Back to Journals » Neuropsychiatric Disease and Treatment » Volume 10
Comparison of three screening tests for autism in preterm children with birth weights less than 1,500 grams
Authors Dudova I, Markova D, Kasparova M, Zemankova J, Beranova S, Urbanek T, Hrdlicka M
Received 19 August 2014
Accepted for publication 15 September 2014
Published 17 November 2014 Volume 2014:10 Pages 2201—2208
DOI https://doi.org/10.2147/NDT.S72921
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Iva Dudova,1 Daniela Markova,2 Martina Kasparova,3 Jana Zemankova,4 Stepanka Beranova,1 Tomas Urbanek,5 Michal Hrdlicka1
1Department of Child Psychiatry, Charles University Second Faculty of Medicine and University Hospital Motol, Prague, Czech Republic; 2Department of Pediatrics and Adolescent Medicine, Charles University First Faculty of Medicine and General University Hospital, Prague, Czech Republic; 3Department of Pediatrics, Charles University Second Faculty of Medicine and University Hospital Motol, Prague, Czech Republic; 4Department of Pediatrics, Charles University Faculty of Medicine and University Hospital, Hradec Kralove, Czech Republic; 5Institute of Psychology, Academy of Sciences, Brno, Czech Republic
Background: Preterm children seem to be at increased risk for autism spectrum disorders (ASD).
Methods: Parents of 157 children with birth weights less than 1,500 g (age 2 years, corrected for prematurity; 88 boys, 69 girls) completed screening questionnaires. The screening battery included the Modified Checklist for Autism in Toddlers (M-CHAT), Communication and Symbolic Behavior Scales Developmental Profile Infant-Toddler Checklist (CSBS-DP-ITC), and the Infant/Toddler Sensory Profile (ITSP). Children with disabilities were excluded. All children who screened positive on any of the screening tools were subsequently assessed by clinical examination including the Autism Diagnostic Observation Schedule.
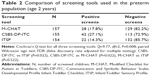
Results: Fifty-six children (35.7%) screened positive on at least one of the parental screening questionnaires. Of the 56 children who tested positive, 33 participated in the detailed clinical follow-up assessment. A diagnosis of ASD was confirmed in 13 of the 33 children. The ASD prevalence was 9.7% of the sample. Analysis of children with and without an ASD diagnosis found significant differences relative to gestational age (26.9 weeks vs 28.3 weeks, P=0.033) and length of the stay in hospital (89.5 days vs 75.4 days, P=0.042). The screening tool with the most positive results was CSBS-DP-ITC (42 positive screens [PS]), followed by M-CHAT (28 PS), and ITSP (22 PS). Differences in the frequency of PS among the tests were significant (P=0.008). CSBS-DP-ITC had the highest sensitivity (0.846), followed by M-CHAT (0.692) and ITSP (0.462).
Conclusion: Our results indicate a higher prevalence of autism in children with birth weights <1,500 g at 2 years of age compared to the general population prevalence. The ASD diagnosis was associated with shorter gestation times and longer hospital stays. Our findings support the simultaneous use of more than one screening tests in order to increase screening sensitivity.
Keywords: autism spectrum disorders, preterm children, screening, Modified Checklist for Autism in Toddlers, Communication and Symbolic Behavior Scales Developmental Profile Infant-Toddler Checklist, Infant/Toddler Sensory Profile
Introduction
There is a growing body of evidence that preterm children with very low birth weight (VLBW; 1,000–1,500 g) or extremely low birth weight (ELBW; under 1,000 g) are at increased risk for autism spectrum disorders (ASD). Recent studies on this topic, in which screening results were validated with clinical examinations and/or diagnostic instruments, have described the prevalence of ASD among preterm births to be in the range 3.65%–12.9%,1–4 whereas the ASD prevalence in the general pediatric population has been found to be in the range 1%–1.5%.5,6
The autistic phenotype seen in preterm children is thought to represent a milder form of the disorder than that seen in full-term children.7 Moreover, extremely preterm children have greater symptoms on the dimension of impaired social interaction and communication than on the dimension of repetitive or stereotyped behavior, the latter of which is a core symptom domain in diagnostic classifications.8 Studies performed on school-age children who were born preterm have revealed a markedly lower prevalence of ASD than would have been expected from the positive screen rate during infancy.8 The change in the expected prevalence may suggest that this population has the potential to “recover from autism”.
