Back to Journals » Clinical Interventions in Aging » Volume 17
Confusion and Hallucination in a Geriatric Patient. Pitfalls of a Rare Differential: Case Report of an Anti-LGI1-Encephalitis
Authors Meier L, Weinrebe W , Annoni JM, Petersen JA
Received 7 July 2022
Accepted for publication 5 September 2022
Published 26 September 2022 Volume 2022:17 Pages 1423—1432
DOI https://doi.org/10.2147/CIA.S380316
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Luzia Meier,1 Wolfram Weinrebe,2 Jean-Marie Annoni,3 Jens A Petersen4
1Internal Medicine, Bürgerspital Solothurn, Solothurn, Switzerland; 2Internal Medicine, Salemspital Hirslanden Bern, Bern, Switzerland; 3Neurosciences, University of Fribourg, Fribourg, Switzerland; 4Neurology, Neurozentrum Bern, Bern, Switzerland
Correspondence: Wolfram Weinrebe, Department Allgemeine Innere Medizin, Salemspital Bern, Hirslanden Kliniken, Schänzlihalde 33, Bern, 3007, Switzerland, Email [email protected]
Background: Confusion and hallucinations in geriatric patients are frequent symptoms and typically associated with delirium, late-life psychosis or dementia syndromes. A far rarer but well-established differential in patients with rapid cognitive deterioration, acute psychosis, abnormal movements and seizures is autoimmune encephalitis. Exemplified by our case we highlight clinical and economic problems arising in management of geriatric patients with cognitive decline and psychotic symptoms.
Case Presentation: A 77-year-old female caucasian patient with an unremarkable medical history was hospitalized after a fall in association with diarrhea and hyponatremia. Upon adequate therapy, disorientation and troubled short-term memory persisted. Within a week the patient developed visual hallucinations. Basic blood and urine samples and imaging (cranial computed tomography and magnetic resonance imaging) were unremarkable. With progressive cognitive decline, amnestic impairment, word finding difficulty and general apathy, psychiatric and neurologic expertise was introduced. Advanced diagnostics did not resolve a final diagnosis; an electroencephalogram showed unspecific generalized slowing. Extended clinical observation revealed visual hallucinations and faciobrachial dystonic seizures. A treatment with anticonvulsants was initiated. Cerebrospinal fluid ultimately tested positive for voltage-gated potassium channel LGl1 (leucine-rich-inactivated-1) antibodies confirming diagnosis of autoimmune anti-LGI1 encephalitis. Immediate immunotherapy (high-dose glucocorticoids and administration of intravenous immunoglobulin G) led to a rapid improvement of the patient’s condition. After immunotherapy was tapered, the patient had one relapse and completely recovered with reintroduction of glucocorticoids and initiation of therapy with rituximab.
Conclusion: Rapidly progressive dementia in geriatric patients demands a structured and multidisciplinary diagnostic approach. Accurate management and financially supportable care is a major issue in rare diseases such as anti-LGI1-encephalitis. Education and awareness about autoimmune encephalitis of all physicians treating a geriatric population is important in order to involve expertise and establish treatment within reasonable time.
Keywords: neurocognitive decline, visual hallucinations, rapid progressive dementia, autoimmune encephalitis, anti-LGI1-encephalitis, psychogeriatry, case report
Background
Admission of geriatric patients to the emergency department (ED) due to acute deterioration has increased by about 46% within a decade.1 Acute illness or injuries can trigger cognitive impairment. Base-line risk factors (ie malnutrition, dehydration, immobility, comorbidity and polymedication) increase with age and contribute to the higher vulnerability of the geriatric population. Hence, differential diagnosis of confusional states in the elderly is complex and demands a structured approach.2 Typical findings in first assessments are disorientation, inattention or impaired memory ability, perceptive disturbances or arousal fluctuations that are often associated with delirium or dementia syndrome.
