Back to Journals » Open Access Journal of Contraception » Volume 11
Contraceptive Demand, Utilization and Associated Factors Among University Female Students in Amhara Region, Ethiopia: Institution-Based Cross-Sectional Study
Authors Simegn A, Tiruneh D , Seid T, Ayalew F
Received 18 June 2020
Accepted for publication 21 August 2020
Published 9 October 2020 Volume 2020:11 Pages 157—165
DOI https://doi.org/10.2147/OAJC.S267966
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Amare Simegn, Dawit Tiruneh, Tigist Seid, Florence Ayalew
Department of Midwifery, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
Correspondence: Amare Simegn Email [email protected]
Background: Worldwide, university students fall in the youth group which is prone to unattended sexual risks, including unintended pregnancies and sexually transmitted diseases. One of the key strategies to prevent these problems is to use contraceptives. Therefore, the study was aimed at assessing contraceptive utilization and factors hindering their utilization.
Objective: The objective of the study was to assess contraceptive demand, utilization, and associated factors among university female students in Amhara region, Ethiopia.
Methods: An institution-based cross-sectional study was conducted. From seven universities, three of them were randomly selected. A multistage sampling method was used. Finally, a simple random sampling method was used to select the respondents. Data were entered via Epi-data version 3.1 and exported to SPSS version 20 for analysis. Bivariable and multivariable logistic regression analyses were employed. Results are presented using text, tables, and graphs.
Results: A total of 1276 respondents participated in the study with a response rate of 98.8%. The median age of the participants is 21.37 years (SD=1.88 years). About 398 (31.2%) of the respondents had sexual intercourse within the last 12 months. However, only 207 (16.2%) of the respondents were currently using contraceptives. Marital status, year of study, history of having information and previous discussion on contraceptives were found to be significantly associated. Married participants had a 94.4% lower contraceptive utilization compared with unmarried participants [0.056 (0.03– 0.12)]. Third year students were 50% less likely to use contraceptives compared to 2nd year students [0.50 (0.30– 0.82)]. Those having previous information on contraceptives [7.7 (1.01– 59.8)] and discussions with someone else [2.3 (1.5– 3.6)] were 7.7- and 2.3-times more likely to use contraceptives than their counterparts, respectively.
Conclusion: Contraceptive utilization among university female students is low. For students, new information, education and communication strategies for sexual and reproductive health issues should be launched.
Keywords: Demand, utilization, factors, females, students
Introduction
Worldwide, university students fall in the youth group which is prone to unattended sexual risk behaviors. This may lead to unwanted pregnancies and other sexually transmitted infections (STIs), which are contemporary public health concerns among University students.1–5 Though these problems are the most important public health problems, they are still prevalent. In a study among students in 42 universities in China, there was sexual intercourse among 10.2% of the students. Of whom, 31.8% had unintended pregnancy and 53.5% experienced two or more abortions.6 Similarly, there was a finding in Nigeria, which shows a 17% unwanted pregnancy and 51% induced abortion rates.7
In Ethiopia, the rate of abortion among students was found to be 6.5%, making it 3-fold the national rate of abortion for Ethiopia (23/1000 women aged 15–44).8 In Wolaita Sodo university, southern Ethiopia, a rate of 32.4% unintended pregnancy was found.9
One of the key strategies to prevent these problems is the availability and utilization of contraceptives.10 Countries in the world designed and used different strategies to effectively enhance the utilization of sexual and reproductive health services like contraceptives. But, especially in most African countries, the utilization of contraceptives is still less than 40%.11–13 Looking at the status of utilization of different countries, South Africa declared that 79% of students used contraceptives.14 Likewise, Uganda (46.6%),15 Lesotho (78%),16 Canada (75%),17 Nigeria (15.6%),18 Dilla, Ethiopia (64.5%),19 and Tanzania (47.4%)20 students used contraceptives. Hence, different factors were also drawn from different studies, like the Students’ academic year, having Pocket money, being married and those who had ever discussed modern family planning methods were more likely to use modern family planning as compared to their counterparts.15,17,21
Our country, Ethiopia, had designed a “Reproductive Health Strategy” which identifies six priority areas including fertility and family planning, HIV/AIDS, and reproductive health of young people to improve the reproductive health of the younger segment of the population.22
Despite these and other similar efforts, sexual and reproductive problems of youth, including students, prevail in the country. Evidence stresses that there is a need for reproductive health services.23,24
Hence, as far as our strong effort is concerned to search for different literatures in this regard, no research puts clear magnitude and factors that inhibit contraceptive utilization among university students in the region. Therefore, this study was designed to assess the magnitude and factors inhibiting contraceptive utilization among university female students.
