Back to Journals » Clinical Optometry » Volume 14
Comparison of the Pre-Lens Tear Film Stability and Visual Performance of a Novel and Two Other Daily Disposable Contact Lenses in Healthcare Professionals Wearing Facial Masks for Prolonged Time
Authors Penbe A , Kanar HS, Donmez Gun R
Received 29 July 2022
Accepted for publication 19 September 2022
Published 10 October 2022 Volume 2022:14 Pages 183—192
DOI https://doi.org/10.2147/OPTO.S384246
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Aysegul Penbe, Hatice Selen Kanar, Raziye Donmez Gun
Department of Ophthalmology, Health Science University, Kartal Dr. Lutfi Kirdar Training and Research Hospital, Istanbul, Turkey
Correspondence: Aysegul Penbe, Department of Ophthalmology, Health Science University, Kartal Dr. Lutfi Kirdar Training and Research Hospital, Semsi Denizer Caddesi, E-5, 34890 Kartal, Istanbul, Turkey, Tel +905442910757, Email [email protected]
Objective: To compare a novel daily disposable contact lens (DDCL) verofilcon A with other DDCL materials in terms of pre-lens tear film (PLTF) stabilization and visual performance for prolonged use in healthcare professionals with the use of masks.
Methods: Subjects aged 20– 40 years old were prospectively randomized into three study groups. Group 1: verofilcon A, group 2: nesofilcon A and group 3: senofilcon A. The subjects were evaluated at baseline with best corrected visual acuity (BCVA), non-invasive tear break up time (NIBUT) of pre-lens tear film, and high order aberrations (HoAs). After 28 days of CL use, NIBUT at 1, 4, 8, and 12 h, HoAs, contrast sensitivity (CS) with CVS100-E and contact lens dry eye questionnaire-8 (CLDEQ-8) were evaluated.
Results: Between August and September 2021, 147 eyes of 77 subjects were included in the three study groups. At day 28, the CS scores at 18 cycles per degree, spatial frequencies, and the mean NIBUT scores at 4, 8, and 12 h were higher in the verofilcon A group compared to the nesofilcon A and at 12 h were higher compared to the senofilcon A (p < 0.05). The mean HoAs and CLDEQ-8 test scores were higher in the nesofilcon A group (p < 0.001).
Conclusion: The results of this study suggest the superiority of the PLTF stabilization ability of verofilcon A in healthcare professionals with prolonged use of mask. The improved CS and NIBUT scores of this lens could be explained by a new and unique surface technology with greater than 80% water content.
Keywords: facial mask, HoAs, nesofilcon A, NIBUT, senofilcon A, verofilcon A
Introduction
In the current coronavirus 2019 (COVID-19) pandemic, the widespread use of face masks, which is essential for the prevention of novel virus transmission, may cause ocular dryness and irritation.1 During facial mask use, tear film instability occurs as a result of the upwardly directed breathing reaching the ocular surface.2
The use of facial masks has become closely related to visual quality of life regarding refractive correction methods in addition to eye dryness symptoms. Complaints of sweating and fogged glasses with contamination risks have been associated with the use of masks.3 To avoid visual disturbance, preferring to use contact lenses (CLs) instead of glasses has become a good option for healthcare professionals who wear masks for extended periods. Although habitual contact lens (CL) wearers reported wearing CLs less than usual, there is an increase in the frequency of visiting CL practitioners to switch glasses to CLs among health care professionals.4
CLs can have biophysical interactions with the tear film and can result in biochemical changes in the tear film.5 When CLs are placed on the ocular surface, they cause the tear film to split into two parts: the pre-lens tear film (PLTF) and post-lens tear film.6 Although evaluating the noninvasive breakup time (NIBUT) of the PLTF gives limited information regarding the pre-lens tear film stability, it could be a useful indicator of tear film dysfunction in symptomatic contact lens users.7
Over the past two years, 35% of CL wearers have reduced or paused their CL wear since early 2020 owing to the covid-19 pandemic because of the CL-related discomfort or occasion problems.8 The appropriate CL wearing modalities during the use of facial masks should be disposable daily instead of reusable CLs to minimize contamination risks and solution-related complications. The selected CL should have high water content and low dehydration rate with high oxygen transmissibility to avoid worsening dry eye symptoms and to eliminate the discontinuation of lens wear in prolonged use.4
