Back to Journals » Risk Management and Healthcare Policy » Volume 14
Compliance with COVID-19 Preventive Measures and Associated Factors Among Women Attending Antenatal Care at Public Health Facilities of Debre Berhan Town, Ethiopia
Authors Silesh M , Demisse TL , Taye BT , Desta K, Kitaw TM, Mekuria AD , Tafesse TT, Fenta B
Received 24 July 2021
Accepted for publication 28 October 2021
Published 10 November 2021 Volume 2021:14 Pages 4561—4569
DOI https://doi.org/10.2147/RMHP.S330932
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jongwha Chang
Mulualem Silesh,1 Tesfanesh Lemma Demisse,1 Birhan Tsegaw Taye,1 Kelem Desta,1 Tebabere Moltot Kitaw,1 Abinet Dagnaw Mekuria,2 Tiwabwork Tekalign Tafesse,3 Belete Fenta4
1Department of Midwifery, College of Health Science, Debre Berhan University, Debre Berhan, Ethiopia; 2Department of Public Health, College of Health Science, Debre Berhan University, Debre Berhan, Ethiopia; 3School of Nursing, College of Health Science, Wolaita Sodo University, Wolaita Sodo, Ethiopia; 4School of Midwifery, Faculty of Health Science, Jimma University, Jimma, Ethiopia
Correspondence: Mulualem Silesh Email [email protected]
Background: Coronavirus disease-2019 (COVID-19) is a highly contagious and cause for the death of many people worldwide. Due to physiological immunosuppressive state and mechanical alteration, pregnant women are at a higher risk of severe illness and adverse maternal and fetal outcomes from COVID-19 than non-pregnant women. Compliance with the preventive measures is essential to control COVID-19 related consequences. Therefore, this study aimed to assess compliance with COVID-19 preventive measures among pregnant women attending antenatal care at public facilities of Debre Berhan town, Ethiopia.
Methods: A facility-based cross-sectional study was conducted from May 1 to 30, 2021 among 402 pregnant mothers. Data were collected via a face-to-face interviewer-administered questionnaire. Then, entered into Epi-Data version 4.6 and exported to SPSS version 25 for data analysis. In multivariable logistic regression analysis, variables with p < 0.05 were declared as statistically significant and the strength of statistical association was measured by adjusted odds ratio (AOR) and 95% confidence interval (CI).
Results: Of the total 396 participants, 222 (56.1%) of women had a good compliance with COVID-19 preventive measures. Maternal age (25– 34 years) [AOR: 1.926; 95% CI (1.084, 3.421)] and (≥ 35 years) [AOR: 3.018; 95% CI (1.53, 5.952)], husband educational status [AOR: 3.68; 95% CI (1.55, 8.737)], had current chronic disease [AOR: 2.516; 95% CI (1.297, 4.883)], and knowledge [AOR: 5.484; 95% CI (3.057, 9.838)] were significant predictors to have good compliance with COVID-19 preventive measures.
Conclusion: Although COVID-19 is a global and national agenda, compliance towards its preventive measures was not sufficient enough. Therefore, scale-up the community awareness via media campaign is crucial which will eventually improve compliance. Furthermore, those women who had no pre-existing chronic diseases and those in the young age group should be given special consideration.
