality. A 2017 systematic review included data from 30 studies reported that T2DM was associated with increased risk fracture, with a relative risk of 1.05 (CI 1.04–1.06).68
Given the conflicting data showing an increase in BMD with T2DM and a simultaneous increased risk of fracture, it is unclear if the addition of DMPA would modify this risk. Based on these insufficient data on harms and strong data to support DMPA as an effective contraceptive method, limiting use in patients with T2DM due to concern for fracture is not recommended.
Contraception And Subsequent Type 2 Diabetes In Women With A History Of GDM
GDM manifests as glucose intolerance and hyperglycemia. GDM that is controlled by lifestyle and diet modification is defined as class A1GDM, and GDM requiring medication for glycemic control is designated as class A2GDM. Universal screening for GDM is recommended in the United States. Typically, a 50-g oral glucose challenge is administered at 24 to 28 weeks of gestation. Venous blood glucose is measured one hour after the ingested load, and women with glucose levels above an established threshold subsequently undergo a one-hour, 100-g oral glucose tolerance test. Thresholds for normal values for the one- and three-hour results vary between institutions.7
The effect of contraceptive hormones on the subsequent risk of development of T2DM in women with GDM is unclear. Large cohort studies have shown that hormonal contraception does not increase the risk of development of T2DM in healthy women.59 Given the increased risk of T2DM in women with GDM, some researchers have postulated that the metabolic changes associated with progestins may be magnified in this particular group of women.
Few studies have addressed whether progestin-only methods increase the risk of development of T2DM. One retrospective cohort study including Latina women with a history of GDM reported a relative risk of 2.87 (95% CI 1.57–5.27) of developing T2DM over 7.5 years in women using progestin-only pills compared to CHC or barrier methods. The study may be limited by confounders, as women in the progestin-only pill group had higher BMI, parity, cholesterol levels, and gestational weight gain than the other groups.9 In another study examining women with a history of GDM who had glucose testing postpartum, there was no significant difference in glucose metabolism in women using non-hormonal, combination, or progestin-only methods aside from DMPA. Women using DMPA in the first year postpartum were at higher risk of glucose intolerance.69 A longitudinal study on Latina women with GDM using DMPA reported that women using DMPA, compared with those using COC, were more likely to be diagnosed with T2DM in up to 10 years of follow-up. Annual incidence rates of developing diabetes was 19% in DMPA users, and 12% in COC users, with an unadjusted hazard ratio of 1.58 (95% CI 1.00–2.50; p = 0.05). However, after adjusting for weight gain in the DMPA group, the adjusted hazard ratio was 1.07 (95% CI 0.61–1.89; p = 0.81). The authors suggested that the increased rate of diabetes was related to weight gain in this particularly susceptible group.70
Hormonal IUDs are highly effective and safe in women with diabetes.66,71 A randomized controlled trial of women with Type 1 DM using the LNG-IUS showed no significant differences in fasting glucose, insulin requirements, or glycosylated hemoglobin in LNG-IUS users compared with Cu-IUD users over 12 months of use.66 Additionally, in a small study of postpartum women with GDM, the LNG-IUS did not impact postpartum glucose tolerance.72 The Cu-IUD is also safe in women with diabetes and provides a highly effective, non-hormonal long-acting reversible contraceptive method.
As IUDs and implants are now being placed in the immediate post-partum period (during the hospitalization for labor and delivery), it was essential to evaluate the impact of contraception and postpartum follow-up. One study studied postpartum women in California and showed that women with diabetes were more likely to follow up for postpartum care than women without diabetes.73 Data from another study suggested that women who received contraception prior to hospital discharge were less likely to attend their postpartum appointment, but were just as likely to participate in postpartum glucose screening.74
Information on the effect of lactation on glucose tolerance are uncertain, and the metabolic effects of contraceptive hormones in breastfeeding women with GDM is unknown. Breastfeeding produces a relatively hypoestrogenic state in the postpartum period, and some data suggest that breastfeeding may decrease the long-term risk of T2DM in women with a history of GDM. Breastfeeding women have better lipid profiles, lower fasting and postprandial glucose levels, and greater insulin sensitivity in the early postpartum period.75
In women who develop T2DM with complications, the safety profile of hormonal contraception potentially change. DM alone, without vascular disease, is MEC category 1 or 2 for all contraceptive methods—no contraindications are present for any method. If patients were to develop nephropathy, retinopathy, neuropathy, or other vascular disease or have DM of > 20 years duration, DMPA becomes Category 3 and CHCs become Category 3 or 4 depending on the severity of the condition. This is due to the theoretical risk of reduction of HDL levels with DMPA, as previously discussed as well as the potential cardiovascular risks associated with estrogen-containing contraception.11,15 Other progestin-only and non-hormonal methods of contraception remain suitable for use in this population.
