Back to Journals » Clinical Optometry » Volume 14
Comparison of Short-Term Effects of Treatment of Accommodative Infacility with Low Plus Addition in Single Vision Rx or Vision Therapy: A Pilot Study
Authors Balke M, Skjöld G, Lundmark PO
Received 23 December 2021
Accepted for publication 20 April 2022
Published 2 June 2022 Volume 2022:14 Pages 83—92
DOI https://doi.org/10.2147/OPTO.S355508
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Mr Simon Berry
Martin Balke,1 Göran Skjöld,2 Per O Lundmark1
1Department of Optometry, Radiography and Lighting Design, Faculty of Health and Social Sciences, University of South-Eastern Norway, Kongsberg, Norway; 2Private Practicing Optometrist, Skjöld/Skjöld & Grönvall, Malmoe, Sweden
Correspondence: Per O Lundmark, Department of Optometry, Radiography and Lighting Design, Faculty of Health and Social Sciences, University of South-Eastern Norway, Hasbergsvei 36, Kongsberg, NO-3616, Norway, Tel/Fax +47 31 00 89 37, Email [email protected]
Purpose: To compare the short-term treatment effect of low plus reading addition (ADD) and home-based vision therapy (VT) in a small group of symptomatic children with accommodative infacility (AIF) being the most significant dysfunction.
Methods: Nineteen children, 8 to 12 years of age, with a first-time diagnosis of AIF were consecutively and alternately allocated to treatment with ADD (+0.50 D addition in single vision Rx) or VT (accommodation exercises using Hart Charts) for a period of 6 weeks. Accommodation facility (AF) was measured monocularly (MAF-R, MAF-L) and binocularly (BAF) with +2 D/-2 D flipper and registered in cycles per minute (cpm). Symptoms were graded using the convergence insufficiency symptom survey (CISS). Measurements were compared before and after treatment and between groups using nonparametric statistics (p < 0.05).
Results: Ten children were allocated to ADD (median age 9.0 F:5) and 9 to VT (median age 11.0 F:7). Baseline median measurements of MAF-R, MAF-L, BAF and CISS were 3.0, 3.0, 2.2 cpm, and 27.5 points, respectively, for ADD, and 2.0, 2.0, 2.0 cpm, and 27.0 points, respectively, for VT. There were no significant differences between groups at baseline. After 6 weeks of treatment, the median change of MAF-R, MAF-L, BAF and CISS was +5.0, +4.5, +4.7 cpm, and – 7.5 points, respectively, for ADD and +8.0, +8.0, +10.0 cpm, and – 20.0 points, respectively for VT. All changes within groups were significant. Comparison of groups showed a significantly greater effect of treatment with VT compared to ADD for BAF (p = 0.008) and CISS (p = 0.017).
Conclusion: In children with newly diagnosed AIF, treatment with accommodation exercises for 6 weeks gives greater short-term relief of symptoms and improvement of binocular accommodative facility compared to treatment with spectacle single vision correction with a weak plus addition.
Keywords: accommodative dysfunction, infacility, +2/-2 flipper, Hart Chart, CISS
Introduction
Accommodative infacility (AIF) is also known as inertia of accommodation or tonic accommodation.1,2 It is defined as a sluggish shift of focus between distance and near1,3 and causes blurry vision at distance or near, headaches, tiredness around the eyes, or asthenopia,1,3,4,5 especially in relation to near work.6 AIF is the second most common accommodation dysfunction found in children.1–3 If left untreated AIF may affect the child’s ability to read, reduce concentration and increase stress level.6–8 Studies have indicated a prevalence from about 5% in children and adolescents9 to 28% in symptomatic young people.10,11
Accommodative facility (AF) is assessed monocularly (MAF) by measuring cycles of shifts per minute between two levels of accommodation (eg, +2 Diopter (D) vs −2 D). In a clinical setting the patient fixates on a detailed object at 40 cm and reports when it is seen clearly while the accommodative effort is alternated by means of a handheld +2 D/-2 D flipper as often as possible during one minute.5,12 AIF is characterized by MAF below normative values (Table 1), with equal ability to clear to plus and minus lenses, a normal accommodative amplitude (AA) and low negative relative accommodation (NRA) and positive relative accommodation (PRA) values.5
 |
Table 1 Normative Values for Subjects Aged 8–12 Years5 |
Accommodative infacility is normally both diagnosed and treated in optometric practice. There is no general consensus on treatment but, full correction is normally the first step.1,5,7,13,14 Treatment of AIF is typically in the form of vision therapy.15 Clinical guidelines of the American Optometric Association recommend vision therapy as a first line treatment of accommodative and vergence dysfunctions.7 However, in clinical practice preferences may be different. For instance, in Norway a low plus addition as a single vision prescription may be more widely used as a first line treatment of AIF rather than vision therapy. The rationale is that a low addition single lens correction will trigger the accommodative effort by improving near visual acuity16 with an acceptable blur of distance vision. Treatment of accommodative dysfunctions is not refundable in Norway. This makes low addition single vision prescription an attractive solution to improve symptoms, although the underlying problem is not adequately targeted.17
The extent to which low plus add may be regarded as a justifiable first line option of treatment of AIF is scarcely explored in general, including in the Norwegian optometric population. Therefore, the purpose of this study was to investigate the effect of 6 weeks of treatment with a low add correction compared with home-based vision therapy on AF and symptoms in children with recently diagnosed AIF. We hypothesized that the effect of treatment would be different for the compared treatments. Results are expected to improve our understanding of the efficiency of treatment options and to contribute to development of clinical guidelines for optometrists.