Keywords: antenatal care, compliance, COVID-19, Ethiopia
Introduction
Coronavirus disease-2019 (COVID-19) is a pandemic disease and a major global health concern1 one which was first reported from Wuhan, in China in December 2019.2 This newly emerged disease novel coronavirus primarily affects the respiratory system.3 Globally, as of July 16, 2021, there have been 188,655,968 confirmed cases of COVID-19, including 4,067,517 deaths reported to world health organization (WHO).4
COVID-19 is highly contagious and causes the death of many peoples in the world. As of July 15, 2021, a total of 3,402,275,866 vaccine doses have been administered reported to WHO.4 As WHO recommendation, the necessary preventive measures for COVID-19 are hand washing daily with soap and water, hand rubbing with sanitizers, using a face mask, covering the mouth with hand during coughing, keeping social distance, and stopping to touch the eyes, nose, and mouth.5,6
The majority of the deaths reported worldwide are among the elderly or those with co-morbidities and poor immunity.7 So, several pregnancy-related complications from physiological immune responses and mechanical alteration during pregnancy and potential risks from the cytokine-storm by COVID-19 infection causes pregnant women more susceptible to respiratory pathogens that may place them to face severe morbidity and even mortality related to COVID-19.8–10
COVID-19 infection does not appear to be more common in pregnant women.4 However, compared to non-pregnant women, pregnant women are at a higher risk of severe illness and adverse maternal obstetrical complications from COVID-19.11–13 A more recent study found that advanced maternal age, a high body mass index (BMI), and pre-existing comorbidities were all risk factors for severe COVID-19 during pregnancy.4,14 Pregnant women are a high-risk group for COVID-19 infection, and the virus’s potential negative consequences on maternal and perinatal outcomes are a major global concern.14 Particularly, COVID-19 puts pregnant women and newborns at risk in LMICs.15
During the COVID-19 pandemic, adverse maternal and fetal outcomes, including as preeclampsia, fetal distress, miscarriage, respiratory distress, stillbirth, preterm birth, and NICU hospitalization, increased globally16–18 which resulted from hypo-perfusion and reduced oxygen delivery from the placenta to the fetus.19 The systematic reviews suggest that maternal COVID-19 infection in the third trimester appears to be associated with a 3.2–3.9% % rate of vertical transmission.20,21
Although, studies revealed that strong social support during pregnancy has a positive impact to improving maternal quality of life (QOL) and preventing the adverse pregnancy outcomes,22 COVID-19 related fear has a negatively effects QOL.23 Due to COVID-19 preventive measures recommendation, the likelihood of developing anxiety and depressive symptoms are increased among pregnant women who are mainly due to poor social support even within family members.24
Although the Ethiopian government is highly dedicated to controlling the outbreak after the first case of COVID-19 on March 13, 2020,25 the incidence of the virus is continuously accelerating every day. As of July 16, 2021, there were a total of 277,443 cases, of which 4350 deaths were reported and as of July 13,2021, 2,062,456 vaccines have been administered.4 For successful control of the pandemic and COVID-19 related negative impact like adverse maternal and fetal outcomes, particularly in developing country including Ethiopia, people’s adherence to COVID-19 preventive measures is essential.27 In Ethiopia, studies on the compliance with COVID-19 preventive measures compliance are mostly focused on health-care practitioners and the general public, with compliance rates ranging from 12.3% to 44.1%.26–28 But, there has not been any research done on this issue yet among pregnant women.
Therefore, this study aimed to assess compliance with COVID-19 preventive measures and associated factors among pregnant women attending antenatal care at public health facilities of Debre Berhan town, Ethiopia. The findings of this study will be used by local policymakers and healthcare professionals to establish effective actions to combat the pandemic effect and to give special considerations in this vulnerable group. Furthermore, it will used as an input for researchers for further investigations.
Methods and Materials
Study Design, Setting and Period
A facility-based cross-sectional study was conducted at public health facilities of Debre Berhan town, North Shoa Zone, Ethiopia from May 1–30, 2021. Debre Berhan is found in North Shoa Zone Amhara regional state 130 km from the capital city of Ethiopia, Addis Ababa. The town has one public referral hospital and three health centers; of which one health center is currently used for COVID-19 patients’ quarantine and treatment center. Therefore, the study was conducted at three public health facilities of Debre Berhan town.
Study Population and Eligibility Criteria
All pregnant women who had antenatal care (ANC) follow-up for the current pregnancy at public health facilities of Debre Berhan town during the study period were the study population. Women who attend ANC follow-up at public health facilities and agree to participate in the study were included, while pregnant women who were critically ill were excluded from the study.