Contraceptive Efficacy And Safety In Obese Women
In addition to the concerns regarding discontinuation of hormonal contraception due to weight gain and the general negative effects of obesity, concerns have also been raised regarding contraceptive efficacy and safety in obese women. Since obesity is highly prevalent among women with GDM, the questions surrounding efficacy and safety impart particular interest. As the obesity epidemic has worsened over time, several recent research studies address contraceptive efficacy and obesity, especially since contraceptive studies historically excluded overweight or obese women. Obesity may affect the efficacy of hormonal contraception because of metabolic effects or greater body mass/body fat.76 Previous pharmacokinetic (PK) studies have shown that obesity affects the drug levels of hormonal contraceptives with varied impact on pharmacodynamics.77 Some research reports lower serum hormone concentrations with COCs and the contraceptive vaginal ring containing LNG and ethinyl estradiol in obese women.78,79 Additionally, obese women using COCs may experience a longer half-life and a longer time to reach steady-state than normal-weight women, which some postulate is a potential mechanism for contraceptive failure.80 However, data support that COCs produce the same degree of ovulation suppression in thin and obese women.81,82 A recent pharmacokinetic study using pooled data from four studies examining LNG-containing COCs demonstrated reduced systemic COC exposure in obese women, but did not show a difference in trough levels of either LNG or ethinyl estradiol. In women using COCs correctly, it would unlikely result in lower contraceptive efficacy.83
Other research has been directed at pregnancy rates. A 2016 Cochrane Review reported on 12 studies comparing pregnancy rates in overweight or obese women and normal-weight women. Most studies did not show a higher rate of pregnancy in overweight or obese women77 The majority of research examined COCs, and of the five studies, two found a relationship between BMI and pregnancy. One study of a pill containing norethindrone acetate and ethinyl estradiol showed a higher pregnancy rate in women with a BMI ≥ 25 (RR 2.49, 95% CI 1.01–6.13). However, this difference disappeared when the BMI cutoff was changed to 27.384 In contrast to this study, another trial evaluating a pill containing LNG and ethinyl estradiol reported more pregnancies in non-obese women as compared to obese women (Pearl index 5.59 [95% CI 0.70–10.47] vs zero).85 In addition, a meta-analysis of seven COC Phase 3 trials was published which showed a higher failure rates in obese women. The Pearl Indices were 3.14 and 2.53 for obese and normal-weight women, respectively (adjusted HR 1.44 [95% confidence interval (CI): 1.06–1.95; p=0.018]).86
An experimental transdermal patch containing levonorgestrel and ethinyl estradiol reported more pregnancies in obese women as compared to non-obese women who were treatment-compliant (Pear Index 4.63 [95% CI 0.10 to 9.17] versus 2.15 [95% CI 0.27 to 4.04]).85 Regarding the currently marketed transdermal contraceptive patch containing norelgestromin and ethinyl estradiol, an FDA review of data surrounding it the found that 33% of pregnancies occurred in a small subset of women whose baseline body weight was ≥ 90kg, with a significant association between baseline body weight and pregnancy (p < 0.001). Therefore, the package insert states that the transdermal patch may be less effective in women in this weight category.87,88 The conclusion that obese women can rely on the efficacy of hormonal contraception to prevent pregnancy is supported by a prospective cohort of 1,523 women using CHCs (pill, patch, ring) without a significant difference in pregnancy rates across BMI categories. Pregnancy rates were 8.44% for BMI < 25, (95% CI 6.1–11.5) 11.03% for BMI 25–30 (95% CI 7.5–16.0), and 8.92% for BMI > 30 (95% confidence interval 7.6–11.5).89
Other studies evaluating DMPA, LNG-IUS, the two-rod LNG implant, and the ENG implant showed no differences between groups.77 Although one study of the ENG implant showed that plasma concentrations of ENG were 48% lower in obese women, multiple larger studies did not show a difference in levels.90 Therefore, consideration for progestin-only methods in obese women should be given, especially given the increased risks of abnormal uterine bleeding and endometrial hyperplasia in obese women.15
Both the World Health Organization and the CDC MEC assign a Category 1 or 2 rating for all contraceptives for obese women (BMI >30). CHCs are considered a Category 2 for this group due to a concern regarding cardiovascular risks, such as acute myocardial infarction (MI), stroke, and venous thromboembolism (VTE). Few studies have looked at these outcomes. One study reported that the risk of stroke in CHC users did not change with BMI.91 There is conflicting evidence regarding risk of acute MI in obese women using CHCs, however the absolute risk of acute MI is low in reproductive aged-women regardless of BMI. It is known that obesity and CHC use are both independent risk factors for VTE. Obese women using CHC may be at a higher risk of VTE than normal-weight women, with a large systematic review suggesting that obese COC users had a 5–8 times higher risk of VTE than obese non-users and a 10-times higher rate than non-obese non-users.92 However, like the risk of acute MI, the absolute risk of VTE in an otherwise-healthy reproductive-aged population is small, and the risk of VTE in obese women during pregnancy and the postpartum period is much higher than while using CHC.15 Given the above-mentioned data, obese women using CHCs should be counseled that there may be an increased risk of VTE.90
Overall, high quality studies do not indicate an association between BMI and efficacy of most contraceptives, but the number of studies is small and further research is needed. In addition, hormonal contraception is safe to use without contraindication in an otherwise-healthy obese population with proper counseling regarding potential cardiovascular and VTE risks.