ASD have generally been regarded as life-long conditions.9 However, in recent years a significant minority of children with well-documented ASD have achieved recovery from the disorder (terms “best outcome” and “optimal outcome” have also been used).10–12 In a comprehensive review, Helt et al10 found that 3%–25% of children reportedly “lost” their ASD diagnosis and attained a normal range of cognitive, adaptive, and social skills. However, we do not yet have any specific data on recovery from autism in preterm children.13
The differences between preterm ASD and genuine ASD in the autism phenotype and/or prognosis may arise from a different causal pathway, ie, one that is nongenetic and stems from brain injuries and altered neurodevelopment associated with a very premature birth.14 Some authors have found a direct relationship between shorter gestation times and increased risk of ASD. Losh et al15 in a same-sex twin study estimated that every 100 g increase in birth weight provided a 13% reduction in the risk of ASD. Kuzniewicz et al16 found that ASD was approximately three times more prevalent in infants born before 27 weeks of gestation compared with term infants and that each 1-week reduction in gestation was associated with further increases in the risk of ASD. Leavey et al17 also observed a gradual increase in ASD risk linked to shorter gestation times, which was especially apparent for cutoffs between 29 weeks and 37 weeks. The results were not affected by sex or measures of fetal growth. Buchmayer et al18 observed a different relationship. They found that the increased risk of ASD related to preterm birth was mediated not by the gestation weeks but primarily by prenatal and neonatal complications, which occur more commonly among preterm infants. However, the largest study on the topic, performed by Mackay et al19 did not identify any significant association between ASD risk and obstetric factors.
Other authors have emphasized the role of fetal growth on the risk of ASD. Moore et al20 reported that autism risk was increased in preterm small-for-gestational age (SGA; <5th percentile) infants 23–33 weeks and term large-for-gestational age (LGA; >95th percentile) 39–41 weeks, but decreased in preterm LGA infants 23–31 weeks. In a study by Abel et al21 ASD risk was seen to increase with fetal growth 1.50 standard deviations below and >2.00 standard deviations above the mean gestational age.
There were three aims of our study: 1) to estimate ASD prevalence in preterm children aged 2 years (corrected for prematurity); 2) to identify potential association of ASD diagnosis in preterm children with specific demographic and medical factors, such as parental age at delivery and education, child’s birth weight and length, gestational age at delivery, length of the stay in hospital, and the use of corticoids; and 3) to compare the efficacy of three different screening tests in this population. The preliminary results have already been published,4 and now we present final data from our study.
Methods
Sample
Children with birth weights less than 1,500 g were consecutively recruited from March 2012 to June 2014. Three centers for “Newborns and Infants at Risk” participated in the study: the Department of Pediatrics, University Hospital Motol, Prague; the Department of Pediatrics and Adolescent Medicine, General University Hospital, Prague; and the Department of Pediatrics, University Hospital, Hradec Kralove. Families were informed about the research project during routinely scheduled checkups for 2-year-old children (age corrected for prematurity). The 2-year (age-corrected) checkup is usually the last examination and assessment of preterm children in specialized centers for “Newborns and Infants at Risk” and further care is then decentralized to pediatricians along with the switch from corrected age to chronological age. Children with substantial disabilities, such as cerebral palsy or major vision and/or hearing impairments, were excluded.
Parents of 247 children with birth weights less than 1,500 g agreed to participate in the study and signed informed consents. Of these, families of 157 children (63.6%) completed the screening questionnaires and returned them to the Department of Child Psychiatry. The sample consisted of 88 boys and 69 girls, aged 2 years (corrected for prematurity).
ASD screening tools
The screening battery included the Modified Checklist for Autism in Toddlers (M-CHAT),22 the Communication and Symbolic Behavior Scales Developmental Profile Infant-Toddler Checklist (CSBS-DP-ITC),23 and the Infant/Toddler Sensory Profile (ITSP).24 General descriptions and detailed information of the psychometric properties of these tests are given in our previous report.4
In those with positive M-CHAT screens, follow-up interviews, consisting of additional corresponding questions, are recommended. In our study, we used a follow-up clinical evaluation instead of the recommended telephone interview; however, we think this substitution improved the accuracy of our results.
