Back to Journals » Clinical Ophthalmology » Volume 10
Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens
Authors Gundersen KG , Potvin R
Received 30 December 2015
Accepted for publication 11 February 2016
Published 17 March 2016 Volume 2016:10 Pages 455—461
DOI https://doi.org/10.2147/OPTH.S103375
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Kjell Gunnar Gundersen,1 Rick Potvin2
1IFocus Øyeklinikk AS, Haugesund, Norway; 2Science in Vision, Akron, NY, USA
Purpose: The aim of this study was to compare a new diffractive trifocal toric lens with an apodized diffractive bifocal toric lens in terms of refractive and visual acuity (VA) outcomes, including low-contrast VA (LCVA), as well as the patient’s visual function 3 months after implantation.
Patients and methods: This is a randomized prospective study involving bilateral implantation of a trifocal toric or a bifocal toric lens. At 3 months postoperatively, the subject’s vision was tested both uncorrected and with his/her best distance correction at: distance (4 m), intermediate (63 cm), and near (40 cm). Binocular defocus curves were measured with no correction and with the subject’s best distance correction in place. Quality of vision was measured using the National Eye Institute Visual Function Questionnaire.
Results: A total of 22 patients were enrolled (eleven in each group). There was no statistically significant difference in the absolute change in measured rotation between 1 month and 3 months postoperatively between the two intraocular lens (IOL) groups (P=0.98). At 3 months, the postoperative refraction and distance VA by eye were similar between groups. There was no statistically significant difference in the measured LCVA between groups (P=0.39). The defocus curve showed that at 67 cm, the trifocal toric lens had statistically significantly better VA when compared to the bifocal toric lens. There were no statistically significant differences by group for any of the National Eye Institute Visual Function Questionnaire scores (P>0.26 in all cases).
Conclusion: The trifocal toric IOL improved the intermediate vision without negatively impacting visual function and distance, near, or low-contrast VA when compared to a bifocal toric IOL. The toric component of the trifocal lens effectively reduced astigmatism and provided good rotational stability.
Keywords: FineVision, ReSTOR, astigmatism, multifocal, defocus curve, contrast sensitivity
Introduction
A high demand for presbyopia correction at the time of cataract surgery has increased the implantation of multifocal intraocular lenses (IOLs). Residual astigmatism is a concern with these lenses, because refractive astigmatism of 1.0 D or more can negatively impact visual outcomes with multifocal IOLs.1 This amount of astigmatism may be encountered in ~40% of patients presenting for routine cataract surgery2 and must be managed in multifocal patients to reduce potential dissatisfaction with the visual outcome. Two of the most common approaches to reduce astigmatism at the time of cataract surgery are using corneal relaxing incisions and/or toric IOLs. Correcting astigmatism with corneal relaxing incisions can be more variable with lower effectivity, predictability, and stability than with toric IOLs.3,4 As such, astigmatic correction with a toric multifocal IOL is a desirable alternative.
Some studies related to multifocal toric IOLs have been published in the literature, but they are limited to accommodative toric or bifocal toric designs, and we are only aware of one study discussing the clinical outcomes with an accommodative toric IOL.5 Studies of bifocal toric IOLs are more common. These lenses are available in a refractive and a diffractive design. The refractive design has specific areas in the lens designed for either near vision or distance vision increasing their dependence on pupil size and need for proper alignment. The diffractive design splits incoming light, with one focus for distance images and the other for near images; such designs have the potential to decrease contrast sensitivity.
One of the most studied diffractive bifocal toric IOLs (AcrySof ReSTOR SND1T; Novartis AG, Basel, Switzerland) has been shown to be effective at significantly improving near vision while maintaining good distance vision and providing similarly reliable astigmatism correction when compared to an aspheric monofocal toric IOL (AcrySof Toric SN6AT; Alcon, Inc.). Glare and halos are more common, and low-contrast sensitivity and low-contrast visual acuity (LCVA) are reported to be poorer with multifocal IOLs compared to monofocal IOLs, but this is unlikely related to the addition of the toric correction to the multifocal IOL.6,7 A primary concern with using a bifocal IOL is that it does not provide an intermediate focal point; a bench study has demonstrated that this can reduce the potential for adequate intermediate vision.8 With the proliferation of handheld devices, intermediate vision has become a significant concern for patients.