Methods
Recruitment
This prospective intervention study was conducted in a private optometric practice in the municipality of Flekkefjord in the south of Norway. The study was approved by the Regional Ethical Committee in Southeast Norway and adhered to the tenets of the Helsinki Declaration.
Invited into the study were Norwegian schoolchildren aged 8 to 12 with symptoms related to near work in school or at home. Invitations were distributed via the Pedagogical Psychological Services and the Municipal Education in Flekkefjord, to staff, teachers, and parents. Children with symptoms were offered an optometric examination free of charge during the period October 2016 to February 2017. Written information about the study was given to the invited child and parents with time for questions. Children whose parents gave their consent for participation were included into the study. Optometric examinations, diagnostic assessments and follow-up assessments were performed unmasked by one senior optometrist (M.B.). Recruitment was consecutively performed. Standard tests were in accordance with The Norwegian Association of Optometry’s clinical guidelines.18 The standard tests included cover test and eye motility and uncorrected vision acuity. Refractive error was examined and corrected based on cycloplegic refraction minus 0.50 D. Residual accommodation, post-cyclo, was measured 40 minutes after administration of cycloplegic drops (Cyclopentolate 1%, Chauvin) with the cycloplegic refraction in a trial frame using an RAF-rule. A cut-off of 0.5 D was chosen to exclude subjects with uncorrected latent hypermetropia from the sample. Patients with residual accommodation less than 0.5 D, were given a new correction that was used a minimum of 4 weeks prior to the binocular measurements. Binocular measurements were performed in the following order, with the patients wearing adequate correction: Stereoscopic acuity using TNO Stereo Test, near point of convergence (NPC), BAF, MAF, vergence facility, phoria distance, negative and positive fusional vergence at distance, phoria near, negative and positive fusional vergence at near, binocular crossed cylinder test (BCC), NRA, PRA, and accommodative amplitude monocularly.
Measurements
Accommodative amplitude (AA) and NPC were measured using an RAF-ruler. Phoria at distance and near, BCC, vergence facility, and negative and positive accommodation reserves (NRA/PRA) were measured as described by Scheiman & Wick.5 Monocular accommodative facility (MAF) and binocular accommodative facility (BAF) was assessed with a +2 D/-2 D flipper at 40 cm with adopted distance correction in a trial frame. The power +2 D/–2 D represents an accommodative effort that is well within the expected accommodative amplitude in the examined group. It was decided to use this routine rather than an amplitude scaled facility, in which case testing should have been done at 18 cm:s. Amplitude scaled facility testing is by Scheiman & Wick recommended from 13 years of age, and for ages 8–12 years +2 D/-2 D at 40 cm is recommended.5 Results were compared with norms for testing at 40 cm (Table 1). The subject viewed a 0.7 line on a near chart and was instructed to report loudly every time letters were clear after a shift of lenses, in which case the lenses were flipped over. Included into the study were children with MAF ≤ 4.5 cycles per minute (cpm) in either eye, with equal ability to clear plus and minus lenses, with BAF < 2.5 cpm below MAF for each eye and with a moderately reduced monocular AA, defined as < 3 D below minimum expected value (Table 1).5 A BAF of 2 cpm or more below MAF in both eyes was used as a possible indicator of convergence insufficiency. Moderately reduced AA was used as inclusion criteria to reflect the coexistence of AIF and reduced accommodative amplitude commonly seen in a clinical setting.
Excluded were children with findings that suggested other accommodative dysfunctions or vergence dysfunctions, such as NPC > 10 cm, AC/A ratio outside 3–5 diopters per prism diopter, detected LAG or LEAD or not met Sheard's criterion, as well as children with conditions requiring treatment and follow-up by other health care professionals. Other exclusion criteria were contraindication to the use of cycloplegics, amblyopia with acuity < 0.5, manifest strabismus, astigmatism ≥ 2.50 Diopter Cylinder (DC) in either eye, and anisometropia ≥ 1.50 Diopter Sphere (DS). Excluded patients were managed according to the diagnosed condition in each case. Management of these patients is not included in this report. A new appointment was booked for commencement of treatment regimen.