Sample Size Determination and Sampling Technique
The sample size was determined using single population proportion formula  with the following assumptions: the proportion of pregnant women who have good level Knowledge 52.1% (p= 0.521) taken from a study conducted in Debre Tabor,29 with a 95% confidence interval (1.96), and margin of error of 5%. After adding a 5% non-response rate, the final sample size was 402.
with the following assumptions: the proportion of pregnant women who have good level Knowledge 52.1% (p= 0.521) taken from a study conducted in Debre Tabor,29 with a 95% confidence interval (1.96), and margin of error of 5%. After adding a 5% non-response rate, the final sample size was 402.
The study was conducted at three public health facilities (Debre Berhan Comprehensive specialized hospital, Debre Berhan 04 health center, and Ayer tena health center. The calculated sample size was proportionally allocated to each public health facility based on the average number of ANC follow-ups per month. The study subjects were selected by using a systematic random sampling technique from each public health facility. The kth interval was computed which was 2.37 ̴ 2. Therefore, every two pregnant women who were attending ANC follow-ups were included in the study until the required/allocated respondents were obtained in each health facility. The first woman was selected randomly using the lottery method.
Data Collection Instrument and Procedures
Data were collected using a pre-tested structured interviewer-administered questionnaire after taking informed written consent from the study participants. The structured questionnaire was translated into local languages (Amharic) then back to English by another person to maintain consistency. The questionnaire comprises five parts; socio-demographic characteristics, reproductive and maternal health service-related characteristics, knowledge assessment, attitude towards COVID-19 preventive measures, and compliance with COVID-19 Preventive measures. The questionnaire was adapted after reviewing different related literature.29–32 Three diploma midwives and one BSc holder midwife were involved as data collectors and supervisor, respectively. Both data collectors and supervisor were trained for one day before the actual data collection period.
Operational Definitions
Knowledge: Was measured using 10-item questions and participants were asked to answer using “yes” and “no”. A value of 1 for correct and 0 for incorrect responses was given and the total score range from 0 to 10. Those women who scored 60% and above were considered as having good knowledge and who scored less than 60% were considered as having poor knowledge.33,34
Attitude towards COVID-19 preventive measures: Was measured using eight attitude-related questions. Participants were asked to answer using a 5-point Likert scale of 1–strongly disagree to 5-strongly agree, with the total score ranges from 8 to 40. Those women who scored 60% and above were considered as having a positive attitude towards COVID-19 preventive measures and who scored less than 60% were considered as having a negative attitude.34
Compliance with COVID-19 preventive measures: Was measured by using ten questions and participants were asked to rate their practice of COVID-19 preventive measures for the last 7 days using a 3-point Likert scale of 1-never, 2-occasionally, and 3-always with a total score ranged from 10 to 30. Those women who scored 80% and above were considered as having good compliance with COVID-19 preventive measures and women who scored less than 80% were grouped as having poor compliance.26,35
Data Quality Control
The data collection tool was first prepared in English then translated into the local language (ie, Amharic), and then back to English to keep its consistency. Both data collectors and supervisors were trained for one day before the actual data collection period. The pre-test of the questionnaire was done on 5% (20 pregnant women) of the sample size at Chacha health center near the study setting. Every day, the supervisor has checkes all the filled questionnaires for completion and clarity.
Data Processing and Analysis
The data were entered using Epi-Data version 4.6 and then exported to SPSS version 25 for data analysis. Descriptive statistics were computed then Bi-variable and multivariable logistic regression analyses were conducted. Variables with P-value < 0.25 in bivariate analysis were entered into multivariable logistic regression analysis. A significant association was declared in multivariable logistic regression analysis based on P-value < 0.05 and AOR with 95% CI. Finally, the results were presented in text, tables, and figures.