The FineVision IOL (PhysIOL®; FineVision Toric, Liège, Belgium) is a diffractive trifocal IOL that provides an intermediate focus at 1.75 D and a near focus at 3.5 D (both at the IOL plane). This corresponds to a nominal intermediate add of approximately +1.15 D and near add of about +2.25 D at the corneal plane, depending on the geometry of the patient’s eye. This intermediate focal point is expected to improve patient satisfaction relative to bifocal IOLs, since bifocal IOLs have a greater drop off in visual acuity (VA) in the intermediate range.9 There is a concern that the addition of a third focal point may increase halos.10 However, a relatively small percentage of energy is dedicated to intermediate vision when compared to distance and near vision; as such, photic phenomena and contrast sensitivity are unlikely to be more problematic with this diffractive trifocal IOL than they are for any other diffractive bifocal IOL.11,12 Results in 198 eyes of 99 patients implanted with this diffractive trifocal IOL show that the lens provides good near, intermediate, and distance vision under different illuminations with high patient satisfaction.13
A new diffractive trifocal toric IOL is now available (PhysIOL®, POD AY 26P F-T; FineVision Toric); it utilizes the same multifocal principles as the FineVision trifocal IOL and the same toric principles as the Ankoris IOL (PhysIOL®; Ankoris, Liège, Belgium).14 The Ankoris IOL is a hydrophilic aspheric toric IOL utilizing double-C loop quadripode haptics for stabilization.15 The purpose of the current study is to compare the refractive and VA outcomes, including LCVA, as well as the patient’s visual function 3 months after implantation of this new diffractive trifocal toric IOL with the ReSTOR SND1T apodized diffractive bifocal toric IOL.
Patients and methods
This study was a single-site, single-surgeon, randomized prospective study involving bilateral implantation of a trifocal toric IOL in one group and a bifocal toric IOL in the other group during one session. The Regional Committees for Medical and Health Research Ethics (REK), Norway reviewed and approved the study and patient informed consent. The study was powered sufficiently to detect a 0.5 line difference in logMAR acuity based on data in the literature. A total of eleven subjects were enrolled in each group.
Subjects were eligible for inclusion if they were >50 years old, had presented for uncomplicated cataract surgery, and were interested in reducing their dependence on glasses for daily life. They had to have regular corneal astigmatism and have a calculated IOL power that was within the available range for each IOL type. All subjects had to be willing and able to sign the informed consent for the study. The surgeon evaluated the interest of the patient in spectacle independence, their affect, and their expectations. If expectations were unrealistic, they were excluded from the study. Additional exclusion criteria included ocular pathology (besides cataract) and previous refractive surgery. If the surgeon felt there were factors that would be likely to affect the subject’s postoperative vision (eg, amblyopia and history of uveitis), the surgeon could exclude the subject.
All subjects had a preoperative examination that included refraction, topography, keratometry, biometry, and a slit-lamp examination, after which, if eligible, they were asked to participate. Toric IOL calculations were performed using the standard calculation for the AcrySof lens (www.acrysoftoriccalculator.com) and for the Physiol lens (www.physioltoric.eu). All subjects were implanted bilaterally at a single visit using the standard phacoemulsification procedure at the site; procedures were completed without any use of femtosecond laser systems. Any surgical complications resulted in the subject being exited from the study, and replaced.
At 3 months postoperatively, the subject’s vision was tested both uncorrected and with his/her best distance correction at: distance (4 m), intermediate (63 cm), and near (40 cm). The examiner was not masked to the lens type, but the manifest refraction was determined for both groups using the standard methodology for the site, including the use of high-contrast logMAR acuity charts. Binocular defocus curves were measured with no correction and with the subject’s best distance correction in place. Quality of vision was measured using the National Eye Institute Visual Function Questionnaire (NEI VFQ)-25. The NEI-VFQ was developed at the RAND under the sponsorship of the NEI; it provides a self-reported measure of visual function.16
The data were imported into an MS Access database for data checking, collation, and preliminary analysis (Microsoft Corporation, Redmond, WA, USA). Statistical analyses were performed using the STATISTICA data analysis software system, Version 12 (StatSoft, Inc., www.statsoft.com). Statistical testing was performed using analysis of variance on continuous variables and appropriate nonparametric tests on categorical data. Statistical significance was set at P=0.05.