Hallucination or delusion represent an important symptomatic overlap of delirium, psychotic disorder, and dementia syndrome. Around 40% of delirious patients are reported to present with psychotic symptoms.3 Primary late-life psychosis is – similar to delirium – is an exclusion diagnosis and approximately 60% of newly onset psychotic symptoms are due to another medical condition.4 In a comprehensive meta-analysis, Stafford et al reported an increasing incidence of psychosis with age (starting from 65 years) and a range of 10–63% in nursing homes. Recent literature shows a significant association of psychotic symptoms with all subtypes of dementia (ie Alzheimer’s dementia, Lewy body, vascular, etc.), though typically reported in the context of Lewy body disease.5 Symptoms of rapid cognitive decline and psychosis can be a relative emergency; some causative diseases are treatable and at least partially reversible, whereby autoimmune-mediated pathologies such as autoimmune encephalitis (AE) shift into focus.6
Autoimmune Encephalitis
The estimated prevalence of AE is 13 per 100,000.7 The recent observation of an increasing incidence correlates with improving knowledge of disease and commercially available laboratory analytics, leading to more frequent case reporting. AE was initially recognized as a paraneoplastic neurologic disease (PND) with antibody-mediated autoimmune inflammatory response of the central nervous system.8 Over time, different clinical syndromes have been diagnosed with AE and up to 30 different associated antibodies have been identified, not all of them present with underlying malignancy.9 In general, two subgroups of antibodies have been distinguished: 1) Antibodies against intracellular antigens and 2) antibodies targeting cell-surface antigens, such as synaptic receptors or ion channels. Antibodies of the first subgroup tend to be cancer-related and are referred to as “onconeural antibodies”. Onconeuronal antibodies cause a T-cell mediated immune response while antibodies against synaptic receptors or cell-surface proteins are often directly pathogenic.9 The etiology of antibodies targeting surface or synaptic antigens remains idiopathic in most cases, some are thought to be triggered by viral infection or immune-modulating therapies (such as immune-checkpoint inhibitors).8,9
The most frequent antibody in this second subgroup is anti-N-methyl-D-aspartate-receptor (anti-NMDA-r) that is associated with the commonly known disease anti-NMDA-r encephalitis. With an estimated incidence of 1.5 per million population per year it is still considered rare.10 Frequent symptoms are psychosis, insomnia, reduced verbal output and seizures.10 Typically affected are young female patients and in 40–60% of those cases it is associated with ovarian theratoma.9 The disease and underlying pathophysiology was described in 2007 and thereafter the knowledge about autoimmune encephalitis and its various subtypes has grown rapidly.10 The ongoing identification of associated antibodies has been helpful in differentiating subtypes and delineating clinical syndromes.
The detection of antibodies targeting the cell-surface protein leucine-rich-glioma 1 (anti-LGI1) is an example of this progress. Prior to detection of anti-LGI1, antibodies targeting the ion channel voltage-gated potassium channel (VGKC) had been described, mostly in elderly males, and the clinical presentation of VGKC-positive patients varied widely. About a decade ago, it was detected that the targeted antigen is not the VGKC itself but rather its associated proteins: leucine-rich glioma 1 (LGI1) and contactin associated protein 2 (CASPR-2). The differentiation helped in distinguishing clinical features: Anti-CASPR-2 mediated disease is associated with central or peripheral nervous system symptoms (ie hyperexcitability or Morvan’s syndrome consisting of neuromyotonia, dysautonomia and sleep disturbances) while anti-LG1-encephalitis presents with limbic encephalitis (LE).11
Overall, AE comprises heterogenous subtypes that vary significantly in etiology, inflammatory-affected anatomical structures and clinical presentation (incl. demographic and sex characteristics).
Frequent symptoms observed in many AE are short-term memory disturbances, confusion, seizures or psychiatric symptoms (the latter indicate involvement of the limbic system).6,12,13
Diagnostic findings may include abnormalities in cerebral magnetic resonance imaging (cMRI), electroencephalogram (EEG) and analysis of cerebrospinal fluid (CSF).