ITSP was not originally considered a screening tool, and this study is probably the first to evaluate its use as a screening tool. Although our initial results did not seem to overly promising,4 we decided to retain ITSP in the battery in order to make a final analysis.
Procedure
The study was approved by the Ethics Committees of all three participating hospitals. Parents of VLBW and ELBW children (2 years of age, corrected for prematurity) who agreed to participate in the study signed informed consents and received test materials with written instructions on how to fill out the questionnaires. No recommendations regarding the order of test completion were given. Parents completed the screening battery of questionnaires at home and returned them by regular mail to the Department of Child Psychiatry, Motol University Hospital.
All children who had screened positive on any of the screening tools were subsequently invited for a detailed follow-up assessment. The assessment involved testing using the Autism Diagnostic Observation Schedule (ADOS)25 and a clinical examination by two experienced child psychiatrists with expertise in autism. The concept of best estimate clinical diagnosis (BECD), by consensus of two experienced specialists, was used as the gold standard.26 In cases of disagreement between the ADOS diagnosis and BECD, the latter was preferred. The International Classification of Diseases, Tenth Edition (ICD-10), was used for clinical diagnoses.27
Data analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (IBM SPSS, version 22.0) and statistical software R28 with the RVAideMemoire29 and pROC libraries.30 Descriptive statistics for the samples were used. The Mann–Whitney U-test and χ2-test were used for analyzing the differences between subgroups with and without an ASD diagnosis. Cochran’s Q-test was used for analyzing differences in positivity among tests. More detailed pair comparisons between tests were performed using the paired Wilcoxon sign tests, with the false discovery rate adjusted for multiple testing. Receiver operating characteristic (ROC) analysis was used in the evaluation of the three screening tests.
Results
ASD prevalence in the sample
Fifty-six children (35.7%) screened positive on at least one of the screening questionnaires. Parents of 33 of the 56 children agreed to participate in the follow-up assessment. A diagnosis of ASD was indicated in 15 children based on the ADOS, and ASD was ultimately confirmed in 13 of the 33 children. Diagnoses, based on the ICD-10, were childhood autism (n=7) and atypical autism (n=6). In two cases (2 of 15), there was a disagreement between the ADOS diagnosis and the BECD. In the first case, ADOS indicated ASD but the BECD was that of mild mental retardation. In second case, ADOS indicated ASD; however, no psychiatric diagnosis (BECD) was established. ASD prevalence calculated from those examined (33 children) and those with negative screening results (101 children) was estimated to be as high as 9.7% of the sample.
Demographic and medical factors
Table 1 shows the family and child characteristics for the total sample and for the subgroups. Based on the final diagnosis, two subgroups were formed. The subgroup with an ASD diagnosis (N=13) consisted of children who screened positive and when subsequently examined (ADOS and BECD) fell into the category of ASD. The other subgroup was without an ASD diagnosis (N=121) and consisted of 101 children who initially screened negative on all three screening tests as well as 20 children who initially screened positive; however, after subsequent examination, BECD failed to confirm a diagnosis of ASD. Children who were positive on at least one screening test but whose parents did not agree with the clinical examination (N=23) were not included in the subgroup analysis.
  | Table 1 Family and child characteristics of the preterm population (age 2 years) |
A comparison of children with and without an ASD diagnosis showed significant differences relative to gestational age (P=0.033) and length of the stay in hospital (P=0.042) between the two subgroups (Table 1). We found no significant differences relative to maternal and paternal age at delivery, level of maternal and paternal education, mean birth weight and length, or the use of corticoids.
Screening battery
The screening tool with the most positive results was CSBS-DP-ITC (42 positive screens). M-CHAT had 28 positive screens and ITSP had 22 positive screens. For details, see Table 2. The difference in positive results among the screening tests was significant (P=0.008). In pair comparisons, using the paired Wilcoxon sign tests with the false discovery rate adjusted for multiple testing, CSBS-DP-ITC was found to be significantly more positive than both ITSP (P=0.022) and M-CHAT (P=0.022). The difference between M-CHAT and ITSP was not significant.