Result
Socio-Demographic Characteristics
A total of 396 pregnant women were participated, making the response rate 98.5%. Of the total respondents, 192 (48.5%) of the women were belonged to 25–34 years, with the participants’ ages ranging from 18 to 40 years. The mean age of the participant was 27.23 (SD ± 5.057) years. Two hundred eighty-nine (73%) of participants were from Amhara ethnic group, 274 (69.2%) of women were Orthodox Christian followers in religion, and 383 (96.7%) of them were married (Table 1).
 |
Table 1 Socio-Demographic Characteristics Among Women Attending Antenatal Care at Public Health Facilities of Debre Berhan Town, Ethiopia (n=396) |
Obstetric and Reproductive Health Characteristics
In the current study, about 213 (53.8%) and 108 (50.7%) participants were multigravida and primipara, respectively. Two hundred ten (53%) of the participants attend their antenatal care (ANC) follow-up visit for less than three times in their current pregnancy. According to the findings of this study, 347 (87.6%) and 279 (70.5%) of respondents had a positive attitude towards preventive measures against COVID-19 and a good knowledge of COVID-19 infection, respectively (Table 2).
Compliance with COVID-19 Preventive Measures
According to this study, 222 (56.1%) of pregnant women had good compliance with COVID-19 preventive measures (Figure 1). Of the total respondents, 220 (55.6%) and 177 (44.7%) pregnant women had never avoid close contact with people who are sick/showing symptoms of respiratory disease and greete people with handshaking, hugging and cheek kissing in the past one week, respectively. Similarly, 195 (49.2%) and 109 (27.5%) of participants had never go to the crowded places and history travel out of their home town, respectively. Also, only 39 (9.6%) and 26 (6.6%) of participants always wash their hands frequently with soap/hand sanitizers before and after contacting anyone out of their home and consistently use face mask, respectively (SupplementaryTable 1).
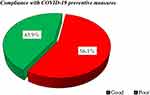 |
Figure 1 Compliance with COVID-19 preventive measures among women attending antenatal care at public health facilities of Debre Berhan town, Ethiopia (n=396). |
Factors of Compliance with COVID-19 Preventive Measures
In bivariable logistic regression analysis; maternal age, educational status, maternal occupation, husband’s educational status, had current chronic diseases, frequency of ANC follow-up, attitude towards COVID-19 preventive measures and Knowledge on COVID-19 preventive measures were entered to multivariable logistic regression analysis. But, in multivariable logistic regression analysis only maternal age, husband’s educational status, current chronic diseases and Knowledge on COVID-19 infection were statistically significant to have good compliance with COVID-19 preventive measures.
Women who were in the 25 years and above age group were more likely to be in good compliance with COVID-19 preventive measures compared to women found in the age group of less than 25 years; (25–34 years) [AOR: 1.926; 95% CI (1.084, 3.421)] and (≥35 years) [AOR: 3.018; 95% CI (1.53, 5.952)]. Women whose husbands had completed secondary education had 3.7 times more likely to have good complying with COVID-19 preventive measures than women whose husbands had no formal education [AOR: 3.68; 95% CI (1.55, 8.737)]. Mothers with current chronic diseases were 2.5 times more likely to be in good compliance with COVID-19 preventive measures compared to their counterparts [AOR: 2.516; 95% CI (1.297, 4.883)]. Mothers who had a good knowledge of COVID-19 infection were 5.5 times more likely to have good compliance with the preventive measures than women who had poor Knowledge [AOR: 5.484; 95% CI (3.057, 9.838)] (Table 3).
Discussion
Pregnant women should have good compliance with COVID-19 to prevent risk of contracting the virus and the adverse maternal and fetal outcomes from the virus.36,37 This study revealed that 222 (56.1%) (95% CI: 51.8, 61.3) of pregnant women had good compliance with COVID-19 preventive measures which is lower than the studies conducted in Guraghe, Ethiopia 76.2%,30 India (67.7–92.7%),38,39 South Africa (76%),40 and low-resource African settings (69.7%).33 The possible variation might be the difference in socio-cultural and demographic characteristics, study setting, and study participants. Also, countries’ health care system in creating community awareness regarding the COVID-19 preventive measures might create a great role for the variation. Furthermore, the education level of the study participants was significantly associated with their Knowledge and attitude towards the preventive measures of COVID-19.41 For instance, the study done in Guraghe found that 49% of the respondents were completed college and above whereas, in our study only 24.5%.