Contraceptive Recommendations And Future Health Implications Of Gestational Diabetes
The CDC MEC assigns a category 1 rating for patients with a history of GDM for all contraceptives. Although the available evidence supports this rating, the literature behind this recommendation is limited. Many studies describe effects over a short period of time (6–12 months) and may not account for long-term effect. Also, since institutions vary in their diagnostic criteria for GDM, there may be heterogeneity in the cohorts presented in the current literature. Additional directed studies in this population of women are needed.
Based on current evidence, women with past GDM are candidates for all hormonal and non-hormonal contraceptives, in the absence of other contraindications. As in all patients, recommendations for contraceptive use in these women should include consideration of medical co-morbidities, plans for subsequent pregnancies, acceptability, convenience, and non-contraceptive benefits.
Progestin-only pills are frequently prescribed for breastfeeding women. There is no theoretical or proven impact on breastmilk supply or infant development, and the absence of estrogen allows immediate postpartum initiation. Since progestin-only pills do not affect thromboembolism risk or lactation, they can be safely initiated immediately postpartum in breastfeeding and non-breastfeeding women. Similarly, progestin implant and IUDs can be safely used postpartum. IUD placement may occur immediately after delivery (post-placental insertion), or 4 to 6 weeks postpartum, without substantially increased risks of expulsion. IUD placement after 10 mins after delivery of the placenta up to the first 4 weeks postpartum (delayed postpartum insertion), can be considered, but expulsion rates are higher than acceptable in many clinical settings. Etonogestrel implants are safely used in lactating and non-lactating women at any time postpartum, and provide LARC benefits without the risk of expulsion associated with IUDs. Clinicians should consider LARC methods the first-line options in many women, based on their high effectiveness.
Given the limited data surrounding the impact of each contraceptive method on insulin sensitivity, glycemic control, lipid profiles, weight gain and long-term risk of T2DM, it is not possible to make a generalized recommendation for women with a history of GDM.
Instead, as with women without prior GDM, counseling should appropriately balance the patient’s knowledge of contraceptive options, past contraceptive use, beliefs surrounding contraception and future childbearing plans. Providers should counsel patients about the superior efficacy of LARC methods. Tubal sterilization is an option for women who no longer desire fertility, and should include consideration of potential surgical risks, especially in the setting of obesity or other conditions.
Women’s preferences for the different types of contraceptives and their contraceptive uptake have shifted in recent years. Older studies found that women with a history of GDM were more likely to choose tubal sterilization and less likely to choose DMPA.93 A more recent study showed that women with a history of GDM were more likely than the general population to use highly-effective, reversible contraception.73 The available data, albeit limited, suggests that all types of CHC are safe for women with a history of GDM.94–96
Counseling a woman about the implications of GDM on her future health and future pregnancies guides decision-making on contraceptive use and timing of subsequent pregnancies. Women should understand that GDM diagnosis in one pregnancy increases the risk of GDM in future pregnancies. In a cohort of 651 women with GDM, the rate of recurrence in the next pregnancy was 35.6%. In this particular study, maternal weight preceding her next pregnancy was predictive of recurrent GDM, with higher weight associated with greater risk.97
Postpartum care for women with GDM involves education about a diet and nutrition, exercise, and weight loss. Appropriate birth spacing with contraceptive use may help a woman reduce her subsequent risk of GDM by allowing her to return to a normal weight between pregnancies. Furthermore, GDM is a major risk factor for future insulin resistance and T2DM. In a large population study of 659,164 pregnant women, 3.3% had a diagnosis of GDM. Of those with GDM, the probability of developing T2DM was 3.7% within 9 months of delivery and 18.9% within 9 years.98
Providers must continually address contraception and reproductive health needs with patients over time. The best contraceptive at one time may no longer be ideal as a woman’s plans for childbearing and medical conditions change. In particular, women with GDM may develop T2DM, hypertension, or cardiovascular or other disorders, with which combined hormonal methods are contraindicated.
Directed counseling and comprehensive information on future health risks associated with GDM will support and motivate women to make healthy lifestyle modifications. Obstetrician-gynecologists and primary care providers should ensure that all women with receive ongoing diabetes screening, blood pressure monitoring, and weight reduction counseling. Postpartum referrals to weight loss programs and nutritionists may also be appropriate for some women.
Conclusion
Women with a history of GDM have specific needs when considering postpartum care and contraceptive management. Current consensus supports the safety of all contraceptive methods, but the evidence is incomplete. Women with GDM should be counseled on methods in a similar manner to those without the condition, considering effectiveness, acceptability, future childbearing plans, and non-contraceptive benefits. Some literature suggests adverse metabolic effects with use of systemic, progestin-only methods, but data are incomplete and findings are mixed. The overall risk of worsening lipid profiles, decreased insulin sensitivity, and the development of diabetes appears to be low and clinically insignificant in most women.