Verofilcon A (Precision1™, Alcon Laboratories Inc., Fort Worth, TX, USA) is a silicone hydrogel (SiHy) daily disposable contact lens (DDCL) made from a new material using Smartsurface™ technology is a lubricious 2–3 µm ultra-soft surface gel that steps up from 51% water at the core to greater than 80% water at the outer surface.9 Changes in the CL hydration or changes in the quality of the PLTF may result in alterations in visual performance.10 These lenses support optically precise PLTF with enhanced comfort levels. Senofilcon A (Acuvue Oasys™ 1- Day; Johnson & Johnson Vision Care, Inc., Jacksonville, FL, USA) is a well-known SiHy DDCL offering high comfort levels with HydraLuxe™ technology that is mucin-like internal wetting agent polyvinylpyrrolidone working with the natural mucins of the tear film.11 Nesofilcon A (Biotrue ONEday™, Bausch & Lomb, Rochester, New York, USA) is a widely used, high-quality, and well-accepted conventional hydrogel (Hy) DDCL material with 78% water content throughout and a surface that retains water, like the natural tear film of the polymer-bound surface active macromer poloxamer 407.12
To identify the most appropriate DDCL material in terms of tear film stabilization, ocular comfort levels, and visual quality for prolonged use, we compared the novel SiHy DDCL of Verofilcon A with another SiHy DDCL of Senofilcon A and a Hy DDCL of nesofilcon A.
Methods
Study Design
This was a prospective randomized comparative clinical study. The subjects were enrolled in the study at the contact lens department of Dr Lutfu Kirdar Training and Research Hospital between August and September 2021. The study protocol adhered to the tenets of the Declaration of Helsinki for clinical research and was approved by the Ethical Committee of the Kartal Dr Lutfu Kirdar Training and Research Hospital. Written informed consent was obtained from all subjects after explaining the purpose and possible consequences of the study.
Patient Recruitment
Healthcare professionals aged between 20 and 40 and wearing a surgical mask at least 8 hours/day and five days in a week were conducted the study. Subjects who had no history of CLs before and were able to wear CLs for more than 12 hours (h) per day, randomized into three study groups. The recommended DDCLs for group 1 were verofilcon A, for group 2 was senofilcon A, and for group 3 was nesofilcon A. Technical details of the DDCLs of the study groups are listed in Table 1.
 |
Table 1 The Parameters of the DDCLs of the Study Groups |
Subjects with refractive errors between +4.00 Diopters (D) and −8.00 D needed no or minimal (<0.75 D) cylindric refractive corrections, and best corrected visual acuity (BCVA) of 20/25 or better was recruited. Detailed anterior and posterior segment examinations with Oxford corneal staining scores and the Schirmer test were performed to exclude ocular surface disorders at baseline.
Subjects with severe dry eye disease, findings of NIBUT ≤ 5 seconds, Oxford corneal staining ≥ scale 3, and <5 mm/5 min Schirmer test scores were excluded from the study. The other exclusion criteria were BCVA <20/25, manifest astigmatism ≥0.75, diopter, ocular allergy findings (papillary conjunctivitis), corneal vascularization, current or history of herpetic keratitis, meibomian gland dysfunction, pregnancy, retinal problems or glaucoma, pseudophakia or cataract, history of ocular surgery, and any systemic or ocular medical treatment including artificial tear drops.
Endpoints
The primary endpoint was tear film stability via NIBUT measurements over time with prolonged use of contact lenses. NIBUT scores were evaluated at baseline and at 1, 4, 8, and 12 h of lens wearing on day 28. Secondary endpoints included anterior corneal wavefront analysis, contrast sensitivity (CS), and subjective ratings of overall comfort with Contact Lens Dry Eye Questionnaire-8 (CLDEQ-8) test, and safety endpoints included adverse events and biomicroscopy/slit lamp examination findings.
CS was evaluated at 3, 6, 12, and 18 cycles per degree (cpd) spatial frequencies with CSV-1000-E test (VectorVision, Ohio, USA) under mesopic (3.5 cd/m2) conditions at 2.5 m without glare. The CS at different spatial frequencies was compared with the physiological CS range for normal subjects of similar ages.13 The CLDEQ-8 test was used for assessing the CL-related satisfaction levels with frequency and severity of CL-related discomfort, dryness, blurred vision, closing the eye, and removing the lens with scores from 37 of the total score.14
Study Protocol
During the first visit, subjects were screened for monocular uncorrected visual acuity (UCVA) and monocular BCVA in decimals with Snellen from 6 meters using a Topcon ACP-8 chart projector (Topcon Corporation, Tokyo, Japan) under mesopic conditions (3.5 cd/m2). All measurements were converted to the logMAR scale. Spherical, cylindrical, and keratometric measurements were performed using an RMK-800 autorefractometer keratometer (Topcon Corporation, Tokyo, Japan).