General Objective
The main objective of the study was to assess contraceptive demand, utilization, and associated factors among university female students in Amhara region in 2018.
Specific Objectives
- To determine contraceptive demand among university female students in Amhara Region.
- To calculate contraceptive utilization among university female students in Amhara Region.
- To identify associated factors for contraceptive utilization among university female students in Amhara Region.
Methods
Study Design and Period
A facility-based cross-sectional study was conducted from April 2018 to June 2018 in the selected universities.
Study Area and Subjects
Amhara is one of the nine ethnic divisions of Ethiopia, containing the homeland of the Amhara people. Previously known as Region 3, its capital is Bahir Dar. The region had seven functional universities at the time of the inception of the project. There are 19 hospitals, 801 health centers, and 3302 in the region. Debre Tabor University, Bahir Dar University, and Debre Berhan University were the three randomly selected universities. The total number of female students in these randomly selected universities is 26,378.
Source Population
All female students in all universities were the source populations in the region.
Study Population
The study population includes all female students in randomly selected universities from the region.
Inclusion Criteria
All female university students in the region and staying for at least 1 year in university.
Exclusion Criteria
Extension students, those with disability (deafness), and critically ill at the time of data collection were purposely excluded from the study.
Sample Size and Sampling Procedures
A single population proportion formula was used to determine the required sample size and the assumptions are: P=50% (no previous studies done on demand for contraceptive among university students), Level of significance (α=5%), Marginal error (D=4%), Non-response rate=10%, and Design effect=2. Then, the total sample size calculated using Open Epi is 1291. Sample size was calculated for both the factors and the dependent variables, and the larger was taken.
Sampling Technique
Multistage sampling was used. First, from the seven universities found in the region, three of them were randomly selected. Proportionate sampling was used to select the study participants. There were 3527, 8947, and 13,904 female students at Debre Tabor University, Debre Berhan University, and Bahir Dar University, respectively. Second, the faculties in each university were considered and proportional to the size allocation method used to determine the number of participants in the faculties too. Therefore, 173 students in Debre Tabor University, 438 in Debre Berhan University, and 680 students in Bahir Dar University were selected. Finally, a simple random sampling method was used to select the study participants (Figure 1).
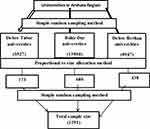 |
Figure 1 Schematic presentation of the sampling procedure for university female students. |
Variables of the Study
Dependent Variable
- Contraceptive demand
- Contraceptive utilization
Independent Variables
- Socio-demographic
- Economic variables
- Sexual behaviors
- Information/awareness on contraceptives
Operational Definition
Contraceptive Utilization
- Ever use: A condition in which the students had a history of utilization of contraception at least once in the past.
- Current use: The use of any method of contraception within the last 12 months.
Contraceptive Demand
A condition in which students have been exposed for sexual intercourse and may or may not use contraceptives. This is the total met and unmet need.
Meet Need
While students are exposed for penetrative sexual intercourse, and they used any contraceptive methods.
Unmet Need
While students are exposed for penetrative sexual intercourse, and they did not use any contraceptives, excluding those planning to get pregnant.
Data Collection Tools and Procedures
A structured self-administered questionnaire was used to collect the data. The data were collected through tools of both Amharic and English versions depending on the need of the participants so that the questionnaire was prepared in both versions. The questionnaire encompasses socio-demographic characteristics, sexual history of the respondents, and awareness on contraceptives, contraceptive utilization, and demand. The data were collected by 10 health professionals working in the university.