Allocation to Treatment Groups
Recruited and adequately visually corrected children were systematically allocated to one of two treatment regimens; low plus reading addition (ADD) or vision therapy (VT) for a period of 6 weeks. The length of the period was chosen to be long enough to obtain a response but short enough to encourage compliance, and to avoid possible effects on myopia progression due to under corrected refractive error. The allocation was performed at random for the first participant and in a systematic and alternating manner for the following participants to avoid unequal sizes of groups by chance. The ADD-regimen consisted of wearing single vision correction for distance use, and a single vision correction with add +0.50 D for indoor use and reading. Emmetropic children were given a correction of +0.50 D for indoor and reading use only. The power of the addition represents a commonly used low plus addition for single vision correction when prescribed as first line treatment of AIF by Norwegian optometrists. Dispensed lenses were standard plastic single vision lenses (CR39) with anti-reflex coating. Treatment and dispensed glasses were for free. The VT-regimen consisted of orthoptic therapy using standardized Hart Chart accommodative rock exercises once a day, five days a week, for a period of ten minutes per therapy session. Exercises with Hart Chart with purpose to restore normal accommodation facility are described by Scheiman & Wick.5 A slightly modified version of the exercise was practiced in the study. With one eye covered the child was asked to read out load letters seen alternately on a large Hart Chart with 10 rows and 10 columns of letters with font size 36, mounted on a wall at 3 m and on a small Hart Chart with letter size corresponding to a visual acuity of 0.7, held at a distance of 10–15 cm. The sequence was repeated as fast as possible until all rows with four letters on each chart had been read out correctly for five minutes. The therapy was then repeated for the other eye for five minutes. The initial therapy session was performed in optometric practice to demonstrate the procedure for the child and accompanying parent, who also were given a written instruction of the Hart Chart regimen. Subsequent sessions were performed at home under the supervision of a parent.
Subjective symptoms were measured using the Convergence Insufficiency Symptom Survey (CISS).19 The questionnaire includes 15 symptom-related items graded from 0 (never), 1 (seldom), 2 (sometimes), 3 (often), to 4 (always). The sum of scores (0–60) provides an indicator of the impact of symptoms. The CISS questionnaire was initially developed to grade symptoms in patients with convergence insufficiency. Since symptoms due to different binocular dysfunctions are similar,5 it was decided to use this questionnaire to grade symptoms in the examined group. The outcome of use of the questionnaire in this study, can therefore not be compared with the outcome reported in the CITT-study.17 The questionnaire was filled out by the child together with the accompanying parent. However, the parent was carefully instructed to read the question, but not to explain or otherwise help the child with answering the questions.
To encourage motivation and compliance follow-up appointments were scheduled at +1 week, +3 weeks, and +5 weeks into the allocated treatment regimen in both groups. All patients conformed with the set dates for follow-up appointments. At the visits, the progress was evaluated by assessment of accommodation facility and symptoms. Home compliance was encouraged by frequent telephone calls to parents. A final follow-up appointment was arranged within 2 weeks after the completion of the treatment regimen when all measurements except cycloplegic refraction were repeated. At every follow-up visit all measurements were performed with the patients using the same correction that was used when the therapy was initiated, ie the patients that started uncorrected remained uncorrected during the study, while patients that were corrected used the same refractive correction during the study.
Analysis
Normal distribution and homogeneity of data were tested with the Kolmogorov Smirnov test and Levene’s test for equal variance. As assumptions were violated for the small samples, non-parametric tests were employed for descriptive and inferential statistics. Within treatment groups, comparisons of outcome measures before and after completed treatment were performed by means of Wilcoxon signed rank test whereas between treatment groups, comparisons of change of outcome measures were performed by means of Mann–Whitney U test (SPSS, v.23, IBM). Comparison of groups were performed by means of Mann–Whitney U and Chi-Square tests. Statistical significance was set at p < 0.05 (two-tailed test). Based on normative values of MAF a sample size of 10 in each group was estimated as sufficient to indicate a large effect size (Cohen’s d > 0.8) of measured difference between the groups, with a statistical power of 80%.
Results
During a recruitment period of 5 months 21 children fulfilled the inclusion criteria. Of these parents of two children declined participation due to long distance travel or other priorities. Thus, nineteen children with first time diagnosis of AIF were included in the study (Table 2). There were no dropouts during the treatment period.
 |
Table 2 Demographics and Refractive Status of Participants |
Ten children (median age 9.0 yrs., Females (F):5) were allocated to ADD whereas 9 (median age 11.0 yrs., F:7) were allocated to VT. There were slightly more girls in the VT group (+10.5%) and median age was two years older than in the ADD group, however none of these differences reached statistical significance. Refraction and visual acuity were not statistically significant different between the groups but there was a greater spread of spherical and astigmatic refractive error among children in the VT group.