ROC analysis was calculated from a sample of 134 children which consisted of the subgroup with an ASD diagnosis (N=13) and the subgroup without an ASD diagnosis (N=121); for a more detailed description of both subgroups see the “Demographic and medical factors” section. Table 3 summarizes the results of the ROC analyses of individual tests in relation to the ASD diagnosis. CSBS-DP-ITC turned out to be the most sensitive tool; similarly, M-CHAT and ITSP also showed high levels of specificity and accuracy. Additionally, the negative predictive value was high for all three screening questionnaires; however, the positive predictive value (PPV) tended to be relatively low for all three tests. The second half of Table 3 displays the psychometric values derived from the combined use of the three screening tests. The first line in Table 3 shows results for the combined use, which is how it was used in our study (ie, if one of the tests was positive, then the screen was considered positive). The next two lines demonstrate how psychometric values would change relative to changes in the “screen positive” criteria (ie, if 2 of 3, or 3 of 3 tests must be positive for the screen to be positive).
Discussion
Our study estimated the prevalence of ASD to be as high as 9.7%, a number that was lower than in our preliminary data (12.9%). The ASD prevalence might have been slightly higher if all the children with positive screens had undergone the clinical examination. Unfortunately, parents of a large proportion of children (41.1%) who screened positive did not bring their children in for the follow-up examination. Our estimated ASD prevalence in preterms was several times higher than in general population, which was in agreement with previous findings from studies that validated the screening results with clinical examinations.1–3 Moreover, our sample of VLBW and ELBW children allowed us to establish an increased frequency of ASD at the age of 2 years, whereas the studies cited above examined either school-age children1,2 or adolescents and those in early adulthood.3
Some may argue that certain developmental trajectories in preterm children are at variance with those in term children. Children with a “preterm behavioral phenotype” may present with symptoms that resemble, overlap, or even meet the criteria for ASD diagnosis. Thus, more prospective studies with comparison groups of term children are needed in order to identify precisely the optimal ASD screening age for preterm children.13 We think that early identification of autism in preterms (eg, at 2 years of corrected age, as it was in our study) and prospective follow-up of this group will provide valuable information on the stability of the diagnosis with time and on possible rates of “recovery from autism” in this specific group. Such a study is one of our long-term research aims.
Many previous studies have examined the association between gestational age and ASD, and some of them observed an increased association with autism in preterm children as well as post-term children. Studies by Kuzniewicz et al16 and Leavey et al17 found a higher prevalence of ASD associated with shorter gestational periods. In accordance with these results, we also observed an association between shorter gestational age and an increased occurrence of ASD. An association between birth weight and ASD frequency has also been reported in a large population-based study.15 Our study also found a difference in birth weight between children with and without ASD; however, it was not statistically significant.
In a study by Buchmayer et al18 the increased risk of autistic disorders related to preterm birth was mediated primarily by prenatal and neonatal complications, which occurred more commonly among preterm infants. Kuzniewicz et al16 retrospectively evaluated changes in ASD risks relative to changes in gestational age. Additionally, the study sought to correlate specific gestational age-related neonatal risk factors (ie, conditions and interventions) with changes in the prevalence of ASD. The study found that high-frequency ventilation and intracranial hemorrhage were associated with ASD in infants with gestation ages <34 weeks. Our study found an association between ASD and length of hospital stay, which indicated an association between ASD and neonatal risk factors. In a population-based cohort study by Moore et al20 the authors found many factors associated with ASD, eg, male sex, advanced maternal and paternal age, and twin gestation. In our study, we found no significant differences relative to maternal and paternal age at delivery or level of maternal and paternal education; however, this could easily be a reflection of a small sample size.
Our study may be the first to compare the efficacy of three well-established tests for use with preterms (M-CHAT and CSBS-DP-ITC have been well established in screening; the use of ITSP for screening was experimental but the test itself has been reliably studied). M-CHAT is the most frequently used parental screening test for autism. Authors of the test have demonstrated its high sensitivity (0.87) and specificity (0.99).22 Kleinman et al31 found a PPV of 0.36 for the initial screening which improved to 0.74 when combined with a follow-up interview. We used the screening questionnaire without a follow-up interview and found the sensitivity lower (0.69) than in Robins et al’s study,22 although the specificity was almost as high (0.93). The PPV, which tends to be low when the screening questionnaire is used without a follow-up interview, was higher in our results (0.5) than in Kleinman et al’s study.31 In previous studies, 21%–41% of extremely preterm infants screened positive on M-CHAT; however, after excluding children with disabilities, the number of positive screens decreased to 10%–16.5%.32,33 Our study also excluded children with major disabilities, and 17.5% of our sample screened positive, a result comparable to previous studies.