On the contrary, the findings from previous studies done in Wollega Zone (43.6%),42 Debre Tabor (47.6%),43 Ghana (46.6%),44 and low-resource African settings (30.3%)33 which were lower than our finding. The possible discrepancy might be the difference in the study setting, socio-demographic characteristics, and study participants. Studies showed that women who were residing in urban areas were more likely to practice COVID-19 preventive measures than those in rural.33,44 This study was done in the urban area of Debre Berhan town while in Ghana; 58.1% of the participants were lived in a rural area.44 Also, the time of the studies conducted might be the possible reason for the variation; the COVID-19 information dissemination and community awareness creation strategies improve over time.
Pregnant women who were 25 years and above were more likely to engage in good compliance with COVID-19 preventive measures compared to women aged less than 25 years old. This finding supplemented the study done in Ghana; older age women were positively associated with good COVID-19 preventive practices.44 However, it is contrary to the studies conducted in Guraghe31 and Wollega Zone.29 Studies showed that advanced maternal age is one of the risk factor for sever complications and mortality related to COVID-19 during pregnancy.14,45,46 This might be made older age group to have good knowledge of COVID-19 and understanding the severity and its consequences, which ultimately causes to engage in good compliance with preventive measures.
Women whose husbands completed secondary education were more likely to have good compliance with COVID-19 preventive measures than husbands’ with no formal education. This is supported by the study conducted in India, and Debre Tabor; educational status was associated with the level of Knowledge, attitude towards COVID-19 preventive measures and practice.29,38 This could be due to an educated husband being likely to exposed to COVID-19 information via mass media, social media, and others; finally, will influence positively his wife to adhere to COVID-19 preventive measures.
Mothers who had current chronic diseases were more likely to have good compliance with COVID-19 preventive measures than their counterparts. This is consistent with the study done in Ghana.44 This might be due to women perception as; the severity and complication of COVID-19 being more severe among patients with chronic diseases. Also, the study done in Guraghe Zone found that participants who perceived that COVID-19 is worst among people who had chronic diseases were more likely to have good COVID-19 preventive measures.30 In addition, studies revealed that severe complications and fatalities occur in people with chronic diseases such as hypertension, diabetes, and respiratory chronic diseases.45–47
Moreover, knowledge was one of the factor that significantly associated to good compliance with COVID-19 preventive measures. Study participants who had a good knowledge of COVID-19 infection were more likely to have good compliance with COVID-19 preventive measures than their counterparts. This finding is consistent with the study conducted in Nigeria and Debre Tabor; women’s Knowledge on COVID-19 had a substantial impact on the attitude and practice of the preventive measures.29,43,48 The reason for this could be that knowing about COVID-19 preventive measures enhances the level of understanding about its consequences, which in turn determines to have good compliance.
Conclusion
The finding of this study revealed that 56.1% of pregnant mothers had good compliance with COVID-19 preventive measures. Good compliance of COVID-19 preventive measures associated with; maternal age, husband educational status, current chronic diseases and having good knowledge on COVID-19 preventive measures. Therefore, COVID-19 prevention and control programmers, North Shoa zone health office, and healthcare providers should scale up the community awareness in all aspects via different mass-media campaigns, and for women who had no pre-existing chronic diseases, as well as those who were in the young age group should be given special consideration to improve the compliance. Finally, the authors recommended further studies by addressing qualitative data and longitudinal research to identify the effect of compliance with COVID-19 preventive measures on pregnancy outcomes.