Data Quality Control
To improve the quality of the data, the data collectors were trained for 3 days on the whole processes of the data collection. Pre-testing of the tool was conducted at the University of Gondar. Hence, all necessary modifications on the questionnaire and data collection procedures was taken accordingly. The tools were translated from English language to local (Amharic) language and back to English language by an expert (PhD fellow in English language) to maintain consistency of the questionnaire.
Data Processing and Analysis
All filled questionnaires were checked for completeness and consistency, cleaned manually, coded and entered into EPI-DATA version 3.1 statistical software, and then exported to SPSS windows version 20 for analysis. Frequencies and summary statistics were used to describe the study populations in relation to relevant variables and presented using text, tables, and graphs. Binary logistic regression analysis was fit to identify factors associated with contraceptive utilization. Odds ratio with 95% confidence interval and P-value<0.05 were computed to declare statistical significance.
Results
Socio Demographic Characteristics of Study Participants
A total of 1276 respondents participated in the study with a response rate of 98.8%. The median age of the participants was 21.37 years (SD=1.88 years). More than two thirds (68.2%) of the participants were single. Almost all (95.9%) of the participants lived in their respective campus. Regarding the religion of the participants, 1098 (86.1%) was Orthodox. More than half (53%) of the respondents were born in the urban area (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Female University Students, 2018 |
Awareness of the Participants on Contraceptives
Of the total participants, 1164 (91.2%) of them had heard of at least one method of contraception. Among these, 925 (72.5%) of them were aware of injectables (Figure 2). Seven hundred and thirty-eight (57.8%) of the participants had discussed at least one method of contraceptive previously. The majority (34.5%) of them discussed this with their classmates. Besides, 1124 (88.1%) of the participants knew where to get contraceptives. Of these, 895 (70.1%) and 676 (53.0%) of the participants believed that contraceptives can be found in the health institution and public pharmacies, respectively. About 96.3% of the participants had also heard about sexually transmitted diseases. Even though 991 (77.7%) of the participants knew that condoms can prevent both pregnancy and STIs, there were respondents who responded that hormonal methods (8.5%) and injectables (7.0%) can prevent STIs.
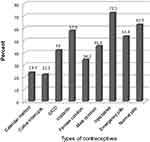 |
Figure 2 Awareness on contraceptives among university female students in Amhara region, 2018. |
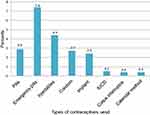 |
Figure 3 Contraceptives use within the last 12 months among university female students in Amhara region, 2018. |
Contraceptive Demand, Utilization, and Sexual History of the Respondents
Four hundred and seventy-eight (37.5%) of the participants had ever had sexual intercourse, while 398 (83.6%) of them had sexual intercourse within the last 12 months. Despite the presence of higher sexual activity, only 297 (23.3%) were ever users of contraceptives, while 207 (16.2%) of the participants were current users.
As shown in Figure 3, 150 (11.8%) of the participants used emergency pills and 116 (9.1%) used injectables. But, emergency pills (7.4%) were the leading contraceptive method used for those using within the last 12 weeks.
Source of Contraceptive Methods
Around 1124 (88.1%) students were aware of the source of contraceptive methods. Of the total respondents, 895 (70.1%) said contraceptives are obtained from public health institutions, 642 (50.3%) from a private clinic, 676 (53%) from a pharmacy, 314 (24.6) from university clinics, and 11 (0.6%) from another source.
Future Needs and Reasons Not to Use Contraceptives Among the Students
Around 892 (69.9%) of the students want to use a contraceptive method in the future. Fear of side-effects (28%), fear of community (34%), and no clinic within the campus (16%) were the major reasons for the students not to use contraceptive methods.
Factors Associated with Contraceptive Use
Associations found to be statistically significant in the bivariate analysis at a P-value less than 0.2 were included in the multivariable analysis to determine which factors best explain or predict the practice of contraceptive utilization. Backward logistic analysis was used to eliminate the confounders.
In a multivariable logistic regression analysis; marital status, having information for contraceptives, year of study and discussion with family members and others were significantly associated with contraceptive utilization.