Lumbar puncture (LP) and analysis of CSF should assess cell count, protein, and glucose as well as cytology to exclude leptomeningeal metastasis and exclusion of infectious etiologies. CSF without any pathologic findings (ie pleocytosis, elevated protein concentration, oligoclonal bands) is reported in up to 46% of patients.14
Detection of specific autoantibodies confirms a diagnosis. It is recommended to test both CSF and blood serum initially for antibodies.12 Turnaround times of analytic panels often take days to weeks. Dependence on these laboratory results is not practicable in clinical settings and three diagnostic criteria for AE without relying on antibody-confirmation have been proposed by Graus et. al: 1) A subacute onset (rapid progression of less than 3 months) of working memory deficits (short-term memory loss), altered mental status or presence of psychiatric symptoms. 2) One or more of the following clinical, laboratory or imaginary findings: New focal CNS findings, seizures not attributable to a preexisting seizure disorder, CSF pleocytosis CSF (white blood cell (WBC) count ≥ 5/cubic mm) or MRI-features suggestive of encephalitis. 3) Reasonable exclusion of alternative causes.12 In some patients who meet the criteria and are highly suspected of having AE, CSF and serum can test negative, which reflects the high probability of yet undescribed antibodies.8
Treatment of AE involves immunotherapy with first line administration of intravenous/oral corticosteroids, followed by intravenous immunoglobulin (IVIG) and/or plasma exchange (PLEX). Rituximab and cyclophosphamide are considered second line treatments. Therapy recommendations based on expert consensus and smaller retrospective studies; randomized controlled trials have not been conducted.8,15
In the context of our case we address differential diagnosis, clinical and diagnostic findings, and therapy response of anti-LGI1 encephalitis. We emphasize difficulties for clinicians in managing and treating complex geriatric patients while trying to provide a cost-covering treatment.
Case Report
Demographics and Past Medical History
We report the case of a 77-year-old female patient living at home on their own and independent in all instrumental activities of daily living (IADL). Her personal history was unremarkable apart from frequent bronchiolitis. She reported penicillin and mite allergy, no regular intake of medication and no substance abuses.
Hospital Admission
The patient was admitted to our primary-care facility ED in July 2020 after a fall with head impact. She complained of subtle deterioration in the preceding 1–2 weeks and reported mild nausea, diarrhea and sleeping disturbances and low nutritional and fluid intake. Upon arrival she had normal vital parameters, a Glasgow coma scale (GCS) of 15 points and no fever. The detailed clinical examination is listed in Table 1. Predominant findings were dsorientation, general psychomotor slowing, gait insecurity and signs of exsiccosis.
 |
Table 1 Clinical Examination at First Admission (July 2020) |
Blood analysis revealed a hyponatremia of 110 mmol/l and hypopotassemia of 3.2 mmol/l. Blood pH, hemoglobin, c-reactive protein (CRP), leucocytes, creatinine and urea were within normal ranges. Uric acid (132 μmol/L) and serum osmolality were low (237 mOsm/kg). Urine analyses showed a leukocyturia and bacteriuria (asymptomatic), within-range osmolality (273 mOsm/kg) and sodium excretion of 35 mmol/L. Through cranial computed tomography (cCT) cerebral lesions or bleedings were excluded. Based on the clinical examination and history, she was diagnosed with a hypovolemic hypoosmolar chronic hyponatremia (>48 h) with suspected extra-renal loss due to persisting diarrhea. The fall was attributed to gait insecurity associated with hyponatremia. Therapy with saline supplementation 0.9% NaCl was initiated, and rapid overcorrection prevented by controlling sodium levels regularly. As Figure 1 shows, hyponatremia improved but persisted mildly after volume correction. Repeated blood and urine analyses were consistent with criteria for syndrome of inappropriate antidiuretic hormone secretion (SIADH) (euvolemia, urine osmolality 493 mOsm/kg, sodium excretion 94 mmol/L, fractional excretion of uric acid 13%). The treatment was adapted to fluid restriction 1000 mL per day. Despite nearly normalized sodium levels, the patient’s symptoms improved marginally. She developed visual hallucinations and described a detailed view of colored butterflies, which were bothering her but not provoking anxiety, aggression or mistrust. A cerebral magnetic resonance imaging (cMRI) did not reveal any pathologic findings. Extended blood analyses were normal except for vitamin D deficiency (testing for folic acid, TSH and fT3, fT4, ferritin, vitamin B12, liver enzymes). A third-party anamnesis with a neighbor revealed no behavioral changes prior to the hospitalization.