Subjects were randomized into verofilcon A, senofilcon A, or nesofilcon A lens groups and instructed to wear the lenses for at least 14 h per day (range, 10–16 h) for 28 (±2) days, with a minimum of 5 days/week starting the following day. The participants were given detailed information about possible adverse events and provided emergency communication information.
During the second visit on day 28, contact lens corrected visual acuity (CLCVA) scores were measured after 12 h of wearing DDCLs for comparative analyses. NIBUT scores were evaluated at 1, 4, 8, and 12 h. The term of NIBUT is the average time in seconds between eye opening and appearance of the first visible break in the lipid layer of the PLTF. NIBUT of the PLTF and anterior corneal higher order aberrations (HoAs) measurements were obtained from Sirius corneal topography (CSO, Firenze, Italy) device, which combines Placido disc and Scheimpflug camera systems. For measuring anterior corneal HOAs, Zernike polynomial expansions up to fourth radial order are provided for a 4 mm pupil zone.
The HoAs coefficients were evaluated at baseline, 1 and 12 h on DDCLs for 10s after blinking. In addition, CS levels were noted at the 12th h. CL wearers were instructed to complete the CLDEQ-8 questionnaire based on their CL wearing experience in the preceding 28-day period. The final decision regarding preferences using the present CLs is recorded. Adverse mechanical and inflammatory events related to CLs were noted in the safety profile.
Statistical Analyses
The R vers. 2.15.3 program (R Core Team, 2013) was used for the statistical analysis. The conformity of the quantitative data to the normal distribution was evaluated using the Shapiro–Wilk test and graphical examinations. One-way analysis of variance and post hoc evaluations with Bonferroni correction were used to evaluate normally distributed variables between more than two groups. The Kruskal–Wallis test and post-hoc evaluations with Bonferroni correction were used for intergroup evaluations of variables that did not show a normal distribution. Pearson’s chi-square test and Fisher-Freeman-Halton exact test were used to compare qualitative variables. To examine the effects of group and time factors on NIBUT and HoAs values, analysis of variance and post-hoc evaluations with Bonferroni correction were used for repeated measurements. Statistical significance was set at p <0.05.
Results
In this study, 147 eyes of 77 patients were evaluated. There were no statistically significant differences between the groups in terms of age or sex (p > 0.05). In addition, there was no statistically significant difference between the groups in terms of spherical, Kavg, UCVA, or BCVA values (p > 0.05). In the 12th h CLCVA evaluation, the mean CLCVA values of the nesofilcon A group were found to be significantly lower than those of the verofilcon A and senofilcon A groups. (p < 0.001 and p = 0.008, respectively). When BCVA and CLCVA measurements were compared, CLCVA was found to be significantly lower than BCVA measurements in the nesofilcon A group. (p < 0.001) (Table 2).
 |
Table 2 Baseline Demographics, Visual Acuity, and Refractive Data of the Study Groups |
Pre-Lens Tear Film Stability
Comparative analyses of the NIBUT scores between the study groups are summarized in Table 3. As a result of NIBUT Bonferroni-corrected post-hoc evaluations, there was no statistically significant difference between the groups in terms of NIBUT scores at baseline and after CL wearing at 1 h on day 28 (p > 0.05). There was a statistically significant difference between the groups in terms of NIBUT values at 4, 8, and 12 h (p = 0.043, p < 0.001, and p < 0.001, respectively). At 4 h, the values of the verofilcon A group were found to be higher than those of the nesofilcon A group (p = 0.041). At 8 h, the values of the nesofilcon A group were found to be lower than those of the verofilcon A and senofilcon A groups (p < 0.001 and p = 0.006, respectively). At 12 h, the values in the nesofilcon A group were lower than those in the verofilcon A and senofilcon A groups (p < 0.001 and p = 0.006, respectively). In addition, while no significant difference was found between the verofilcon A and senofilcon A groups in the measurements up to 8 h, the values of the verofilcon A group were higher than those of the senofilcon A group in measurements taken at 12 h (p < 0.001).
 |
Table 3 NIBUT Scores and Comparative Analyses of Study Groups |
After 28 days of use, when comparing the NIBUT measurements between baseline and 1 h, all groups showed significant increases in PLTF break up time scores. In the verofilcon A group, NIBUT scores were significantly lower than the baseline values at 12 h. (p = 0.999) In the senofilcon A group and nesofilcon A group; the mean NIBUT values at 1 h were significantly higher than at baseline (p = 0.002, p = 0.001) but were statistically significantly lower than the baseline values at both 8 and 12 h (p < 0.05) (Table 3) (Figure 1).