Married participants had a 94.4% lower contraceptive utilization compared with unmarried participants [AOR (95% CI)=0.056 (0.03–0.12)]. Similarly, separated participants had a 90.6% lower contraceptive utilization as compared with unmarried participants [AOR (95% CI)=0 0.094 (0.04–0.22)] and divorced participants were 84% lower contraceptive utilization when compared with unmarried participants [AOR (95% CI)=0.16 (0.03–0.75)].
The year of study shows a significant association with contraceptive utilization. Third, fourth, and fifth year students had 50%, 62%, and 82% lower contraceptive utilization compared to 2nd year students [AOR (95% CI)=0.50 (0.30–0.82), 0.38 (0.18–0.82), and 0.18 (0.08–0.41)], respectively. Students who heard information about contraceptive methods had 7-times higher contraceptive utilization compared to students who did not hear information [AOR (95% CI)=7.77 (1.01–59.84)]. Students who discussed contraceptive methods with family members had 2-times higher contraceptive utilization compared to their counterparts [AOR (95% CI)=2.33 (1.49– 3.64)] (Table 2).
 |
Table 2 Bivariable and Multivariable Analysis of Factors Associated with Contraceptive Use Among University Female Students in Amhara Region, Ethiopia, 2018 |
Discussion
Utilization of contraceptive methods is one of the most important strategies to prevent maternal and perinatal morbidity and mortality, thereby improving the quality-of-life of the people, especially in developing countries. In our study, 478 (37.5%) of the participants had ever had sexual intercourse, while 398 (31.2%) of them had sexual intercourse within the last 12 months. Despite the presence of higher sexual activity, only 297 (23.3%) were ever users of contraceptives, while 207 (16.2%) of the participants were current users.
This finding is consistent with a study done at Dilla University in Ethiopia25 and Nigeria.26
However, a study done at Asaita in Afar Regional State, Ethiopia revealed that 68.4% were currently using modern family planning methods. This discrepancy could be attributed to women’s good awareness about family planning methods in Asaita town.21 Similarly, it is lower than a study conducted among Canada, outh Africa, Uganda, Lesotho, and Tanzania students, which was 79%, 77.1%, 46.6%, 55.3%, and 47.4%, respectively.27–31 This might be due to the difference in socio-economic status and age gap between them. But it is higher than a study conducted among Nigerian students which was 15.6%.26
Different determining factors were found to be associated with utilization of contraceptives. The odds of using modern contraceptives among married students were lower compared to single/unmarried students. This is consistent with the Study in Tanzania.31
Marital status, having prior information, year of study and discussion with family members and others were statistically associated with contraceptive utilization. This is similar to the study done in Adama, Ethiopia.10
Students who had heard information about contraceptive methods had 7-times higher contraceptive utilization when compared with students who did not hear any information [AOR (95% CI)=7.77 (1.11–59.8)]. On top of this, students who discussed about modern family planning methods with their family members were more likely to use contraceptive methods compared to those who did not discuss with their family. This is in line with other research.21 In addition, this is a similar finding to a finding in Arba Minch, Ethiopian undergraduates, in that students having prior information about contraceptives were more likely to the methods.32 This might be due to the fact that discussion about family planning methods might be associated with the use of contraceptive methods.
Second year students were more likely to use contraceptives than 3rd, 4th, and 5th year students. This is consistent with the finding among female University students in Uganda.30
The study has its own strengths and limitations. A random sampling method was used, having a representative high sample size to increase the precision of the study. The study design was cross-sectional so that the study does not allow for making assumptions surrounding causal effects between the relationships. Despite many efforts in minimizing bias, like preparing self-administered questionnaire, social desirability bias might be the possible source of bias that might affect the result of the study.
Conclusion
Contraceptive utilization among university female students is low. Quality sexual and reproductive health information and education for these segments of students might be important. The universities in the country could consider the information to share with the students via incorporating the issues in the curricula.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; SD, standard deviation; STDs, sexually transmitted diseases; SPSS, Statistical Package Software for Social Sciences; WHO, World Health Organizations.
Data Sharing Statement
In case of a reasonable request, the data is available from the corresponding author.