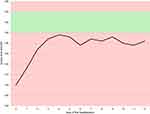 |
Figure 1 Sodium levels at first hospitalization. |
Within a week the patient’s condition stabilized, though she remained partially disoriented phase-wise and distractible in conversations. The hallucinations disappeared without specific therapy. Psychiatric and neurologic expertise was involved and the working diagnosis of a prolonged delirium (triggered by recent illness and the hospitalization) was established. A transfer to a psychiatric ward was discussed, the patient urged for a discharge since feeling better. Her condition was stable and not endangering herself or others; hence institutionalization was not indicated. Considering the frequent improvement of long-term deliriant patients when returning to their familiar environment, she was dismissed. Daily medical support was guaranteed through home visits of specialized nursing staff. Her condition did not improve, an unobserved second fall was reported after a few days and led to readmission. She presented with aggravated symptoms of disorientation, loss of concentration, reduced short-term memory and inability to follow a conversation. She scored 17 points out of 30 in the Montreal Cognitive Assessment (MoCA) (see Appendix Figure 1). A detailed neurologic exam revealed neuropsychologic deficits and psychomotor slowing (see Appendix Table 1). Another third-party anamnesis (with a long-term friend), revealed some disorientation prior to the first hospitalization with general slowing and forgetfulness while doing groceries.
Basic laboratory analysis showed persisting mild hyponatremia while being otherwise unsuspicious. Repeated cCT and cMRI with contrast media were assessed by a radiologist and a neurologist who reported unspecific findings (cortical atrophia and a singular microbleeding in the left frontal lobe) that did not correlate with the clinical condition.
LP was performed in search of an infectious or autoimmune disease, basic analysis of CSF showed normal range of protein (albumin), cell-count, glucose levels, IgG and IgM. Screening of biomarkers for infectious or rheumatic diseases was unremarkable. Parameters indicating endocrinologic pathologies such as autoimmune thyroiditis or adrenal insufficiency were normal (see Appendix Table 2 for a summary of laboratory analyses).
Cerebrospinal fluid (CSF) samples were sent to an external laboratory to test for specific neuropathologic biochemical parameters (dementia and Creutzfeld-Jacob disease biomarkers, panel of autoimmune encephalitis antibodies).
Considering a paraneoplastic phenomenon, a screening for underlying malignancy was performed (thoraco-abdominal CT-scan, gynecologic examination and vaginal ultrasound) but did not reveal any tumor-suspicious lesions. The patient`s condition deteriorated; she presented fluctuating vigilance and drowsiness with stupor-like phases. A second episode of hallucinations occurred: The patient described falling objects she tried to catch and saw machines driving towards her, resulting in massive discomfort. Within a few days conversations were no longer possible and she only answered simple, close-ended questions. Simultaneously, seizures were observed: Awareness remained unchanged while brief episodes of face tightening and grimacing with right arm flexing and sometimes right hand tightening and right leg flexion occurred. The episodes lasted around 30 seconds and happened 3–4 times per day and were consistent with faciobrachial dystonic seizures (FBDS). An electroencephalogram (EEG) showed generalized intermittent mild to moderate background slowing in the theta-/delta-range. This unspecific pathologic pattern remained unchanged with no signs of ictal morphology during the FBDS. A treatment with anticonvulsants (levetiracetam) was initiated and reduced the frequency of FBDS to once or twice per day.
Diagnosis of limbic AE was confirmed with a positive titer (1:3.2) of LGI1-antibodies in the CSF. A serum analysis was not performed. Immediate immunotherapy with intravenous application of methyl prednisone 1000 mg/day for five days followed by intravenous immunoglobulin G (IVIG) 60 g/day for three days (privigen). Within the first days of corticosteroid-therapy, the patient’s condition improved remarkably. She still had some mnestic deficits, sluggishness and fatigability. Glucocorticosteroids were orally tapered and a detailed neuropsychological examination 9 weeks after treatment initiation revealed normal neurocognitive findings indicating a dramatic improvement. After completing a month of neurorehabilitation the patient returned to her home with nursing support once per day. A slow reduction and cessation of glucocortico-steroids was planned until 4 months after initiation.