Results
A total of 22 patients were successfully enrolled, with no complications requiring any patients to exit the study. The preoperative demographics for both groups are shown in Table 1. As can be seen, the breakdown by sex was similar. The average age in the trifocal group was 8 years lower than the bifocal group, a statistically significant difference (P=0.02). The trifocal group also had a statistically significantly higher average keratometry (P=0.01), but the average corneal astigmatism measured in both groups was similar (P=0.58). There was no statistically significant difference in the measured axial length (P=0.57).
  | Table 1 Demographics by group (n=11 in each group) |
The surgically induced astigmatism (SIA) was calculated for each eye based on the difference in the measured corneal astigmatism preoperatively and at 3 months postoperatively. There was no statistically significant difference in the measured magnitude of the SIA between groups (P=0.07). The average SIA magnitude was 0.49 D ±0.36 D, while the calculated centroid (the vector sum of all SIA measures) for both groups was between 0.10 D and 0.15 D.
An intended lens orientation was available at the time of surgery, and lens orientation was measured at each follow-up visit. There were only two lenses with a measured change in orientation of >5° between the 1-day and 1-month postoperative visits, one bifocal lens, and one trifocal lens; the maximum measured change was 7°. There was no statistically significant difference in the change of lens orientation between the 1-day and 1-month postoperative visits between IOL groups (P=0.07).
In three of the cases involving trifocal IOLs, the 1-month postop orientation of the lens was noted to be ~10° from intended. A chart review showed a similar but slightly lower alignment error 1 day postoperatively suggesting an alignment error rather than actual IOL rotation. These three lenses were reoriented to the intended angle between the 1-month and 3-month postoperative visits. With these manual exceptions, no change of lens orientation of >5° was measured between the 1-month and 3-month visits for either lens. There was a statistically significant difference between the trifocal and bifocal groups in the change in lens orientation between the 1-month and 3-month postoperative visits (P<0.01); the difference was <2°. The bifocal lenses appeared to rotate slightly more clockwise and the trifocal lenses appeared to rotate slightly more counterclockwise, with average measured rotation <1° in both cases. There was no statistically significant difference in the absolute change in measured rotation between 1 month and 3 months postoperatively between the two IOL groups (P=0.98). There was also no statistically significant correlation between change in lens orientation and axial length for either lens (P>0.05).
At 3 months, the postoperative refraction and distance VA by eye were similar between groups. Table 2 summarizes the data. Average uncorrected logMAR VA in the trifocal group was about a half line better than in the bifocal group, which is presumably associated with the slightly lower (0.19 D) residual refractive cylinder, but neither of these differences was statistically significant. The percentage of eyes with ≤0.5 D of refractive cylinder at 3 months was slightly higher in the trifocal group (82%, 18/22) relative to the bifocal group (68%, 15/22), but the difference was not statistically significant (Fisher’s exact test, two-tailed, P=0.48).
  | Table 2 VA and refractive data 3 months postoperatively (by eye, n=22 in each group) |
The distribution of uncorrected binocular VA measured at the three test distances is shown in Figure 1. There was no statistically significant difference in the measured VA at any distance between the groups. There was a higher number of subjects with 20/25 uncorrected VA at 63 cm in the trifocal group (ten of eleven vs seven of eleven in the bifocal group), but the difference was not statistically significant (Fisher’s exact test, one-tailed, P=0.16). Similar results were obtained for the best distance-corrected VA, with no statistically significant difference between groups at any distance. At 63 cm, 82% of eyes (9/11) with the trifocal toric IOL had a best distance-corrected VA equal to or better than 0.1 logMAR (20/25 Snellen), compared to 64% of eyes (7/11) with the bifocal toric IOL; the difference was not statistically significant (Fisher’s exact test, one-tailed, P=0.18).