Ethical Issues and Consent to Participate
The study was conducted following the Declaration of Helsinki. It was reviewed and approved by the ethical review committee of Debre Tabor University with ref. No. of RP/415/18 as its ethically sound, a non-clinical trial research. Hence, ethical clearance was obtained from the ethical review committee of the university. Formal letter of permission was secured from the deans of the respective faculty. The purpose of the research was explained to the study participants and written informed consent was received from each study participant. Confidentiality and privacy were also maintained throughout the study in that no name was recorded on the questionnaire and the collected data were kept using computer password. The participants were informed that participation in the study was based on their volunteer status.
Acknowledgment
Our gratitude goes to Debre Tabor University for giving us the ethical clearance. The authors also thank university deans and other administrative staff for their cooperative support during the implementation of the research. We also acknowledge the supervisors, data collectors, and the respondents for their invaluable support.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. Besides, all authors agreed on the journal to which the article is sent and processed for publication, agreed to take responsibility and be accountable for all the contents of the article.
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Dimoso PJ, Msaki MM, Suleiman MA. The use of contraceptives among female students in state University of Zanzibar. Religion. 2014;31(40):5.
2. Reis M, Ramiro L, Matos MG, Diniz JA. Nationwide survey of contraceptive and sexually transmitted infection knowledge, attitudes and skills of university students in Portugal. Int J Clin Health Psychol. 2013;13(2):127–137. doi:10.1016/S1697-2600(13)70016-4
3. Hoque M, Ntsipe T, Mokgatle-Nthabu M. Awareness and practices of contraceptive use among university students in Botswana. SAHARA-J. 2013;10(2):83–88. doi:10.1080/17290376.2013.869649
4. Hoque M. Sexual practices among University students in Botswana. Gender Behav. 2012;10(2):4645–4656.
5. Somba MJ, Mbonile M, Obure J, Mahande MJ. Sexual behaviour, contraceptive knowledge and use among female undergraduates’ students of Muhimbili and Dar es Salaam Universities, Tanzania: a cross-sectional study. BMC Womens Health. 2014;14(1):94. doi:10.1186/1472-6874-14-94
6. Wang H, Long L, Cai H, et al. Contraception and unintended pregnancy among unmarried female university students: a cross-sectional study from China. PLoS One. 2015;10(6):e0130212. doi:10.1371/journal.pone.0130212
7. Onebunne CA, Bello FA. Unwanted pregnancy and induced abortion among female undergraduates in University of Ibadan, Nigeria. Trop J Obstet Gynaecol. 2019;36(2):238–242. doi:10.4103/TJOG.TJOG_35_19
8. Gelaye AA, Taye KN, Mekonen T. Magnitude and risk factors of abortion among regular female students in Wolaita Sodo University, Ethiopia. BMC Womens Health. 2014;14(1):50. doi:10.1186/1472-6874-14-50
9. Erena G, Kerbo AA. Unwanted pregnancy and associated factors among female students of Madawalabu University Bale Zone, Oromia Region south east, Ethiopia. Sci J Public Health. 2015;3(1):50–55. doi:10.11648/j.sjph.20150301.19
10. Tilahun D, Assefa T, Belachew T. Predictors of emergency contraceptive use among regular female students at Adama University, Central Ethiopia. Pan Afr Med J. 2010;7(1).
11. Hedayati-Moghaddam MR, Eftekharzadeh-Mashhadi I, Fathimoghadam F, Pourafzali SJ. Sexual and reproductive behaviors among undergraduate university students in Mashhad, a city in Northeast of Iran. J Reprod Infertil. 2015;16(1):43.