Abbreviations
ANC, Antenatal Care; AOR, Adjusted Odd Ratio; CI, Confidence Interval; COR, Crude odds ratio; COVID, Corona Virus Disease; SD, Standard Deviation; QOL, Quality Of Life; WHO, World Health Organization.
Ethics Approval
Ethical clearance and approval letter to conduct the study was obtained from Debre Berhan University institutional review board (IRB) before data collection. Also, written permission letters to conduct the study were obtained from each public health facility. After the objective of the study was explained to the participants, written informed consent was obtained from each participant. Data were kept confidential and coded instead of the name of the participants. Generally, all methods in the study were carried out in accordance with the declaration of Helsinki as a statement of ethical principles for medical research involving human subjects.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi:10.1016/S0140-6736(20)30185-9
2. Margallo LN, Diaz M, Lim PP. 2019 novel coronavirus pandemic: what do we know. SD Med. 2020;73:262–264.
3. Cao Y, Hiyoshi A, Montgomery S. COVID-19 case-fatality rate and demographic and socioeconomic influencers: worldwide spatial regression analysis based on country- level data. BMJ Open. 2020;10:e043560. doi:10.1136/bmjopen-2020-043560
4. World Health Organization. WHO coronavirus disease (COVID-19) Dashboard; 2021. Available from: https://covid19.who.int/%0Ahttps://covid19.who.int/?gclid=CjwKCAjwnK36BRBVEiwAsMT8WJ3y00_BUzvrLsvbl3uthuoTH_Occ45gyEUbpYRyEqAzll3aZB6TYxoCcM0QAvD_BwE.
5. World Health Organization. Updated WHO advice for international traffic in relation to the outbreak of the novel coronavirus 2019-nCoV; 2020.
6. Abdo RA, Endalemaw T, Tesso F. Prevalence and associated factors of adverse birth outcomes among women attended maternity ward at Negest Elene Mohammed Memorial General Hospital in Hosanna Town, SNNPR, Ethiopia. J Women’s Heal Care. 2016;5(4):1000324. doi:10.4172/2167-0420.1000324
7. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. doi:10.1016/j.tmaid.2020.101623
8. Liu H, Wang LL, Zhao SJ, Kwak-Kim J, Mor G, Liao AH. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020;139:103122. doi:10.1016/j.jri.2020.103122
9. Lim LM, Li S, Biswas A, Choolani M. Special Report and pregnancy. Am J Obstet Gynecol. 2020;222(6):521–531. doi:10.1016/j.ajog.2020.03.021
10. Haft JW, Atluri P, Ailawadi G, et al. Adult cardiac surgery during the COVID-19 pandemic: a tiered patient triage guidance statement. Ann Thorac Surg. 2020;110(2):697–700. doi:10.1016/j.athoracsur.2020.04.003
11. Centers for Disease Control and Prevention. Pregnant and recently pregnant people. Centers for Disease Control and Prevention; 2021. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html.
12. Diriba K, Awulachew E, Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):1–14. doi:10.1186/s40001-020-00439-w
13. Liang H, Acharya G. Novel Corona virus disease (COVID-19) in pregnancy: what clinical recommendations to follow? Acta Obstet Gynecol Scand. 2020;99(4):439–442. doi:10.1111/aogs.13836
14. Allotey J, Stallings E, Bonet M, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370. doi:10.1136/bmj.m3320
15. Gajbhiye RK, Sawant MS, Kuppusamy P, et al. Differential impact of COVID-19 in pregnant women from high-income countries and low- to middle-income countries: a systematic review and meta-analysis. Int J Gynecol Obstet. 2021;155(1):48–56. doi:10.1002/ijgo.13793
16. Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021;193(16):E540–E548. doi:10.1503/cmaj.202604
17. Chmielewska B, Barratt I, Townsend R, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Heal. 2021;9(6):e759–e772. doi:10.1016/S2214-109X(21)00079-6
18. Panahi L, Amiri M, Pouy S. Risks of novel coronavirus disease (COVID-19) in pregnancy; a narrative review. Arch Acad Emerg Med. 2020;8(1):1–5.