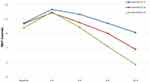 |
Figure 1 The change pattern of the study groups among NIBUT scores over time. |
The Wavefront Analysis of the Pre- Lens Tear Film
The mean coefficient of HoAs observed at baseline and 1 h was not statistically significant in any of the three groups (p > 0.05). However, the HoA scores at 12 h were significantly higher in the nesofilcon A group (p < 0.001). Post-hoc evaluation with Bonferroni correction showed that the change observed in the verofilcon A group was lower than the change observed in the senofilcon A and nesofilcon A groups (p = 0.041 and p < 0.001, respectively). Additionally, the change observed in the senofilcon A group was lower than that observed in the nesofilcon A group (p < 0.001) (Table 4).
 |
Table 4 Comparative Analyses of HoAs Scores Between the Study Groups |
The CS in mesopic conditions evaluated at different spatial frequencies and compared with the normal range with the CSV 1000-E test are summarized in Table 5. There was no statistically significant difference between the groups in terms of lower spatial frequencies of the 3 and 6 cpd CS mean values (p > 0.05). However, post-hoc evaluation with Bonferroni correction showed that the values in the verofilcon A group were higher than the nesofilcon A group values in 12 cpd measurements (p = 0.02) and 18 cpd measurements (p = 0.048). Moreover, verofilcon A group values were found to be higher than senofilcon A group values in 18 cpd measurements (p = 0.037). The mean values of the study groups were close to the normal range at lower special frequencies of 3 and 6 cpd; however, the differences became more significant at higher special frequencies of 12 and 18 cpd (Figure 2).
 |
Table 5 CS Scores and Comparative Analyses of the Study Groups |
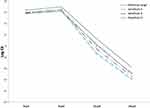 |
Figure 2 The change pattern of the study groups among CS scores over time. |
Subjective Analyses with CLDEQ-8 Test and Preference of Wear
There was a statistically significant difference between the groups in terms of the CLDEQ-8 values (p < 0.001). Nesofilcon A group values (13.2 ±1.0) were higher than those of the verofilcon A (0.8 ±0.9) and senofilcon A (11.2 ± 0.8) groups (p < 0.001 and p = 0.011, respectively). A statistically significant difference was found between the groups in terms of the percentage of preference to continue. The rate of positive preference for using nesofilcon A (20 (80%)) was lower than that of the verofilcon A (25 (96%)) and senofilcon A (24 (92%)) groups (p < 0.001 and p = 0.002, respectively).
None of the subjects experienced mechanical or infectious adverse events or discontinued lens wear. No evidence of corneal edema or chemosis was observed on biomicroscopy/slit-lamp examination during the follow-up.
Discussion
Due to the Covid-19 pandemic, the incidence of CL-related discomfort tends to increase depending on facial mask-induced tear film instability and increased screen time at home.8 In the current study, we compared the novel SiHy DDCL, verofilcon A with a commercially available SiHy DDCL and Hy DDCL in terms of PLTF stability over time and visual performance in healthcare professionals. Although the early measurements were similar, verofilcon A showed a better PLTF stability performance at extended wear times with better NIBUT score, HoAs coefficient, and CS scores at higher spatial frequencies compared to senofilcon A and nesofilcon A.
Facial mask use during the COVID-19 pandemic is a risk factor for worsening tear film parameters. A recent study conducted that the daily number of hours spent wearing a face mask correlated strongly with OSDI and corneal staining and showed a weak negative correlation with NITBUT.15 On the other hand, CLs are determined as an iatrogenic dry eye etiologic according to the 2017 Tear Film and Ocular Surface Society Dry Eye Workshop II (TFOS DEWS II).16 When compared to normal individuals, the NIBUT scores were increased at 1.2–2.6 times in all CL wearers, and the tear film thickness was decreased due to the damaged lipid layer of the PLTF.17 Therefore, it becomes a challenging problem for a healthcare professional to use CLs while wearing facial masks because of the negative alterations of the tear film stability. However, the NIBUT scores of PLTF are highly variable depending on the surface wetting ability of the CLs that interact directly with the lipid layer of the tear film.18 To the best of our knowledge, this is the first comparative study to evaluate the PLTF NIBUT of novel DDCL verofilcon A over time. In the current study, the NIBUT scores of all groups increased during the first hour of wearing according to the baseline. However, the decrease in NIBUT scores was significantly different between the groups.