CSBS-DP-ITC is a general broadband screen that detects a wide range of disorders such as global developmental delay, general language delay, and autism. Sensitivity estimates ranged from 0.87 to 0.93, and specificity was found to be 0.75.23 In our study, the sensitivity was comparable to the estimated range (0.85), while the specificity was higher (0.85) than in Wetherby et al’s report.23 The sensitivity of CSBS-DP-ITC test was the highest of the three screening tools used in our study (Table 3). The number of positive responses was high (27.1%). PPV specific to an ASD diagnosis was low in our study (0.38) compared to the PPV presented in Pierce et al’s report34 which used CSBS-DP-ITC for the detection of a wide range of disorders connected to global developmental impairment (PPV =0.75).
ITSP is a norm-referenced questionnaire, in which the caregiver rates the frequency at which the individual being tested engages in the described response to sensory input.24 In extensive meta-analysis of sensory modulation symptoms in persons with ASD, different versions of the sensory profile, including ITSP, were found to be the most frequently used methods for measuring sensory processing.35 Unlike M-CHAT and CSBS-DP-ITC, ITSP is not generally used for screening;36 however, early on we concluded that ITSP might be a useful screening tool because autistic children often display unusual behavioral responses to sensory input, such as hypersensitivity to auditory, visual, tactile, and olfactory stimuli.37,38 Our study may be the first to evaluate its use as a screening tool. We also established a new criterion for a positive screening. The criterion was that participants were considered to have screened positive if the results were definitely abnormal (ie, results outside two standard deviations of population norms) on at least two scores involving section and/or quadrant scores.4 ITSP had the lowest number of positive responses (14.3%). With regard to the lowest number of positive responses in comparison to the other two questionnaires, it seems that the established criteria might have been too strict. Test accuracy, with regard to ASD diagnosis, was high (0.90), and so was its specificity (0.94); both parameters were comparable to those of M-CHAT (Table 3). As with the other two tests, the negative predictive value was high (0.94) and the PPV was low (0.46). However, of the three tests, ITSP turned out to be the least sensitive (0.46) and this handicaps its use for general screening.
To conclude this part of the discussion, M-CHAT and CSBS-DP-ITC showed good psychometric properties for screening a preterm population. CSBS-DP-ITC had the highest sensitivity of the three tests we used, which could be outweighed by faster and easier administration of M-CHAT. Therefore, the selection of an appropriate screening test for clinical purposes should be based not only on psychometric properties of the tests but also on specific aims and broader circumstances of each screening.
To our knowledge, our results can only be compared to the 2012 study by Stephens et al39 who also used a screening battery instead of a single tool. They found a markedly smaller percentage of positive screens, with only 20% of infants (excluding those with disabilities) having at least one positive screen, whereas in our study it was 35.7% of children. Stephens et al reported that only 1% of the sample screened positive on all three screens, whereas our study found that 9% of participants were positive on all three screens. It must be noted that Stephens et al used less common screening instruments such as the Pervasive Developmental Disorder Screening Test, Second Edition Stage 2, and two parts from the ADOS (ie, response to name and response to joint attention). Despite using different screening tools, they reached the same conclusion as we did: that is, simultaneous use of more than one screening test results in a higher number of positive screens, which means better screening sensitivity.
The most noteworthy limitation of our study was the large number of children with positive screens who did not undergo clinical evaluation because of their parent’s lack of interest (23 from 56 or 41.1%). Additionally, we did not clinically examine the children who had negative screening results; therefore we were not able to make a valid differentiation between true and false negatives in our ROC analyses. However, we can model this differentiation using an analysis of the combined use of the three tests, because there were children who were negative on one screening test and positive on one or both of the other screening test(s) (Table 3). The assessment of the combined tests are done using three steps, each using a different criterion for a “positive screen” (positive on at least one test, on at least two tests, on all three tests), shows us, despite the first step where the sensitivity and NPV are unrealistically high (this is direct logical consequence of the lack of false negatives in our sample), that there is a potential for substantial improvement of ROC values (sensitivity, specificity, PPV, and NPV) when using a combination of screening tests. However, taking into account the second limitation, the psychometric values given in Table 3 are much stronger for mutual comparisons among the listed screening tests than for use as independent values.
