Back to Journals » Clinical and Experimental Gastroenterology » Volume 11
Complete esophageal obstruction following endoscopic variceal ligation: a case report and literature review
Authors Kubovy J, Boswell TD, Vautier G, Arnold MM
Received 6 January 2018
Accepted for publication 23 February 2018
Published 10 April 2018 Volume 2018:11 Pages 165—168
DOI https://doi.org/10.2147/CEG.S161772
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Everson L.A. Artifon
Jan Kubovy, Tom D Boswell, Guy Vautier, Malcolm M Arnold
Department of Gastroenterology, Hawkes Bay Hospital, Hastings, New Zealand
Abstract: Endoscopic variceal ligation (EVL) is an important treatment modality in managing complications of portal hypertension. Since its advent 30 years ago, the procedural complications have decreased significantly, especially when compared with variceal sclerotherapy. With the current widespread use of EVL, rare complications are now becoming increasingly recognized. We present a case of complete esophageal obstruction, its management, and clinical course. Our literature review identified only eight reported cases. We compare the varied treatment approaches and outcomes in the cited articles.
Keywords: portal hypertension, esophageal varices, endoscopic variceal ligation, esophageal obstruction
Introduction
Portal hypertension of any etiology can be associated with esophageal varices. This carries a risk of bleeding. Endoscopic variceal ligation (EVL) is currently regarded as the treatment of choice for both esophageal variceal bleed prophylaxis as well as acute hemostasis.1,2 Although EVL is considered to be a safe intervention, complications can and do occur.3 The most common are postprocedural pain, dysphagia, delayed ulcer bleeding, and chronic esophageal strictures.4 We present a particularly rare complication, a case of complete esophageal obstruction. We also compare the varied management approaches and their outcomes of the very few cases found in published literature. We hope this may provide a reference point for clinicians facing this rare and challenging complication.
Case report
This patient has provided written informed consent in regard to publishing her case.
A 62-year-old Caucasian woman underwent elective EVL as primary prophylaxis. Her portal hypertension was related to seronegative autoimmune liver disease with cholangiopathy (baseline Model for End-stage Liver Disease score-7, all values within normal limits). Comorbidities included ulcerative colitis, mild chronic obstructive pulmonary airway disease, and recurrent deep venous thrombosis. Relevant pharmacotherapy included ursodeoxycholic acid, 6-mercaptopurine, mesalazine, omeprazole, and propranolol (only able to tolerate low dose due to excessive fatigue).
Surveillance esophago-gastro-duodenoscopy (OGD) demonstrated variceal formation (3 columns of grade 2 varices, all >5 mm in size) despite the above beta-blocker regimen, and a decision was made for endoscopic ablation.
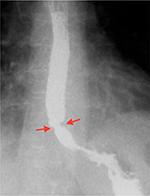
The OGD resulting in the complication under discussion took place 4 weeks after application of two bands on two separate varices. This second procedure showed a single remaining varix in the 2 o’clock position without obvious scarring, but perhaps with a minor narrowing of the distal esophagus (Figure 1). The remaining varix was banded 2 cm above the gastro-esophageal junction (GOJ) applying a single band using Saeed Multi-band Ligator 6-shooter (MBL-U-6, Cook Medical).
  | Figure 1 Index OGD showing a single remaining varix in 2 o’clock position. Notes: Arrows indicate the culprit varix prior to banding. Abbreviation: OGD, esophago-gastro-duodenoscopy. |
The patient developed severe retrosternal pain followed by retching and vomiting in the recovery room. This was successfully managed with antiemetics and analgesia, and she was discharged pain-free and without nausea or vomiting.
She presented 3 days later to the emergency department with chest pain and aphagia (unable to tolerate even sips of water).
Serum biochemistry indicated acute kidney injury, and her chest X-ray was unremarkable.
The initial management was conservative as further intervention was considered too risky. Treatment included intravenous fluids, omeprazole, antiemetics, and a trial of dexamethasone. As there was no symptomatic improvement on day 3 of her admission (6 days after the procedure), further OGD was performed. The findings were of a nubbin of necrotic tissue encased by a visible band in the distal esophagus and a small amount of food residue above it (Figure 2). The lumen was not able to be identified. A computed tomography scan of her chest demonstrated distal esophageal wall thickening and a soft tissue nodule (likely representing the banded varix) just above the GOJ, but without other complications (Figure 3).
  | Figure 2 Necrotic banded varix in 2 o’clock position with some food residue. Note: The arrows indicate the position of the band. |
Total parenteral nutrition was established via a peripherally inserted central catheter. Progress thereafter was slow with a negligible oral fluid intake on day 17, barium swallow at that time indicating delayed esophageal clearance with an underlying stricture (Figure 4). Further complications during the admission occurred, namely, peripherally inserted central catheter-related deep venous thrombosis and exacerbation of ulcerative colitis. Total parenteral nutrition was discontinued after 14 days. Total length of stay was 20 days.