Nesofilcon A is a new generation hydrogel DDCL that has a surface wetting technology with a polymer-bound macromer for maintaining a higher water content 78%.12 A stable average NIBUT score with 8 h of wearing was previously reported in both presbyopic and non-presbyopic wearers.19 However, the nesofilcon A group showed the lowest scores from the beginning of 4 h to 12 h compared to the other two SiHy DDCL groups. The lower NIBUT scores of nesofilcon A might depend on the higher dehydration rates of the high-water-content hydrogel CLs according to the new-generation SiHy CLs with enhanced surface properties and low water content.
When comparing the two SiHy DDCLs, the verofilcon A and senofilcon A groups had similar NIBUT scores until 8 h, but the differences became significant at 12 h. In vitro studies conducted with verofilcon A demonstrated superior lens-surface moisture stability compared to senofilcon A.20 The contact angles that can be used to determine wettability in the laboratory were 41.0° for verofilcon A vs 96.5° for senofilcon A with lower modulus scores in nanoindentation tests.20 Another in vitro bench study demonstrated the superiority of the aqueous film stability of verofilcon A to comparator CLs by evaluating the water breakup time.9 Moreover, in a recent study, 81% of existing CLs wearers expressed a preference for verofilcon A over their current lenses, including senofilcon A and nesofilcon A, citing all-day comfort, longer wearing time, and less disruption throughout the day time.21 Thus, different wetting technologies appear to have different abilities to maintain PLTF stability.
As the front optical surface, PLTF is a constituent factor of the optical quality of the CLs.22 In the current study, CLCVA at 12 h was lower in the nesofilcon A group. The significant decrease in vision levels in the nesofilcon A group may be associated with the more dramatically altered PLTF layer at the end of the day. In addition, the CLCVA scores were slightly higher in the verofilcon A group than in the senofilcon A group. In a recent study, it was reported that >95% eyes wearing verofilcon A CLs had CLCVA of 20/20 or better after 12 h.23
Maintaining a consistent optical surface is important for reducing light scattering and preventing optical aberrations during CL wear.24 Placido disc-based systems measure HoA coefficients derived from the front surface of the cornea with PLTF. Ruiz-Alcocer et al reported that no significant differences were found in HoAs changes with nesofilcon A and two conventional SiHy DDCLs of delefilcon A and stenfilcon A.25 In contrast, owing to the PLTF stability relation with the HoAs coefficients, the verofilcon A and senofilcon A groups showed less increase in aberrations, as expected. However, the increase in HoAs coefficients was less in the verofilcon A group than in the senofilcon A group. An in vitro study showed that verofilcon A maintained Placido ring pattern stability over a 60s dehydration interval and maintained its image quality.26 Senofilcon A group were noted similar HoAs scores to the literature (0.18 ± 0.15 µm, 0.13 ± 0.04 µm respectively).
There are a limited number of studies in the literature comparing the conventional CLs with the current study in terms of CS27,28 The CS functions of nelfilcon A, senofilcon A, and nesofilcon A were compared previously, and no significant difference was found between Hy and SiHy CLs.28 Although the scores of the three study groups were similar at higher spatial frequencies, the difference became evident in favor of verofilcon A. The results of the current study could be dependent on the superiority of unique surface wetting technologies, which provide a better optical surface.