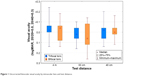  | Figure 1 Uncorrected binocular visual acuity by intraocular lens and test distance. |
LCVA was tested binocularly with the subject’s best distance correction in place using a target at 4 m and a letter contrast of 10%. There was no statistically significant difference in the measured LCVA between groups (P=0.39).
Figure 2A shows the uncorrected binocular defocus curve, and Figure 2B shows the best distance-corrected binocular defocus curve for the two groups. Results were not statistically significantly different at any test distances except +2.0 (not clinically relevant) and -1.5 D, corresponding to a reading distance of ~67 cm. At both these levels of defocus, subjects implanted with the trifocal IOL had statistically significantly better VA.
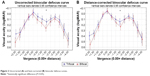  | Figure 2 Uncorrected (A) and best-corrected (B) binocular defocus curves. |
The questionnaire results from the NEI-VFQ were tabulated, and the subgroup scores for general vision, distance vision, near vision, and driving were compared between groups. Figure 3 shows the distribution of these subgroup scores by the IOL group. There were no statistically significant differences by the IOL group for any of these subgroup scores (P>0.26 in all cases).
  | Figure 3 NEI-VFQ subscale scores by intraocular lens type. |
Discussion
In this study, statistically significant differences in preoperative average keratometry and patient age were found between groups, despite randomization, but the differences were not considered clinically significant. The small sample size is likely a contributing factor. More importantly, there was no statistically significant difference in the level of corneal astigmatism between groups.
The bifocal toric IOL is based on a modified L haptic design, while the trifocal toric IOL uses a double C-loop quadripod.15 Despite these design differences, the correction of astigmatism was effective and stable in both groups. Three cases in the trifocal group required reorientation because of minor misalignment at the time of surgery. Lens alignment was stable in both IOL groups, varying only within a 5° range up to 3 months postoperatively. Rotational stability has been documented previously for both IOL groups; the toric component of the trifocal IOL has been shown to have a mean rotation of ~2°.6,14
At 3 months, the postoperative astigmatism was slightly less (0.19 D) in the trifocal toric group when compared to the bifocal toric group, but the difference was not statistically significant. The mean postoperative astigmatism in the bifocal toric group in this study was consistent with the average of the mean postoperative astigmatism reported in two previous studies using the same lens.6,7 The spherical equivalent refraction for the bifocal toric IOL group in the current study was also the same as that reported in a larger study of the same lens.7 The mean postoperative astigmatism in the trifocal toric group was 0.3 D in the current study, which is slightly lower than the 0.4 D mean reported by a previous study of the same toric lens design.14
The VA results were similar between the two groups at all distances. The mean uncorrected distance visual acuities for both groups were reasonably consistent with previously reported values for the bifocal toric group and the multifocal component of the trifocal toric group.7,13 This is not unexpected, as both lenses use a similar diffractive multifocal design. It is worth noting that the additional intermediate focal point in the trifocal lens did not appear to negatively impact distance or near vision.
The binocular defocus curves in Figure 2 show that the trifocal toric group had statistically significantly better VA at -1.5 D (corresponding to the vision of a target at 67 cm) when compared to the bifocal toric group. A previous bench study comparing the multifocal component of both lenses found that the trifocal lens provides a true third intermediate focal point that is not found with the bifocal lens.8 Clinical studies evaluating the bifocal toric IOL and the multifocal component of the trifocal toric IOL provided similar defocus curves to the one shown in the current study.7,13 These studies noted a similar drop in the intermediate vision with the bifocal IOL relative to the trifocal IOL.