Future well-designed studies must evaluate the safety of hormonal contraception, particularly progestin-only contraception, in women with GDM. Also, with the recent increased popularity of immediate postpartum LARC in US hospitals, evaluation of the metabolic effects of progestin implants in the early postpartum period in women with GDM is warranted. Additional evaluation of the relationships between diabetes, bone mass, and contraception is necessary. Adequate postpartum glycemic control and pregnancy spacing are paramount in these women, and further research on best contraceptive practices are necessary.
Disclosure
Dr Kiley reports consulting fees from CVS Caremark, outside the submitted work. Dr Kiley serves as a consultant for CVS Caremark. This relationship does not present a conflict of interest with the current work. The authors report no other conflicts of interest in this work.
References
1. Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374(9):843–852. doi:10.1056/NEJMsa1506575
2. Kavanaugh MLJ. Jenna Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014. Contraception. 2018;97:1. doi:10.1016/j.contraception.2017.10.003
3. Chen I, Jhangri GS, Chandra S. Relationship between interpregnancy interval and congenital anomalies. Am J Obstet Gynecol. 2014;210(6):
4. Caughey AB, Chandrasekaran S. Short interpregnancy interval increases the risk of preterm premature rupture of membranes and early delivery AU - Shree, Raj. J Maternal-Fetal Neonatal Med. 2018;31(22):3014–3020. doi:10.1080/14767058.2017.1362384
5. Hanley GE, Hutcheon JA, Kinniburgh BA, Lee L. Interpregnancy interval and adverse pregnancy outcomes: an analysis of successive pregnancies. Obstetrics Gynecol. 2017;129(3):408–415. doi:10.1097/AOG.0000000000001891
6. Davis EM, Babineau DC, Wang X, et al. Short inter-pregnancy intervals, parity, excessive pregnancy weight gain and risk of maternal obesity. Matern Child Health J. 2014;18(3):554–562. doi:10.1007/s10995-013-1272-3
7. Practice Bulletin ACOG. No. 190: gestational Diabetes Mellitus. Obstetrics Gynecol. 2018;131(2):e49–e64. doi:10.1097/AOG.0000000000002501
8. Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25(10):1862–1868. doi:10.2337/diacare.25.10.1862
9. Kjos SL, Peters RK, Xiang A, Thomas D, Schaefer U, Buchanan TA. Contraception and the risk of type 2 Diabetes Mellitus in Latina women with prior gestational Diabetes Mellitus. Jama. 1998;280(6):533–538. doi:10.1001/jama.280.6.533
10. Peters RK, Xiang A, Kjos SL, Buchanan TA. Long-term diabetogenic effect of single pregnancy in women with previous gestational diabetes mellitus. Lancet. 1996;347(8996):227–230. doi:10.1016/S0140-6736(96)90405-5
11. Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep. 2016;65(No.RR–3):1–104. doi:http://dx.doi.org/10.15585/mmwr.rr6503a1
12. Sundaram A, Vaughan B, Kost K, et al. Contraceptive failure in the United States: estimates from the 2006-2010 national survey of family growth. Perspect Sex Reprod Health. 2017;49(1):7–16. doi:10.1363/psrh.12017
13. Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404. doi:10.1016/j.contraception.2011.01.021
14. Sober S, Schreiber CA. Postpartum contraception. Clin Obstet Gynecol. 2014;57(4):763–776. doi:10.1097/GRF.0000000000000055
15. Committee on Practice Bulletins—Gynecology. ACOG practice bulletin No. 206: use of hormonal contraception in women with coexisting medical conditions. Obstetrics Gynecol. 2019;133(2):e128–e150. doi:10.1097/AOG.0000000000003072
16. Clare C, Squire M-B, Alvarez K, Meisler J, Fraser C. Barriers to adolescent contraception use and adherence. Int J Adolesc Med Health. 2016;30(4). doi:10.1515/ijamh-2016-0098
17. Gallo MF, Lopez LM, Grimes DA, Carayon F, Schulz KF, Helmerhorst FM. Combination contraceptives: effects on weight. Cochrane Database Syst Rev. 2014;(1):CD003987.
18. Kim SY, England L, Wilson HG, Bish C, Satten GA, Dietz P. Percentage of gestational Diabetes Mellitus attributable to overweight and obesity. Am J Public Health. 2010;100(6):1047–1052. doi:10.2105/AJPH.2009.172890
19. Flegal KM, Troiano RP. Changes in the distribution of body mass index of adults and children in the US population. Int J Obesity Relat Metab Disorders. 2000;24(7):807. doi:10.1038/sj.ijo.0801232
20. Moore LL, Valuck R, McDougall C, Fink W. A comparative study of one-year weight gain among users of medroxyprogesterone acetate, levonorgestrel implants, and oral contraceptives. Contraception. 1995;52(4):215–219. doi:10.1016/0010-7824(95)00189-h
21. Rosenberg M. Weight change with oral contraceptive use and during the menstrual cycle: results of daily measurements. Contraception. 1998;58(6):345–349. doi:10.1016/s0010-7824(98)00127-9
22. Bonny AE, Secic M, Cromer BA. A longitudinal comparison of body composition changes in adolescent girls receiving hormonal contraception. J Adolesc Health. 2009;45(4):423–425. doi:10.1016/j.jadohealth.2009.04.009
23. Lopez LM, Ramesh S, Chen M, et al. Progestin‐only contraceptives: effects on weight. Cochrane Database Syst Rev. 2016;(8):CD008815.