12. Abiodun OM, Balogun OR. Sexual activity and contraceptive use among young female students of tertiary educational institutions in Ilorin, Nigeria. Contraception. 2009;79(2):146–149. doi:10.1016/j.contraception.2008.08.002
13. Nalwadda G, Mirembe F, Byamugisha J, Faxelid E. Persistent high fertility in Uganda: young people recount obstacles and enabling factors to use of contraceptives. BMC Public Health. 2010;10(1):530. doi:10.1186/1471-2458-10-530
14. Coetzee MH, Ngunyulu RN. Assessing the use of contraceptives by female undergraduate students in a selected higher educational institution in Gauteng. Curationis. 2015;38(2):1–7. doi:10.4102/curationis.v38i2.1535
15. Nsubuga H, Sekandi JN, Sempeera H, Makumbi FE. Contraceptive use, knowledge, attitude, perceptions and sexual behavior among female University students in Uganda: a cross-sectional survey. BMC Womens Health. 2015;16(1):6. doi:10.1186/s12905-016-0286-6
16. Akintade OL, Pengpid S, Peltzer K. Awareness and use of and barriers to family planning services among female university students in Lesotho. S Afr J Obstet Gynaecol. 2011;17(3):72–78.
17. Munz D, Carson S, Brock B, et al. Contraceptive knowledge and practice among undergraduates at a Canadian university. Am J Obstet Gynecol. 1976;124(5):499–505. doi:10.1016/0002-9378(76)90177-0
18. Ahmed ZD, Sule IB, Abolaji ML, Mohammed Y, Nguku P. Knowledge and utilization of contraceptive devices among unmarried undergraduate students of a tertiary institution in Kano State, Nigeria 2016. Pan Afr Med J. 2017;26. doi:10.11604/pamj.2017.26.103.11436
19. Soressa M, Astatkie A, Berhane Y, Mitiku S. Contraceptive use and associated factors among Dilla University Female Students, Southern Ethiopia. JMCR. 2016;20:11–21.
20. Kara WSK, Benedicto M, Mao J. Knowledge, attitude, and practice of contraception methods among female undergraduates in Dodoma, Tanzania. Cureus. 2019;11(4).
21. Mahamed K, Medhanyie AA, Liben ML, Shamie R. Modern family planning methods utilization and associated Factors among female students in aysaita town, northeastern Ethiopia. Med Res Chronicles. 2017;4:411–419.
22. Lale S, Doris C. Accelerating Universal Access to Reproductive Health. World Health Organization; 2011.
23. Yari F, Moghadam ZB, Parvizi S, Nayeri ND, Rezaei E. Sexual and reproductive health problems of female university students in Iran: a qualitative study. Glob J Health Sci. 2015;7(4):278. doi:10.5539/gjhs.v7n4p278
24. Yared A, Sahile Z, Mekuria M. Sexual and reproductive health experience, knowledge and problems among university students in Ambo, central Ethiopia. Reprod Health. 2017;14(1):41. doi:10.1186/s12978-017-0302-9
25. Yemane B. Contraceptive use and associated factors among Dilla University Female Students, Southern Ethiopia. JMCR. 2016;20:11–21.
26. Ahmed ZD, Sule IB, Abolaji ML, Mohammed Y, Nguku P. Knowledge and utilization of contraceptive devices among unmarried undergraduate students of a tertiary institution in Kano State, Nigeria 2016. Pan Afr Med J. 2017;26.
27. Coetzee MHN. Assessing the use of contraceptives by female undergraduate students in a selected higher educational institution in Gauteng. Curationis. 2015;38(2):1–7.
28. Diane Munz BA. Contraceptive knowledge and practice among undergraduates at a Canadian university. J Obstet Gynaecol. 2016; 124(5):499–505.
29. Akintade OL, Pengpid S, Peltzer K. Awareness and use of and barriers to family planning services among female university students in Lesotho. South Afr J Obstet Gynaecol. 2011; 17(3):72–78.
30. Nsubuga H, Sekandi JN, Sempeera H, Makumbi FE. Contraceptive use, knowledge, attitude, perceptions and sexual behavior among female University students in Uganda: a cross-sectional survey. BMC Womens Health. 2016;16:6.
31. Kara WS, Benedicto M, Mao J. Knowledge, attitude, and practice of contraception methods among female undergraduates in Dodoma, Tanzania. Cureus. 2019;11.
32. Habitu YA, Yeshita HY, Dadi AF, Galcha D. Prevalence of and factors associated with emergency contraceptive use among female undergraduates in Arba Minch University, Southern Ethiopia, 2015: a cross-sectional study. Int J Popul Res. 2018;2018.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