Follow Up
In the further course, the patient suffered vertebral body compression fractures (L1-L4) due to advanced osteoporosis. Percutaneous vertebroplasty was necessary 6 months after initiation of corticosteroid-therapy in July 2020 (which was stopped a month prior to the operation). Two weeks later, the patient was readmitted to our primary care facility for cognitive deterioration. A relapse of AE was suspected and confirmed with detection of anti-LGI1 antibodies in blood serum. Repetition of LP for CSF analysis was contraindicated due to recent vertebroplasty. After receiving a second high-dose i.v. corticosteroid-therapy and clinical improvement, she was dismissed with oral corticosteroids. A week later (December 2020), re-hospitalization occurred due to general impairment; Bilateral Sars-Cov2-pneumonia and right superior pulmonary embolism were diagnosed. After treatment and successful recovery of pneumonia and embolism, a steroid-sparing therapy with rituximab was favored and planned in an ambulatory setting. Three months after the relapse, the first cycle of rituximab (1000 mg i.v.) was successfully administered and followed by a second cycle. In March 2021 she was independent in almost all IADL (she had nursing support for daily medication) and able to live in her apartment again.
Discussion
Remarks on Differential Diagnosis of Rapidly Progressive Cognitive Impairment
In assessing cognitive changes or hallucination in geriatric patients, consideration and research of underlying, attributing or causative disorders and factors are essential. The evaluation of possible differentials is typically guided by incidence of diseases (comp. general overview Figure 2 in the Appendix). Encephalopathy, dementia, delirium and cognitive impairment can present with similar clinical symptoms, but underlying pathophysiology and treatment differ significantly.9 Difficulties in differentiation is reflected by up to a third of geriatric patients with immune-mediated etiologies of cognitive impairment that were initially diagnosed with an irreversible neurodegenerative dementia or prion disorder.6
Clinical presentation and basic diagnostics may be unspecific. For example, geriatric patients with AE often present unremarkable cMRI findings and basic analysis of CSF.16,17
Mismanagement of specific symptoms in geriatric patients can lead to transfer to nursing homes or psychiatric wards and potentially delay diagnosis.6 In AE, diagnosis is reported to be established within 5–6 months after first presentation but delays of up to two years have occurred.15,18 Extended diagnostics are more likely to be initiated later as in the younger population, since delusional or cognitive symptoms are less contrasted and occur with a higher frequency in the elderly.6
Autoimmune Encephalitis
In confirmed or highly suspected AE regardless of subtype (and after infection being ruled out as an alternative cause of encephalitis) a prompt initiation of immunotherapy with high dose corticosteroids is strongly recommended.12 Hesitative administration of immunotherapy might still be an issue without confirmation of a corresponding antibody in serum or CSF (although proposed diagnostic criteria do not rely on these results).12 Patients with seronegative autoimmune encephalitis (who exhibit typical symptoms but laboratory analysis does not confirm associated antibodies) need to be treated equally.12 AE associated with synaptic receptor or surface-protein targeting-antibodies tend to respond better to immunotherapy than AE arising from PND associated with the onconeural antibodies, which improve only with cancer-treatment. Accountable are the different underlying pathophysiologic mechanisms (direct pathogeny of antibodies versus humoral and cell-mediated immune response). Despite the different response, first-line empiric treatment recommendations for all AE include intravenous methylprednisolone 1 g/day for 3−7 days.8 Relative contraindications to steroids are frequent amongst geriatric patients: Uncontrolled hypertension, uncontrolled diabetes mellitus, acute peptic ulceration.13 A general tumor screening though is advisable as underlying malignancy is possible in all subtypes of AE. The higher prevalence of neoplastic disease in certain clinical syndromes or associated antibodies (for example, small-cell lung carcinoma (SCLC) with anti-neuronal nuclear antibodies) or specific patient groups guide further diagnostics. If any neoplasia is identified, early involvement of oncologists and cancer-specific therapy must parallel immunomodulatory AE therapy.8,12 A diagnostic pathway in AE assessment is proposed in Figure 2.