In line with the PLTF stability results, the subjects of the SiHy DDCLs of the study groups gave better CLDEQ-8 test scores than the hydrogel nesofilcon A group (p < 0.001). The high oxygen transmissibility of SiHy DDCLs has been associated with improved patient symptoms of comfort, including dryness and wear time.29 Cummings et al reported that the mean subjective ratings for overall vision, comfort, and handling were greater than 9 out of a possible 10 after a 3-month-wear time.23 On the other hand, in a recent metanalyses, the mean CLDEQ-8 score was reported very similar to the current results for senofilcon A (11.9 (±0.9), 11.2 (±0.8), respectively).11
Discontinuation of lens wear is a major problem in contact lens compliance. Dropout rates in the first year are 20%–25% and of these, 41% problems with vision and 36% discomfort.30 The rates of positive preference for DDCLs were significantly higher in the verofilcon A and senofilcon A groups (96%, 92% respectively). Similarly, the discontinuation rates of verofilcon A were reported (2.8%) previously.23 Moreover, Grant et al reported that 94% of the subjects agreed with the statement that “is the CL I will continue to wear in the future”. In the same study, after experiencing verofilcon A, current CLs wearers, including both senofilcon A and nesofilcon A, showed a significantly higher preference for verofilcon A because of long-lasting comfort (86%).21
Similar to a previous study with verofilcon A, mechanical or inflammatory CL-related adverse events were not observed in any of the subjects in the present study.23 These findings demonstrate that the DDCLs used in the current study were safe for prolonged use with facial masks.
This study has a few limitations, including its short-term nature and small sample size. Another limitation was the inability to use single- or double-masked CLs in the study groups. The reason for the preference to continue or not continue using the CLs was not investigated. Assessment of the NIBUT over time ended at 12 h. However, most individuals wore their CLs over 12 h daily. Therefore, it would be better to evaluate the long-term results of the NIBUT scores.
Conclusion
The results of the current study conducted the superiority of SiHy DDCLs of verofilcon A and senofilcon A CLs in terms of PLTF stability and visual performance against Hy DDCL nesofilcon A in prolonged use with facial masks. However, verofilcon A showed a better performance with respect to senofilcon A as determined by NIBUT and HoAs scores at 12 h and CS measurements at higher spatial frequencies. Thus, the verofilcon A lens may be one of the best options for those seeking stable visual performance with prolonged facial mask usage in challenging environments. Moreover, our results suggest a safety profile for the three CLs without remarkable adverse events. Further clinical trials are warranted to evaluate the long-term prolonged use of DDCLs.
Data Sharing Statement
Data are available on request from the authors.
Informed Consent
Written informed consent was obtained for identifiable health information included in this study. The manuscript has been read and approved by all authors. In addition, each author believes that the manuscript represents an honest work.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by an investigator-initiated trial grant IIT #66288565 from Alcon SA.
Disclosure
The authors declare no conflicts of interest regarding this work.
References
1. Scalinci SZ, Pacella E, Battagliola ET. Prolonged face mask use might worsen dry eye symptoms. Indian J Ophthalmol. 2021;69:1508–1510. doi:10.4103/ijo.IJO_2641_20
2. Krolo I, Blazeka M, Merdzo I, et al. Mask-associated dry eye during COVID-19 pandemic-how face masks contribute to dry eye disease symptoms. Med Arch. 2021;75:144–148. doi:10.5455/medarh.2021.75.144-148
3. Matusiak Ł, Szepietowska M, Krajewski P, et al. Inconveniences due to the use of face masks during the COVID −19 pandemic: a survey study of 876 young people. Dermatol Ther. 2020;33:e13567. doi:10.1111/dth.13567
4. Vianya-Estopa M, Wolffsohn JS, Beukes E, et al. Soft contact lens wearers’ compliance during the COVID-19 pandemic. Contact Lens Anterior Eye. 2021;44:101359. doi:10.1016/j.clae.2020.08.003
5. Craig J, Willcox M, Argueso P, et al. The TFOS international workshop on contact lens discomfort: report of the contact lens interactions with the tear film subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS123–TFOS156.
6. Guillon M, Dumbleton K, Theodoratos P, et al. Pre-contact lens and pre-corneal tear film kinetics. Cont Lens Anterior Eye. 2019;42:246–252. doi:10.1016/j.clae.2019.02.001
7. Guillon M, Dumbleton KA, Theodoratos P, et al. Association between contact lens discomfort and pre-lens tear film kinetics. Optom Vis Sci. 2016;93:881–891. doi:10.1097/OPX.0000000000000866
8. Johnson & Johnson Vision. JOHNSON & JOHNSON VISION SURVEY FINDS WESTERN EUROPEAN CONTACT LENS WEAR IS RECOVERING AS LOCKDOWNS EASE. Available from: https://www.jjvision.com/press-release/johnson-johnson-vision-survey-finds-western-european-contact-lens-wear-recovering
9. Tucker BLE, Bauman E, Subbaraman L. Characterization of the surface properties of a novel daily disposable silicone hydrogel contact lens.