24. Curtis KM, Ravi A, Gaffield ML. Progestogen-only contraceptive use in obese women. Contraception. 2009;80(4):346–354. doi:10.1016/j.contraception.2009.04.006
25. Merki-Feld GS, Skouby S, Serfaty D, et al. European Society of contraception statement on contraception in obese women. Eur J Contraception Reprod Health Care. 2015;20(1):19–28. doi:10.3109/13625187.2014.960561
26. Mody SK, Han M. Obesity and contraception. Clin Obstet Gynecol. 2014;57(3):501–507. doi:10.1097/GRF.0000000000000047
27. Nyirati CM, Habash DL, Shaffer LET. Weight and body fat changes in postpartum depot-medroxyprogesterone acetate users. Contraception. 2013;88(1):169–176. doi:10.1016/j.contraception.2012.10.016
28. Natália Dal’Ava LB, Valeria Bahamondes M, Allan de Oliveira S, Ilza M. Body weight and composition in users of levonorgestrel-releasing intrauterine system. Contraception. 2012;86(4):350–353. doi:10.1016/j.contraception.2012.01.017
29. Vickery Z, Madden T, Zhao Q, Secura GM, Allsworth JE, Peipert JF. Weight change at 12 months in users of three progestin-only contraceptive methods. Contraception. 2013;88(4):503–508. doi:10.1016/j.contraception.2013.03.004
30. Modesto W, de Nazare Silva Dos Santos P, Correia VM, Borges L, Bahamondes L. Weight variation in users of depot-medroxyprogesterone acetate, the levonorgestrel-releasing intrauterine system and a copper intrauterine device for up to ten years of use. Eur J Contracept Reprod Health Care. 2015;20(1):57–63. doi:10.3109/13625187.2014.951433
31. Ball MJ, Ashwell E, Gillmer MD. Progestagen-only oral contraceptives: comparison of the metabolic effects of levonorgestrel and norethisterone. Contraception. 1991;44(3):223–233. doi:10.1016/0010-7824(91)90014-7
32. Napolitano A, Zanin R, Palma F, et al. Body composition and resting metabolic rate of perimenopausal women using continuous progestogen contraception. Eur J Contracept Reprod Health Care. 2016;21(2):168–175. doi:10.3109/13625187.2015.1079610
33. Silva Dos Santos P, Madden T, Omvig K, Peipert JF. Changes in body composition in women using long-acting reversible contraception. Contraception. 2017;95(4):382–389. doi:10.1016/j.contraception.2016.12.006
34. Modesto W, Dal´Ava N, Monteiro I, Bahamondes L. Body composition and bone mineral density in users of the etonogestrel-releasing contraceptive implant. Arch Gynecol Obstet. 2015;292(6):1387–1391. doi:10.1007/s00404-015-3784-0
35. Klipping C, Marr J. Effects of two combined oral contraceptives containing ethinyl estradiol 20 μg combined with either drospirenone or desogestrel on lipids, hemostatic parameters and carbohydrate metabolism. Contraception. 2005;71(6):409–416. doi:10.1016/j.contraception.2004.12.005
36. Sitruk-Ware R, Nath A. Metabolic effects of contraceptive steroids. Rev Endocr Metab Disord. 2011;12(2):63. doi:10.1007/s11154-011-9182-4
37. Gaspard U, Endrikat J, Desager JP, Buicu C, Gerlinger C, Heithecker R. A randomized study on the influence of oral contraceptives containing ethinylestradiol combined with drospirenone or desogestrel on lipid and lipoprotein metabolism over a period of 13 cycles. Contraception. 2004;69(4):271–278. doi:10.1016/j.contraception.2003.11.003
38. Lobo RA, Skinner JB, Lippman JS, Cirillo SJ. Plasma lipids and desogestrel and ethinyl estradiol: a meta-analysis**Supported by a grant from Ortho-McNeil Pharmaceutical Corporation, Raritan, New Jersey. Fertil Steril. 1996;65(6):1100–1109.