 |
In the case of an unsuccessful initial treatment cycle with methyl prednisone, administration of IVIG or therapeutic plasma exchange (PLEX) is recommended. PLEX is preferred in severe hyponatremia, high thromboembolic risk, and if associated brain or spinal demyelination are present.8,14 After 2–4 weeks a therapy evaluation is recommended; If there is no improvement (clinically, radiologically or serologically), a second line agent (ie rituximab) in idiopathic AE or cyclophosphamide in PND should be considered.8 The overall good prognosis of non-paraneoplastic AE is confirmed by compelling data which show that immunotherapy led to clinical improvement in 80% of patients who achieved a good outcome.14 In PND, outcome varies and depends on the subtype as well as on progression and treatability of underlying malignancy.9
Anti-LGI-1-Encephalitis
In retrospect, the overall symptoms of our patient classify as a typical presentation of anti-LGI1 encephalitis (comp. Figure 3).
 |
Figure 3 Illustration of the patient`s clinical course until established diagnosis of anti-LGI1-encephalitis. |
However, some deviations had a significant impact on differential diagnosis. The mean onset age is around 60 years with a 2:1 male predominance. Patients with anti-LG1-encephalitis typically present rapidly progressive dementia with memory impairment and altered behavior. Intractable hyponatremia is frequent (60%) and the resulting SIADH as LGI1 antibodies are assumed to interfere with ADH-producing neurons in the hypothalamic region. In our case, the initial diagnosis of hypovolemic hyponatremia can be critically discussed as it was predominantly based on clinical findings and anamnestic cues, but is partially supported by improvement of sodium values after isotonic saline administration. After volume-correction, criteria for SIADH were present and overall, a mixed etiology is very likely.19 The hyponatremia in anti-LGI1-encephalitis does not or only minimally responds to fluid restriction or saline supplementation, but improves with immunotherapy as it did in our patient.13
Psychiatric symptoms (ie hallucinations, mood disturbances) are unspecific for all types of limbic encephalitis but reported in association with cognitive impairment, though research on frequency is lacking.13
Pathognomonic for anti-LGI1 encephalitis (but only reported in about 50% of cases) are FBDS. They consist of brief, unilateral contractions of the arm, may involve the ipsilateral face or leg and occur up to 100 times per day.20 FBDS rarely present with correlating ictal morphology in EEG.21,22 Contrary as in our patient, they typically precede the onset of cognitive decline and often represent the first symptom of disease.14,20 Cerebral MRI shows T2 signal alterations in medial temporal lobe in two-thirds of the patients,11,20 and 38% of patients with FBDS show basal ganglia abnormalities.22 Tumors are present in 0–11% of patients with thymoma and small-cell lung cancer being the most common types.11,12,20 The relapse rate in anti-LGI1 encephalitis in retrospectively analyzed patient groups ranges from 16% to 35%, occurring within 5 months up to 2 years.15,17,23
Overall, our patient marks an example for the described difficulties in differential diagnostics in the elderly and in AE: Initial symptoms were attributed to more probable differentials such as delirium or neurodegenerative dementia syndrome. Demographic atypia, repetitively unremarkable cMRI-scans and normal basic CSF-analysis as well as late onset of FBDS may have delayed immunotherapy to a certain extent. Since autoimmune encephalitis antibodies may be found either in CSF or serum, both should be analyzed. Therapy was initiated around 7 weeks after symptom-onset with confirmed antibodies, respectively 4.9 weeks after first admission. Though a prompt immunotherapy is indicated, a thorough evaluation and close follow up is necessary especially in the elderly, as complications from chronic immunosuppressive therapy might arise more frequently and severely.
Financial Aspects and Medical Coding
Clinicians must provide cost-efficient ancillary testing and prevent over diagnosing and unnecessary examinations, hence initiation of the adequate work-up is an act of balance. In Switzerland, some difficulties in providing a cost-covering treatment is rooted in the billing system for clinical care. Remuneration of inpatient hospital services is regulated through the Swiss diagnosis related groups (SwissDRG), a rating system wherein diagnoses and assigned lengths of hospital stay represent the core areas of payment.24 Specifications arise from comparison of different clinical care settings; rare conditions have a low impact and are not (yet) well represented in this system. Cost-intensive rare diseases (diagnostics and therapy) are mostly not covered by the SwissDRG.