19. James JL, Stone PR, Chamley LW. The regulation of trophoblast differentiation by oxygen in the first trimester of pregnancy. Hum Reprod Update. 2006;12:137–144. doi:10.1093/humupd/dmi043
20. Martinez-Portilla RJ. Vertical transmission of coronavirus disease 2019. Am J Obstet Gynecol. 2021;224(3):328–329. doi:10.1016/j.ajog.2020.11.013
21. Chi J, Gong W, Gao Q. Clinical characteristics and outcomes of pregnant women with COVID-19 and the risk of vertical transmission: a systematic review. Arch Gynecol Obstet. 2021;303(2):337–345. doi:10.1007/s00404-020-05889-5
22. Benson S. Social support during pregnancy: effects on maternal depressive symptoms, smoking and pregnancy outcome. Hum Reprod. 2007;22:869–877. doi:10.1093/humrep/del432
23. Dule A, Hajure M, Mohammedhussein M. Health-related quality of life among Ethiopian pregnant women during COVID-19 pandemic. Brain Behav. 2021;11:e02045. DOI:10.1002/brb3.2045
24. Molgora S, Accordini M. Motherhood in the time of coronavirus: the impact of the pandemic emergency on expectant and postpartum women ’ s psychological well-being. Front Psychol. 2020;11:1–16. doi:10.3389/fpsyg.2020.567155
25. Shuka Z, Zewdu GA. Containing the spread of COVID-19 in Ethiopia. J Global Health. 2020. doi:10.7189/jogh.10.010369
26. Etafa W, Gadisa G, Jabessa S, Takele T. Healthcare workers’ compliance and its potential determinants to prevent COVID-19 in public hospitals in Western Ethiopia. BMC Infect Dis. 2021;21(1):1–8. doi:10.1186/s12879-021-06149-w
27. Bante A, Mersha A, Tesfaye A, et al. Adherence with COVID-19 preventive measures and associated factors among residents of Dirashe district, southern Ethiopia. Patient Prefer Adherence. 2021;15:237–249. doi:10.2147/PPA.S293647
28. Yehualashet SS, Asefa KK, Mekonnen AG, et al. Predictors of adherence to COVID-19 prevention measure among communities in North Shoa Zone, Ethiopia based on health belief model: a cross-sectional study. PLoS One. 2021;16:1–16. doi:10.1371/journal.pone.0246006
29. Degu A, Nibret G, Gebrehana H, Getie A, Getnet B. Knowledge and attitude towards the current pandemic Corona virus disease and associated factors among pregnant women attending antenatal care in Debre Tabor general hospital northwest Ethiopia: an institutional-based cross-sectional study. Int J Womens Health. 2021;13:61–71. doi:10.2147/IJWH.S285552
30. Fikadu Y, Yeshaneh A, Melis T, Mesele M, Anmut W, Argaw M. Covid-19 preventive measure practices and knowledge of pregnant women in guraghe zone hospitals. Int J Womens Health. 2021;13:39–50. doi:10.2147/IJWH.S291507
31. Azene ZN, Merid MW, Muluneh AG, et al. Adherence towards COVID-19 mitigation measures and its associated factors among Gondar City residents: a community-based cross-sectional study in Northwest Ethiopia. PLoS One. 2020;15:1–15. doi:10.1371/journal.pone.0244265
32. W/ Mariam TG, Kassie BA, Asratie MH, Abate AT. The effects of fear and knowledge of COVID-19 on preventive practice among pregnant women who attend antenatal care in Northwest Ethiopia, 2020: institution-based cross-sectional study. Int J Womens Health. 2021;13:95–100. doi:10.2147/ijwh.s286088
33. Nwafor JI, Aniukwu JK, Anozie BO, Ikeotuonye AC, Okedo-Alex IN. Pregnant women’s knowledge and practice of preventive measures against COVID-19 in a low-resource African setting. Int J Gynecol Obstet. 2020;150(1):121–123. doi:10.1002/ijgo.13186
34. Yesse M, Muze M, Kedir S, et al. Assessment of knowledge, attitude and practice toward COVID-19 and associated factors among health care workers in Silte Zone, Southern Ethiopia. PLoS One. 2021;16(10):e0257058. doi:10.1371/journal.pone.0257058
35. Belete ZW, Berihun G, Keleb A, et al. Knowledge, attitude, and preventive practices towards COVID-19 and associated factors among adult hospital visitors in South Gondar Zone Hospitals, Northwest Ethiopia. PLoS One. 2021;16:1–18. doi:10.1371/journal.pone.0250145
36. World Health Organization. Coronavirus disease (COVID-19): pregnancy and childbirth. World Health Organization; 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-pregnancy-and-childbirth.