  | Figure 4 Distal esophageal stricture seen on barium swallow study on day 17. Note: The arrows indicate distal esophageal stricture. |
Repeat OGD 42 days after the procedure revealed a patent esophagus with a mild stricture and a semicircular scar just above the GOJ (Figure 5).
  | Figure 5 Semicircular scar in distal esophagus 42 days after the index procedure. Note: The arrows indicate the scar. |
Discussion
Complete esophageal obstruction as a complication of EVL is exceedingly rare. Our literature search identified only eight cases of this since the advent of EVL 30 years ago.5–12
The mechanism is thought to be multifactorial: a large engorged banded varix causing a “plug”; excessive use of suction resulting in extra-variceal mucosal encasement; or even banding opposing walls of esophagus; surrounding tissue edema; impaired lower esophageal sphincter relaxation; altered esophageal motility post EVL; hematoma; and predisposing underlying esophageal stricture from previous banding.
In our case, we believe the obstruction may have been caused by encasing a large portion of the surrounding mucosa as well as the varix on a background of chronic stricture related to previous EVL.
The available literature experience regarding appropriate management of this complication is divided between conservative and urgent intervention.5–12
The conservative approach is based on the premise that this is likely to be a self-limiting condition, with an emphasis on supportive care alone.5–8 The average time until the resumption of liquid diet was 4 days.
Advocates of urgent reintervention aim to dislodge/remove the variceal band mechanically, thus relieving the obstruction. Several such methods have been applied: a “bottle opener” technique with a capped endoscope;9 a simple band dislodgement with the tip of the scope;10 the use of biopsy forceps, rat-tooth forceps or hot biopsy forceps,11,12 or a reusable loop cutter.12
It is conceivable that further complications may arise from these procedures. Successful removal of the band and resolution of the obstruction was achieved in three out of the four interventional cases. One case, however, was complicated by a 6 cm intramural esophageal dissection and bleeding (this was managed conservatively).11
We perceive the risk–benefit ratio to be in favor of the conservative approach.
Nonetheless, early intervention may be more cost-effective if successful, thus potentially avoiding prolonged hospital admission with further complications, as demonstrated in our case.
Only the most experienced endoscopists should attempt to intervene in this scenario.
Conclusion
EVL-related complete esophageal obstruction is very rare. Recognition of possible precursors, especially underlying luminal narrowing, may aid in the prevention of this complication. The risk–benefit and cost-effectiveness of early interventional versus conservative management is unclear at this point.
Disclosure
The authors report no conflicts of interest in this work.
References
Thiele M, Krag A, Rohde U, Gluud LL. Meta-analysis: banding ligation and medical interventions for the prevention of rebleeding from oesophageal varices. Aliment Pharmacol Ther. 2012;35(10):1155–1165. | ||
Lo GH, Lai KH, Cheng JS, et al. A prospective, randomized trial of sclerotherapy versus ligation in the management of bleeding esophageal varices. Hepatology. 1995;22(2):466–471. | ||
Schmitz RJ, Sharma P, Badr AS, Qamar MT, Weston AP. Incidence and management of esophageal stricture formation, ulcer bleeding, perforation, and massive hematoma formation from sclerotherapy versus band ligation. Am J Gastroenterol. 2001;96(2):437–441. | ||
Rai RR, Nijhawan S, Singh G. Post-ligation stricture: a rare complication. Endoscopy. 1996;28(4):406. | ||
Nikoloff MA, Riley III TR, Schreibman IR. Complete esophageal obstruction following endoscopic variceal ligation. Gastroenterol Hepatol. 2011;7(8):557. | ||
Elizondo-Rivera RL, González-González JA, Garcia-Compean D, Maldonado-Garza HJ. Complete esophageal obstruction after endoscopic variceal band ligation. Endoscopy. 2014;46(Suppl 1): E457–E458. | ||
Dilshad A, Ahmad I, Niazi AK, Zubair M, Khalid U. Severe dysphagia after endoscopic variceal band ligation: a case report. Proceeding S.Z.P.G.M.L. 2003;17(2):91–92. | ||
Saltzman JR, Arora S. Complications of esophageal variceal band ligation. Gastrointest Endosc. 1993;39(2):185–186. | ||
De Melo SW. Complete esophageal occlusion after band ligation. Endoscopy. 2011;43(S 02):E259. | ||
Sarwar FC, Batul MB. Complete esophageal occlusion following esophageal variceal band ligation: an unusual complication; a case report. Visible Hum J Endosc. 2010;9(1). | ||
Chahal H, Ahmed A, Sexton C, Bhatia A. Complete esophageal obstruction following endoscopic variceal band ligation. J Community Hosp Intern Med Perspect. 2013;3(1):20043. | ||
Kwiatt JT, Merchant P. Successful removal of an esophageal band causing complete esophageal obstruction after variceal ligation. Gastrointest Endosc. 2016;83(5):1030–1031. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