Overall the hospital care of our case required 75 days. In AE patients, increased charges have been described due to the long duration of hospitalization, which is - apart from the complexity of the disease itself - assumed to be a partial result of suboptimal diagnostic and therapeutic modalities.25
Whether earlier recognition and treatment of our patient would have alleviated the outcome or minimized complication rate and costs is debatable, as therapy was initiated around 7 weeks after first onset of symptoms. Van Sonderen et al state in a retrospective analysis of 38 included cases with anti-LGI1 encephalitis a median treatment delay of 22 weeks. A two-year follow up of 21 patients showed no relation of treatment delay with final outcome or time to maximum recovery in 67% of patients with a favorable outcome, which is comparable to our case so far. They reported two patients who died due to comorbidities associated and aggravated with corticosteroid-therapy (ie spinal cord injury due to thoracic fracture).15
The overall financial loss in our case amounts to approximately 36,000 CHF and would have possibly been considerably higher without specific in-hospital economic optimization.
Conclusion
In view of a growing geriatric population, the health system will face severe challenges in order to provide accurate as well as financially supportable care. Confusional states and psychotic symptoms in the elderly are frequent and need to be addressed carefully. Polymorbidity and symptomatic overlap add to the complexity in differential diagnosis, especially concerning rare cases such as our patient with anti-LG1-encephalitis presenting as rapidly progressive dementia. Education about AE and suggestive symptoms (ie FBDS) in primary caregivers, psychiatrists and clinicians of geriatric wards are essential in order to select patients that need further evaluation and to prevent or minimize hazardous delays in immunotherapy.
Data Sharing Statement
The patient’s data was acquired from the electronic database of the Hirslanden Campus Bern and Neurozentrum Bern, including demographic information, laboratory results, radiological and neurological examinations and treatment details. The patient was participating in a geriatric rehabilitation program, resulting in repeated detailed multidisciplinary assessment of the patient’s condition involving medical, physiotherapeutic, occupational and nutritional advisory expertise.
Statement of Ethics
The patient gave her written informed consent to use her anonymized data, case history and graphics for a case report. Institutional approval was not required to publish the case.
Author Contributions
LM obtained clinical findings, reviewed the literature, prepared the tables and figures, obtained written informed consent and drafted the manuscript. WW obtained clinical findings, performed the financial calculation, wrote the corresponding section and reviewed and revised the manuscript. JP obtained clinical findings, reviewed and revised the manuscript. JMA reviewed and revised the manuscript, the figures and tables. All Authors read and approved the final manuscript including the tables and figures. They all agreed on the submission to the journal “Clinical Interventions in Aging” and take responsibility for the contents of the article.
Funding
No funding was received.
Disclosure
The authors declare that they have no competing interests.
References
1. Ukkonen M, Jämsen E, Zeitlin R, Pauniaho SL. Emergency department visits in older patients: a population-based survey. BMC Emerg Med. 2019;19(1):20. doi:10.1186/s12873-019-0236-3
2. Grossman M, Irwin DJ. The mental status examination in patients with suspected dementia. Contin Minneap Minn. 2016;22(2Dementia):385–403.