Another issue, which was stated in the publication of our preliminary results,4 was that we relied solely on the clinical judgment of pediatricians and child neurologists regarding disabilities. This reliance could have affected the number of children excluded for major disabilities. Finally, there was no structured examination of motor and cognitive functions in our sample of children, which can be analyzed and presented.
Conclusion
Our results indicate a higher prevalence of autism in children with birth weights <1,500 g at 2 years of age compared to the prevalence in the general population. We found that the ASD diagnosis was associated with shorter gestational age and longer hospital stays. Our findings support the simultaneous use of more than one screening test in order to increase screening sensitivity.
Acknowledgments
This work was supported by the Ministry of Education, Youth and Sports, Czech Republic (research grant COST LD11028), by the Ministry of Health, Czech Republic (research grant IGA NT/14200 and conceptual development of research organization, University Hospital Motol, Prague, Czech Republic 00064203), and by the ESF (COST Action ESSEA BM1004). The authors would like to thank Thomas Secrest for his assistance with the English version of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Hack M, Taylor HG, Schluchter M, Andreias L, Drotar D, Klein N. Behavioral outcomes of extremely low birth weight children at age 8 years. J Dev Behav Pediatr. 2009;30:122–130. | ||
Johnson S, Hollis C, Kochhar P, Hennessy E, Wolke D, Marlow N. Autism spectrum disorders in extremely preterm children. J Pediatr. 2010;156:525–531. | ||
Pinto-Martin JA, Levy SE, Feldman JF, Lorenz JM, Paneth N, Whitaker AH. Prevalence of autism spectrum disorders in adolescents born weighing <2,000 grams. Pediatrics. 2011;128:883–891. | ||
Dudova I, Kasparova M, Markova D, et al. Screening for autism in preterm children with extremely low and very low birth weight. Neuropsychiatr Dis Treat. 2014;10:277–282. | ||
Baron-Cohen S, Scott FJ, Allison C, et al. Prevalence of autism-spectrum conditions: UK school-based population study. Br J Psychiatry. 2009;194:500–509. | ||
Baio J. Prevalence of autism spectrum disorders among children aged 8 years – Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2010. MMWR Surveill Summ. 2014;63(2):1–21. | ||
Indredavik MS, Vik T, Skranes J, Brubakk AM. Positive screening results for autism in ex-preterm infants. Pediatrics. 2008;122:222–223. | ||
Johnson S, Marlow N. Growing up after extremely preterm birth: lifespan mental health outcomes. Semin Fetal Neonatal Med. 2014;19:97–104. | ||
Amaral DG, Dawson G, Geschwind DH, editors. Autism Spectrum Disorders. New York: Oxford University Press; 2011. | ||
Helt M, Kelley E, Kinsbourne M, et al. Can children with autism recover? If so, how? Neuropsychol Rev. 2008;18:339–366. | ||
Kamio Y, Tobimatsu S, Fukui H. Developmental disorders. In: Decety J, Cacioppo JT, editors. The Oxford Handbook of Social Neuroscience. New York: Oxford University Press; 2011:848–858. | ||
Hrdlicka M, Dudova I. Controversies in autism: is a broader model of social disorders needed? Child Adolesc Psychiatry Ment Health. 2013;7:9. | ||
Yarri M, Eventov-Freidman S, Mankuta D, Bar-Oz B, Yirmiya N. Prematurity and autism spectrum disorders. In: Patel VB, Preedy VR, Martin CR, editors. Comprehensive Guide to Autism. New York: Springer; 2014:1371–1387. | ||
Williamson KE, Jakobson LS. Social perception in children born at very low birthweight and its relationship with social/behavioral outcomes. J Child Psychol Psychiatry. 2014;55:990–998. | ||
Losh M, Esserman D, Anckarsater H, Sullivan PF, Lichtenstein P. Lower birth weight indicates higher risk of autistic traits in discordant twin pairs. Psychol Med. 2012;42:1091–1102. | ||
Kuzniewicz MW, Wi S, Qian Y, Walsh EM, Armstrong MA, Croen LA. Prevalence and neonatal factors associated with autism spectrum disorders in preterm infants. J Pediatr. 2014;164:20–25. | ||