There is always some concern that the additional focal point provided by a trifocal IOL may reduce visual quality more than bifocal IOLs, as a result of splitting the light into three foci.10 One objective measure of this is LCVA. In the current study, the VA under low contrast was similar between the trifocal and bifocal groups. Previous studies have found LCVA (10%) to be better than reported here for the trifocal toric IOL group and worse than reported here for the bifocal toric IOL group, though different testing methods may have been used and the previous trifocal IOL data did not include the toric component.6,13
Another common measure of overall visual function is the NEI-VFQ questionnaire; all subjects in the current study completed the questionnaire. The subscales for general vision, near vision, distance vision, and driving showed no statistically significant differences between the bifocal and trifocal IOLs, with median subscore values ≥80 in all cases, suggesting high satisfaction with postoperative vision. A high level of satisfaction related to near vision in subjects undergoing bifocal toric IOL implantation has previously been reported.6 A high level of satisfaction based on the patients’ answer to whether or not they would have the same lens implanted again in those that underwent trifocal IOL implantation has also been documented.13
Conclusion
In conclusion, the trifocal toric IOL provided improved intermediate vision without negatively impacting distance or near VA when compared to a bifocal toric IOL. LCVA and the patient’s visual functions were comparable between the trifocal and bifocal toric IOL groups. The trifocal toric lens demonstrated good rotation stability, leaving subjects with low postoperative refractive astigmatism.
Acknowledgment
The study was funded with a grant from FineVision, Liège, Belgium. Sarah Y Makari, OD is a consultant to Science in Vision who received compensation for writing assistance in the preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Hayashi K, Manabe S, Yoshida M, Hayashi H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2010;36(8):1323–1329. | ||
Khan MI, Muhtaseb M. Prevalence of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom. J Cataract Refract Surg. 2011;37(10):1751–1755. | ||
Mingo-Botín D, Muñoz-Negrete FJ, Won Kim HR, Morcillo-Laiz R, Rebolleda G, Oblanca N. Comparison of toric intraocular lenses and peripheral corneal relaxing incisions to treat astigmatism during cataract surgery. J Cataract Refract Surg. 2010;36(10):1700–1708. | ||
Gangwani V, Hirnschall N, Findl O, Maurino V. Multifocal toric intraocular lenses versus multifocal intraocular lenses combined with peripheral corneal relaxing incisions to correct moderate astigmatism. J Cataract Refract Surg. 2014;40(10):1625–1632. | ||
Pepose JS, Hayashida J, Hovanesian J, et al. Safety and effectiveness of a new toric presbyopia-correcting posterior chamber silicone intraocular lens. J Cataract Refract Surg. 2015;41(2):295–305. | ||
Hayashi K, Masumoto M, Takimoto M. Comparison of visual and refractive outcomes after bilateral implantation of toric intraocular lenses with or without a multifocal component. J Cataract Refract Surg. 2015;41(1):73–83. | ||
Alfonso JF, Knorz M, Fernandez-Vega L, et al. Clinical outcomes after bilateral implantation of an apodized +3.0 D toric diffractive multifocal intraocular lens. J Cataract Refract Surg. 2014;40(1):51–59. | ||
Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013;39(7):1093–1099. | ||
Cochener B, Vryghem J, Rozot P, et al. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 2012;6:1421–1427. | ||
Carson D, Hill WE, Hong X, Karakelle M. Optical bench performance of AcrySof(®) IQ ReSTOR(®), AT LISA(®) tri, and FineVision(®) intraocular lenses. Clin Ophthalmol. 2014;8:2105–2113. | ||
Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011;37(11):2060–2067. | ||
Vryghem JC, Heireman S. Visual performance after the implantation of a new trifocal intraocular lens. Clin Ophthalmol. 2013;7:1957–1965. | ||
Cochener B, Vryghem J, Rozot P, et al. Clinical outcomes with a trifocal intraocular lens: a multicenter study. J Refract Surg. 2014;30(11):762–768. | ||
Chassain C. Évaluation des performances visuelles après implantation d’une lentille intraoculaire torique à double anse en C [Evaluation of visual performance after implantation of a double C-Loop toric intraocular lens]. J Fr Ophtalmol. 2014;37(7):507–513. [French]. | ||
Bozukova D, Werner L, Mamalis N, et al. Double-C loop platform in combination with hydrophobic and hydrophilic acrylic intraocular lens materials. J Cataract Refract Surg. 2015;41(7):1490–1502. | ||
Mangione CM, Lee PP, Gutierrez PR, et al; National Eye Institute Visual Function Questionnaire Field Test Investigators. Development of the 25-item national eye institute visual function questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