39. Mahnaz Shahnazi AF-K, Pourzeinali-Beilankouh S, Sadrimehr F. Effects of second and third generation oral contraceptives on lipid and carbohydrate metabolism in overweight and obese women: a randomized triple-blind controlled trial. Iran Red Crescent Med J. 2016;18(9):e36982. doi:10.5812/ircmj.36982
40. Tuppurainen M, Klimscheffskij R, Venhola M, Dieben TOM. The combined contraceptive vaginal ring (NuvaRing®) and lipid metabolism: a comparative study. Contraception. 2004;69(5):389–394. doi:10.1016/j.contraception.2004.01.004
41. Young RL, DelConte A. Effects of low-dose monophasic levonorgestrel with ethinyl estradiol preparation on serum lipid levels: a twenty-four month clinical trial. Am J Obstet Gynecol. 1999;181(5, Supplement):S59–S62. doi:10.1016/S0002-9378(99)70365-0
42. Barkfeldt J, Virkkunen A, Dieben T. The effects of two progestogen-only pills containing either desogestrel (75 μg/day) or levonorgestrel (30 μg/day) on lipid metabolism☆☆This study was sponsored by NV Organon, Oss, The Netherlands. Contraception. 2001;64(5):295–299. doi:10.1016/s0010-7824(01)00269-4
43. Binod KY, Rajesh KG, Prajwal G, et al. Effects of long-term use of depo-medroxyprogesterone acetate on lipid metabolism in Nepalese women. Korean J Lab Med. 2011;31(2):95–97. doi:10.3343/kjlm.2011.31.2.95
44. Berenson AB, Rahman M, Wilkinson G. Effect of injectable and oral contraceptives on serum lipids. Obstetrics Gynecol. 2009;114(4):786–794. doi:10.1097/AOG.0b013e3181b76bea
45. Taneepanichskul S, Reinprayoon D, Jaisamrarn U. Effects of DMPA on weight and blood pressure in long term acceptors. Contraception. 1999;59(5):301–303. doi:10.1016/s0010-7824(99)00037-2
46. Westhoff C. Depot medroxyprogesterone acetate contraception. metabolic parameters and mood changes. J Reprod Med. 2006;41(5):401–406.
47. Guazzelli CAF, de Queiroz FT, Barbieri M, Barreiros FA, Torloni MR, Araujo FF. Metabolic effects of contraceptive implants in adolescents. Contraception. 2011;84(4):409–412. doi:10.1016/j.contraception.2011.02.006
48. Dilbaz B, Ozdegirmenci O, Caliskan E, Dilbaz S, Haberal A. Effect of etonogestrel implant on serum lipids, liver function tests and hemoglobin levels. Contraception. 2010;81(6):510–514. doi:10.1016/j.contraception.2010.01.014
49. Bender NM, Segall-Gutierrez P, Najera SOL, Stanczyk FZ, Montoro M, Mishell DR. Effects of progestin-only long-acting contraception on metabolic markers in obese women. Contraception. 2013;88(3):418–425. doi:10.1016/j.contraception.2012.12.007
50. Ng YW, Liang S, Singh K. Effects of Mirena (levonorgestrel-releasing intrauterine system) and Ortho Gynae T380 intrauterine copper device on lipid metabolism—a randomized comparative study. Contraception. 2009;79(1):24–28. doi:10.1016/j.contraception.2008.07.012
51. Graff-Iversen S, Tonstad S. Use of progestogen-only contraceptives/medications and lipid parameters in women age 40 to 42 years: results of a population-based cross-sectional Norwegian Survey. Contraception. 2002;66(1):7–13. doi:10.1016/s0010-7824(02)00311-6
52. Kayikcioglu F, Gunes M, Ozdegirmenci O, Haberal A. Effects of levonorgestrel-releasing intrauterine system on glucose and lipid metabolism: a 1-year follow-up study. Contraception. 2006;73(5):528–531. doi:10.1016/j.contraception.2005.12.005
53. Hedderson MM, Ferrara A, Williams MA, Holt VL, Weiss NS. Androgenicity of progestins in hormonal contraceptives and the risk of gestational Diabetes Mellitus. Diabetes Care. 2007;30(5):1062–1068. doi:10.2337/dc06-2227
54. Godsland IF, Crook D, Simpson R, et al. The effects of different formulations of oral contraceptive agents on lipid and carbohydrate metabolism. N Engl J Med. 1990;323(20):1375–1381. doi:10.1056/NEJM199011153232003
55. Godsland IF, Walton C, Felton C, Proudler A, Patel A, Wynn V. Insulin resistance, secretion, and metabolism in users of oral contraceptives. J Clin Endocrinol Metab. 1992;74(1):64–70. doi:10.1210/jcem.74.1.1530790
56. Perlman JA, Russell-Briefel R, Ezzati T, Lieberknecht G. Oral glucose tolerance and the potency of contraceptive progestins. J Chronic Dis. 1985;38(10):857–864. doi:10.1016/0021-9681(85)90110-9
57. Bastianelli C, Farris M, Rosato E, Brosens I, Benagiano G. Pharmacodynamics of combined estrogen-progestin oral contraceptives: 1. Effects on metabolism. Expert Rev Clin Pharmacol. 2017;10(3):315–326. doi:10.1080/17512433.2017.1271708
58. Bonds DE, Lasser N, Qi L, et al. The effect of conjugated equine oestrogen on diabetes incidence: the women’s health initiative randomised trial. Diabetologia. 2006;49(3):459–468. doi:10.1007/s00125-005-0096-0
59. Kim C, Siscovick DS, Sidney S, Lewis CE, Kiefe CI, Koepsell TD. Oral contraceptive use and association with glucose, insulin, and diabetes in young adult women. CARDIA Study. 2002;25(6):1027–1032.