10. Tutt R, Bradley A, Begley C, et al. Optical and visual impact of tear break-up in human eyes. Invest Ophthalmol Vis Sci. 2000;41:4117–4123.
11. Bishop MJ, Sun CK, Coles-Brennan C, et al. Evaluation of daily disposable senofilcon A contact lenses in a symptomatic population. Cont Lens Anterior Eye. 2022;45:101574. doi:10.1016/j.clae.2022.101574
12. Montani G, Martino M. Tear film characteristics during wear of daily disposable contact lenses. Clin Ophthalmol. 2020;14:1521–1531. doi:10.2147/OPTH.S242422
13. Pomerance GN, Evans DW. Test-retest reliability of the CSV-1000 contrast test and its relationship to glaucoma therapy. Invest Ophthalmol Vis Sci. 1994;35:3357–3361.
14. Dogan AS, Karabulut E, Gurdal C. Validation and reliability of the Turkish version of Contact Lens Dry Eye Questionnaire-8 (CLDEQ-8). Cont Lens Anterior Eye. 2020;43:472–475. doi:10.1016/j.clae.2020.02.002
15. Shalaby HS, Eldesouky MEE. Effect of facemasks on the tear film during the COVID-19 pandemic. Eur J Ophthalmol. 2022;11206721221110010. doi:10.1177/11206721221110010
16. Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15:511–538. doi:10.1016/j.jtos.2017.05.004
17. Guillon M, Maissa C. Contact lens wear affects tear film evaporation. Eye Contact Lens. 2008;34:326–330. doi:10.1097/ICL.0b013e31818c5d00
18. Thai LC, Tomlinson A, Doane MG. Effect of contact lens materials on tear physiology. Optom Vis Sci. 2004;81:194–204. doi:10.1097/00006324-200403000-00012
19. Lorente-Velázquez A, García-Montero M, Gómez-Sanz FJ, et al. Comparison of the impact of nesofilcon A hydrogel contact lens on the ocular surface and the comfort of presbyopic and non-presbyopic wearers. Int J Ophthalmol. 2019;12:640–646. doi:10.18240/ijo.2019.04.19
20. SIBF. Surface characterization methods developed to optimize the “SMARTSURFACE®” chemistry for Precision1™ (One Day Contact Lenses).
21. Grant T, Tang A. A survey of contact lens wearers and eye care professionals on satisfaction with a new smart-surface silicone hydrogel daily disposable contact lens. Clin Optom. 2020;12:9–15. doi:10.2147/OPTO.S233328
22. Koh S, Watanabe K, Nishida K. Objective evaluation of on-eye optical quality of daily disposable silicone hydrogel contact lens with internal wetting agents. Clin Ophthalmol. 2019;13:2159–2165. doi:10.2147/OPTH.S224450
23. Cummings S, Giedd B, Pearson C. Clinical performance of a novel daily disposable soft contact lens. JCLRS. 2020;4:e23–e30. doi:10.22374/jclrs.v4i1.39
24. Schafer J, Steffen R, Reindel W, et al. Evaluation of surface water characteristics of novel daily disposable contact lens materials, using refractive index shifts after wear. Clin Ophthalmol. 2015;9:1973–1979. doi:10.2147/OPTH.S90376
25. Ruiz-Alcocer J, Monsálvez-Romín D, García-Lázaro S, et al. Impact of contact lens material and design on the ocular surface. Clin Exp Optom. 2018;101:188–192. doi:10.1111/cxo.12622
26. Boojari S, Schwiegerling J. Measurement of the optical quality of contact lens materials with dehydration. Invest Ophthalmol Vis Sci. 2019;60:6346.
27. Wachler BS, Phillips CL, Schanzlin DJ, et al. Comparison of contrast sensitivity in different soft contact lenses and spectacles. Clao j. 1999;25:48–51.
28. Sapkota K, Franco S, Lira M. Contrast sensitivity function with soft contact lens wear. J Optom. 2020;13:96–101. doi:10.1016/j.optom.2020.01.002
29. Papas EB. The significance of oxygen during contact lens wear. Cont Lens Anterior Eye. 2014;37:394–404. doi:10.1016/j.clae.2014.07.012
30. Sulley A, Young G, Hunt C, et al. Retention rates in new contact lens wearers. Eye Contact Lens. 2018;44(Suppl 1):S273–s282. doi:10.1097/ICL.0000000000000402
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