Leavey A, Zwaigenbaum L, Heavner K, Burstyn I. Gestational age at birth and risk of autism spectrum disorders in Alberta, Canada. J Pediatr. 2013;162:361–368. | ||
Buchmayer S, Johansson S, Johansson A, Hultman CM, Sparen P, Cnattingius S. Can association between preterm birth and autism be explained by maternal or neonatal morbidity? Pediatrics. 2009;124:e817–e825. | ||
Mackay DF, Smith GCS, Dobbie R, Cooper SA, Pell JP. Obstetric factors and different causes of special educational need: retrospective cohort study of 407 503 schoolchildren. BJOG. 2013;120:297–308. | ||
Moore GS, Kneitel AW, Walker CK, Gilbertz WM, Xing G. Autism risk in small- and large-for-gestational-age infants. Am J Obstet Gynecol. 2012;206:314.e1–314.e9. | ||
Abel KM, Dalman C, Svensson AC, et al. Deviance in fetal growth and risk of autism spectrum disorder. Am J Psychiatry. 2013;170:391–398. | ||
Robins DL, Fein D, Barton ML, Green A. The modified checklist for autism in toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord. 2001;31:131–144. | ||
Wetherby AM, Brosnan-Maddox S, Peace V, Newton L. Validation of the infant-toddler checklist as a broadband screener for autism spectrum disorders from 9 to 24 months of age. Autism. 2008;12:487–511. | ||
Dunn W. Infant/Toddler Sensory Profile. User’s Manual. San Antonio, TX: The Psychological Corporation; 2002. | ||
Lord C, Risi S, Lambrecht L, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–223. | ||
Kim SH, Lord C. Combining information from multiple sources for the diagnosis of autism spectrum disorders for toddlers and young preschoolers from 12 to 47 months of age. J Child Psychol Psychiatry. 2012;53:143–151. | ||
World Health Organization. International Classification of Diseases. 10th ed. Geneva: WHO; 1992. | ||
R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. Available from: http://www.R-project.org/ | ||
Hervé M. RVAideMemoire: Diverse Basic Statistical and Graphical Functions. R Package Version 0.9-27; 2013. Available from: http://CRAN.Rproject.org/package=RVAideMemoire | ||
Robin X, Turck N, Hainard A, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011;12:77. | ||
Kleinman JM, Robins DL, Ventola PE, et al. The modified checklist for autism in toddlers: a follow-up study investigating the early detection of autism spectrum disorders. J Autism Dev Disord. 2008;38:827–839. | ||
Kuban KC, O’Shea M, Allred EN, Tager-Flusberg H, Goldstein DJ, Leviton A. Positive screening of the Modified Checklist for Autism in Toddlers (M-CHAT) in extremely low gestational age newborns. J Pediatr. 2009;154:535–540. | ||
Moore T, Johnson S, Hennessy E, Marlow N. Screening for autism in extremely preterm infants: problems in interpretation. Dev Med Child Neurol. 2012;54:514–520. | ||
Pierce K, Carter C, Weinfeld M, et al. Detecting, studying, and treating autism early: the one-year well-baby check-up approach. J Pediatr. 2011;159:458–465. | ||
Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, Gal E. A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. J Autism Dev Disord. 2009;39:1–11. | ||
Eeles AL, Spittle AJ, Anderson PJ, et al. Assessment of sensory processing in infants: a systematic review. Dev Med Child Neurol. 2013;55:314–326. | ||
Wiggins LD, Robins DL, Bakeman R, Adamson LB. Brief report: sensory abnormalities as distinguishing symptoms of autism spectrum disorders in young children. J Autism Dev Disord. 2009;39:1087–1091. | ||
Hrdlicka M, Vodicka J, Havlovicova M, Urbanek T, Blatny M, Dudova I. Brief report: significant differences in perceived odor pleasantness found in children with ASD. J Autism Dev Disord. 2011;41:524–527. | ||
Stephens BE, Bann CM, Watson VE, et al. Screening for autism spectrum disorders in extremely preterm infants. J Dev Behav Pediatr. 2012;33:535–541. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.