60. Lopez LM, Grimes DA, Schulz KF. Steroidal contraceptives: effect on carbohydrate metabolism in women without diabetes mellitus. Cochrane Database Syst Rev. 2014;18(4):CD00613.
61. Kim C, Seidel KW, Begier EA, Kwok YS. Diabetes and depot medroxyprogesterone contraception in Navajo women. Arch Intern Med. 2001;161(14):1766–1771. doi:10.1001/archinte.161.14.1766
62. Fahmy K, Abdel-Razik M, Shaaraway M, et al. Effect of long-acting progestagen-only injectable contraceptives on carbohydrate metabolism and its hormonal profile. Contraception. 1991;44(4):419–430. doi:10.1016/0010-7824(91)90032-b
63. Oderich CL, Wender MCO, Lubianca JN, Santos LM, de Mello GC. Impact of etonogestrel-releasing implant and copper intrauterine device on carbohydrate metabolism: a comparative study. Contraception. 2012;85(2):173–176. doi:10.1016/j.contraception.2011.05.018
64. Villas-Boas J, Vilodre LC, Malerba H, Pontremoli Salcedo M, Foresti Jiménez M, El Beitune P. Metabolic safety of the etonogestrel contraceptive implant in healthy women over a 3-year period. Eur J Obstetrics Gynecol Reprod Biol. 2016;202:51–54. doi:10.1016/j.ejogrb.2016.04.025
65. Raudaskoski T, Tomas C, Laatikainen T. Insulin sensitivity during postmenopausal hormone replacement with transdermal estradiol and intrauterine levonorgestrel. Acta Obstet Gynecol Scand. 1999;78(6):540–545.
66. Rogovskaya SM, Rivera R, Grimes DA, et al. Effect of a levonorgestrel intrauterine system on women with type 1 diabetes: a randomized trial. Obstetrics Gynecol. 2005;105(4):811–815. doi:10.1097/01.AOG.0000156301.11939.56
67. Committee Opinion No. 602. Depot medroxyprogesterone acetate and bone effects. Obstet Gynecol. 2014;123(6):1398–1402. doi:10.1097/01.AOG.0000450758.95422.c8
68. Moayeri A, Mohamadpour M, Mousavi SF, Shirzadpour E, Mohamadpour S, Amraei M. Fracture risk in patients with type 2 diabetes mellitus and possible risk factors: a systematic review and meta-analysis. Ther Clin Risk Manag. 2017;13:455–468. doi:10.2147/TCRM.S131945
69. Nelson AL, Le MHH, Musherraf Z, VanBerckelaer A. Intermediate-term glucose tolerance in women with a history of gestational diabetes: natural history and potential associations with breastfeeding and contraception. Am J Obstet Gynecol. 2008;198(6):
70. Xiang AH, Kawakubo M, Kjos SL, Buchanan TA. Long-acting injectable progestin contraception and risk of type 2 diabetes in latino women with prior gestational Diabetes Mellitus. Diabetes Care. 2006;29(3):613–617. doi:10.2337/diacare.29.03.06.dc05-1940
71. Skouby SO, Mølsted-Pedersen L, Kosonen A. Consequences of intrauterine contraception in diabetic women**The study of the corrosion investigations was supported by the Schering company. Fertil Steril. 1984;42(4):568–572.
72. Kiley JW, Hammond C, Niznik C, Rademaker A, Liu D, Shulman LP. Postpartum glucose tolerance in women with gestational diabetes using levonorgestrel intrauterine contraception. Contraception. 2015;91(1):67–70. doi:10.1016/j.contraception.2014.08.004
73. Schwarz EB, Braughton MY, Riedel JC, et al. Postpartum care and contraception provided to women with gestational and preconception diabetes in California’s Medicaid program. Contraception. 2017;96(6):432–438. doi:10.1016/j.contraception.2017.08.006
74. Rosenthal EW, Easter SR, Morton-Eggleston E, Dutton C, Zera C. Contraception and postpartum follow-up in patients with gestational diabetes. Contraception. 2017;95(4):431–433. doi:10.1016/j.contraception.2016.11.001
75. Gunderson EP. Impact of breastfeeding on maternal metabolism: implications for women with gestational diabetes. Curr Diab Rep. 2014;14(2):460. doi:10.1007/s11892-014-0475-3
76. Grimes DA, Shields WC. Family planning for obese women: challenges and opportunities. Contraception. 2005;72(1):1–4. doi:10.1016/j.contraception.2005.04.002
77. Lopez LM, Bernholc A, Chen M, et al. Hormonal contraceptives for contraception in overweight or obese women. Cochrane Database Syst Rev. 2016;18(8):CD008452.