37. Apanga PA, Kumbeni MT. Adherence to COVID-19 preventive measures and associated factors among pregnant women in Ghana. Trop Med Int Heal. 2021;26(6):656–663. doi:10.1111/tmi.13566
38. Shivanagappa M, Bhavana YS, Chandrashekarappa SM. Pregnant women’s knowledge and practice of preventive measures against COVID-19: a study from Mysore city, Karnataka, India. Int J Reprod Contraception Obstet Gynecol. 2020;9(9):3622. doi:10.18203/2320-1770.ijrcog20203830
39. Kamal D, Thakur V, Swain S, Vikneshram C. Knowledge, attitude, and practice toward COVID-19 among pregnant women in a tertiary care hospital during the COVID-19 outbreak. J Mar Med Soc. 2020. doi:10.4103/jmms.jmms_81_20
40. Hoque AM, Alam AM, Hoque M, Hoque ME, Van Hal G. Knowledge, attitudes, and practices towards COVID-19 of pregnant women at a primary health care facility in South Africa. Eur J Med Heal Sci. 2021;3(1):50–55. doi:10.24018/ejmed.2021.3.1.654
41. Adegoke JI, Ajibade BL, Rhoda D. Knowledge, attitude and practice of preventive measures towards COVID-19 among pregnant women attending selected primary health centre’s in Osogbo, Osun state. Int J Nursing Midwife Heal Relat Cases. 2020;6(2):29–45.
42. Besho M, Tsegaye R, Yilma MT, et al. Knowledge, attitude and practice toward Corona virus infection among pregnant women attending antenatal care at public hospitals in three wollega zones, Ethiopia. Int J Gen Med. 2021;14:3563–3573. doi:10.2147/IJGM.S295490
43. Ayele AD, Mihretie GN, Belay HG, Teffera AG, Kassa BG, Amsalu BT. Knowledge and practice to prevent COVID-19 and its associated factors among pregnant women in Debre Tabor Town Northwest Ethiopia, a community-based cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):1–12. doi:10.1186/s12884-021-03877-4
44. Kumbeni MT, Apanga PA, Yeboah EO, Lettor IBK. Knowledge and preventive practices towards COVID-19 among pregnant women seeking antenatal services in Northern Ghana. PLoS One. 2021;16(6):e0253446. doi:10.1371/journal.pone.0253446
45. Eastin C, Eastin T. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. J Emerg Med. 2020;58(4):713–714. doi:10.1016/j.jemermed.2020.04.007
46. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
47. Yang J, Zheng Y, Gou X, Pu K, Chen Z. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi:10.1016/j.ijid.2020.03.017
48. Anikwe CC, Ogah CO, Anikwe IH, Okorochukwu BC, Ikeoha CC. Coronavirus disease 2019: knowledge, attitude, and practice of pregnant women in a tertiary hospital in Abakaliki, southeast Nigeria. Int J Gynecol Obstet. 2020;151(2):197–202. doi:10.1002/ijgo.13293
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