3. Paik SH, Ahn JS, Min S, Park KC, Kim MH, Guloksuz S. Impact of psychotic symptoms on clinical outcomes in delirium. PLoS One. 2018;13(7):e0200538. doi:10.1371/journal.pone.0200538
4. Khouzam HR, Emes R. Late life psychosis: assessment and general treatment strategies. Compr Ther. 2007;33(3):127–143. doi:10.1007/s12019-007-0016-y
5. Liew TM. Neuropsychiatric symptoms in cognitively normal older persons, and the association with Alzheimer’s and non-Alzheimer’s dementia. Alzheimers Res Ther. 2020;31(12):35. doi:10.1186/s13195-020-00604-7
6. Banks SA, Sechi E, Flanagan EP. Autoimmune encephalopathies presenting as dementia of subacute onset and rapid progression. Ther Adv Neurol Disord. 2021;14:175628642199890. doi:10.1177/1756286421998906
7. Dubey D, Pittock SJ, Kelly CR, et al. Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann Neurol. 2018;83(1):166–177. doi:10.1002/ana.25131
8. Abboud H, Probasco JC, Irani S, et al. Autoimmune encephalitis: proposed best practice recommendations for diagnosis and acute management. J Neurol Neurosurg Psychiatry. 2021;92(7):757–768. doi:10.1136/jnnp-2020-325300
9. Bradshaw MJ, Linnoila JJ. An Overview of Autoimmune and Paraneoplastic Encephalitides. Semin Neurol. 2018;38(3):330–343. doi:10.1055/s-0038-1660821
10. Dalmau J, Armangué T, Planagumà J, et al. An update on anti-NMDA receptor encephalitis for neurologists and psychiatrists: mechanisms and models. Lancet Neurol. 2019;18(11):1045–1057. doi:10.1016/S1474-4422(19)30244-3
11. van Sonderen A, Schreurs MWJ, Wirtz PW, Sillevis Smitt PAE, Titulaer MJ. From VGKC to LGI1 and Caspr2 encephalitis: the evolution of a disease entity over time. Autoimmun Rev. 2016;15(10):970–974. doi:10.1016/j.autrev.2016.07.018
12. Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391–404. doi:10.1016/S1474-4422(15)00401-9
13. Thompson J, Bi M, Murchison AG, et al. The importance of early immunotherapy in patients with faciobrachial dystonic seizures. Brain. 2018;141(2):348–356. doi:10.1093/brain/awx323
14. Hayden Z, Bóné B, Orsi G, et al. Clinical characteristics and outcome of neuronal surface antibody-mediated autoimmune encephalitis patients in a national cohort. Front Neurol. 2021;12:611597. doi:10.3389/fneur.2021.611597
15. van Sonderen A, Thijs RD, Coenders EC, et al. Anti-LGI1 encephalitis: clinical syndrome and long-term follow-up. Neurology. 2016;87(14):1449–1456. doi:10.1212/WNL.0000000000003173
16. Escudero D, Guasp M, Ariño H, et al. Antibody-associated CNS syndromes without signs of inflammation in the elderly. Neurology. 2017;89(14):1471–1475. doi:10.1212/WNL.0000000000004541
17. Ariño H, Armangué T, Petit-Pedrol M, et al. Anti-LGI1–associated cognitive impairment. Neurology. 2016;87(8):759–765. doi:10.1212/WNL.0000000000003009
18. Wang M, Cao X, Liu Q, Ma W, Guo X, Liu X. Clinical features of limbic encephalitis with LGI1 antibody. Neuropsychiatr Dis Treat. 2017;13:1589–1596. doi:10.2147/NDT.S136723
19. Hoorn EJ, Zietse R. Diagnosis and treatment of hyponatremia: compilation of the guidelines. J Am Soc Nephrol. 2017;28(5):1340–1349. doi:10.1681/ASN.2016101139
20. Irani SR, Michell AW, Lang B, et al. Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann Neurol. 2011;69(5):892–900. doi:10.1002/ana.22307
21. Simabukuro MM, Nóbrega PR, Pitombeira M, et al. The importance of recognizing faciobrachial dystonic seizures in rapidly progressive dementias. Dement Neuropsychol. 2016;10(4):351–357. doi:10.1590/s1980-5764-2016dn1004016
22. Flanagan EP, Kotsenas AL, Britton JW, et al. Basal ganglia T1 hyperintensity in LGI1-autoantibody faciobrachial dystonic seizures. Neurol Neuroimmunol Neuroinflam. 2015;2(6):e161. doi:10.1212/NXI.0000000000000161
23. Qiao S, Wu HK, Liu LL, et al. Clinical features and long-term outcomes of anti-leucine-rich glioma-inactivated 1 encephalitis: a multi-center study. Neuropsychiatr Dis Treat. 2021;17:203–212. doi:10.2147/NDT.S292343
24. Swiss DR. Regeln und Definitionen zur Fallabrechnung unter SwissDRG und TARPSY; 2019.
25. Cohen J, Sotoca J, Gandhi S, et al. Autoimmune encephalitis: a costly condition. Neurology. 2019;92(9):e964–e972. doi:10.1212/WNL.0000000000006990
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