78. Westhoff CL, Torgal AH, Mayeda ER, Pike MC, Stanczyk FZ. Pharmacokinetics of a combined oral contraceptive in obese and normal-weight women. Contraception. 2010;81(6):474–480. doi:10.1016/j.contraception.2010.01.016
79. Westhoff CL, Pike MC, Tang R, DiNapoli MN, Sull M, Cremers S. Estimating systemic exposure to ethinyl estradiol from an oral contraceptive. Am J Obstet Gynecol. 2015;212(5):614e611–617. doi:10.1016/j.ajog.2014.12.007
80. Edelman AB, Cherala G, Munar MY, et al. Prolonged monitoring of ethinyl estradiol and levonorgestrel levels confirms an altered pharmacokinetic profile in obese oral contraceptives users. Contraception. 2013;87(2):220–226. doi:10.1016/j.contraception.2012.10.008
81. Westhoff CL, Torgal AH, Mayeda ER, et al. Ovarian suppression in normal-weight and obese women during oral contraceptive use: a randomized controlled trial. Obstet Gynecol. 2010;116(2 Pt 1):275–283. doi:10.1097/AOG.0b013e3181e79440
82. Westhoff CL, Torgal AH, Mayeda ER, et al. Pharmacokinetics and ovarian suppression during use of a contraceptive vaginal ring in normal-weight and obese women. Am J Obstet Gynecol. 2012;207(1):39 e31–36. doi:10.1016/j.ajog.2012.04.022
83. Luo D, Westhoff CL, Edelman AB, Natavio M, Stanczyk FZ, Jusko WJ. Altered pharmacokinetics of combined oral contraceptives in obesity - multistudy assessment. Contraception. 2019;99(4):256–263. doi:10.1016/j.contraception.2018.12.009
84. Burkman RT, Fisher AC, Wan GJ, Barnowski CE, LaGuardia KD. Association between efficacy and body weight or body mass index for two low-dose oral contraceptives. Contraception. 2009;79(6):424–427. doi:10.1016/j.contraception.2008.12.013
85. Kaunitz AM, Portman D, Westhoff CL, et al. Low-dose levonorgestrel and ethinyl estradiol patch and pill: a randomized controlled trial. Obstet Gynecol. 2014;123(2 Pt 1):295–303. doi:10.1097/AOG.0000000000000095
86. Yamazaki M, Dwyer K, Sobhan M, et al. Effect of obesity on the effectiveness of hormonal contraceptives: an individual participant data meta-analysis. Contraception. 2015;92(5):445–452. doi:10.1016/j.contraception.2015.07.016
87. Edelman A, Trussell J, Aiken ARA, Portman DJ, Chiodo JA
88. Zieman M, Guillebaud J, Weisberg E, Shangold GA, Fisher AC, Creasy GW. Contraceptive efficacy and cycle control with the Ortho Evra/Evra transdermal system: the analysis of pooled data. Fertil Steril. 2002;77(2 Suppl 2):S13–18. doi:10.1016/s0015-0282(01)03275-7
89. McNicholas C, Zhao Q, Secura G, Allsworth JE, Madden T, Peipert JF. Contraceptive failures in overweight and obese combined hormonal contraceptive users. Obstet Gynecol. 2013;121(3):585–592. doi:10.1097/AOG.0b013e31828317cc
90. Simmons KB, Edelman AB. Hormonal contraception and obesity. Fertil Steril. 2016;106(6):1282–1288. doi:10.1016/j.fertnstert.2016.07.1094
91. Schwartz SM, Petitti DB, Siscovick DS, et al. Stroke and use of low-dose oral contraceptives in young women: a pooled analysis of two US studies. Stroke. 1998;29(11):2277–2284. doi:10.1161/01.str.29.11.2277
92. Horton LG, Simmons KB, Curtis KM. Combined hormonal contraceptive use among obese women and risk for cardiovascular events: a systematic review. Contraception. 2016;94(6):590–604. doi:10.1016/j.contraception.2016.05.014
93. Beydoun HA, Beydoun MA, Tamim H. How does gestational diabetes affect postpartum contraception in nondiabetic primiparous women? Contraception. 2009;79(4):290–296. doi:10.1016/j.contraception.2008.10.013
94. Damm P, Mathiesen ER, Petersen KR, Kjos S. Contraception After Gestational Diabetes. Diabetes Care. 2007;30(Supplement 2):S236–S241. doi:10.2337/dc07-s222
95. Kjos SL, Shoupe D, Douyan S, et al. Effect of low-dose oral contraceptives on carbohydrate and lipid metabolism in women with recent gestational diabetes: results of a controlled, randomized, prospective study. Am J Obstet Gynecol. 1990;163(6, Part 1):1822–1827. doi:10.1016/0002-9378(90)90757-x
96. Skouby SO, Kühl C, Mølsted-Pedersen L, Petersen K, Christensen MS. Triphasic oral contraception: metabolic effects in normal women and those with previous gestational diabetes. Am J Obstet Gynecol. 1985;153(5):495–500. doi:10.1016/0002-9378(85)90460-0
97. MacNeill S, Dodds L, Hamilton DC, Armson BA, VandenHof M. Rates and risk factors for recurrence of gestational diabetes. Diabetes Care. 2001;24(4):659–662. doi:10.2337/diacare.24.4.659
98. Feig DS, Zinman B, Wang X, Hux JE. Risk of development of diabetes mellitus after diagnosis of gestational diabetes. Cmaj. 2008;179(3):229–234. doi:10.1503/cmaj.080012
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