Binocular and accommodative status of participants are displayed in Table 3. Median NPC was 2.5 cm greater for VT compared with ADD (p = 0.035). Comparison of other measurements did not reach statistical significance.
 |
Table 3 Binocular Status of Participants |
Median baseline measurements of MAF-R, MAF-L, BAF and CISS were 3.0 cpm, 3.0 cpm, 2.2 cpm and 27.5 points, respectively in the ADD group, and 2.0 cpm, 2.0 cpm, 2.0 cpm and 27.0 points, respectively in the VT group (Table 4). There were no statistical significant differences between groups at baseline.
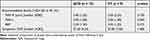 |
Table 4 Baseline Measurements |
After 6 weeks of treatment the change of median MAF-R, MAF-L, BAF and CISS was +4.5 cpm, +4.5 cpm, +3.2 cpm and −10.0 points, respectively in the ADD group, and +7.0 cpm, +7.0 cpm, +10.0 cpm and −17.0 points, respectively in the VT group (Table 5). The median change of MAF-R, MAF-L, BAF and CISS was +5.0 cpm, +4.5 cpm, +4.7 cpm and –7.5 points, respectively, in the ADD group and +8.0 cpm, +8.0 cpm, +10.0 cpm and –20.0 points, respectively, in the VT group (displayed in Figures 1 and 2). All changes within groups were statistically significant.
 |
Table 5 Comparison of Outcome Measurements Before and After 6 Weeks of Treatment |
Comparison of changes between groups showed a significantly greater effect of treatment with VT compared to ADD for BAF (p = 0.008) (Figure 1) and CISS (p = 0.017) (Figure 2).
Discussion
The purpose of the study was to investigate the short-term effect of treatment with a low plus add correction in comparison with vision therapy on accommodative facility and symptoms in children with recently diagnosed AIF as the most significant accommodative dysfunction. In the studied group, MAF was below expected values, with equal reaction to plus and minus lenses, both NRA and PRA was also low, which is consistent with AIF. In the group accommodative amplitude was slightly (1D) below the minimum expected value. NPC was slightly beyond expected values in both the ADD and in the VT-group, which could indicate convergence insufficiency. However, patients with BAF more than 2 cpm below MAF for both eyes, were excluded. All patients in the group had normal AC/A values, which contradicts the diagnosis of convergence insufficiency, as well as both NRA and PRA being low. The equally low values for NRA and PRA suggest that neither basal exophoria or basal esophoria was the probable diagnosis for the group. There was neither LAG nor LEAD in the included patients. In summary this indicates that AIF with comorbid AI is the most significant diagnosis for accommodative dysfunction in the examined group. Both treatments showed significant improvement of facility and less symptoms after 6 weeks of treatment, however the improvements seen with active treatment with VT were nearly double in magnitude compared with those seen with passive treatment with ADD for both AF and symptoms. As far as the immediate effects are concerned the results point toward VT as the treatment of choice in children with accommodative dysfunction with AIF as the most significant accommodative dysfunction.
Various studies have suggested that vision therapy is successful in alleviating symptoms of accommodative dysfunction and improving accommodation performance.4,20–24 However, the effect of VT on AIF when it is described as the most significant accommodative dysfunction, has been less investigated. In a Swedish study of 9 to 14 years old children with accommodative infacility Sterner et al25 compared the effect of accommodative therapy with a dioptric flipper with sham treatment. Following a therapy period of on average 8 weeks the accommodative function increased significantly and was reported to remain unaltered 2 years after the study.25 The effect on the accommodative facility was not reported although the authors conclude that it was improved after treatment.25 In a study by Brautaset et al,26 treatment with +1.00 D add was compared with treatment with accommodative flippers (+1.5 D/-1.5 D) in children with accommodative insufficiency. Their study showed greater improvement of both accommodative amplitude and facility for treatment with flippers compared to +1.00 D addition. Cooper et al4 conducted a well-controlled study in five patients with accommodative dysfunctions. Accommodative facility therapy resulted in an improvement of accommodative amplitude and facility, and a decrease in asthenopia in 4 out of 5 cases. AF was not quantified but assessed on ability to monocularly clear a −2 D lens within 5 sec. Nevertheless, our results are in concordance with these observations, and with those in the studies of Sterner et al25 and Brautaset et al.26 In a more recent study Scheiman et al27 examined the effect of office-based vision therapy in children and adolescents between the ages of 9 and 17 with convergence insufficiency and a comorbid accommodative dysfunction (the Convergence Insufficiency Treatment Trial – Attention and Reading Trial (CITT-ART)). Monocular accommodative facility improved by on average 8.8 cpm (p < 0.001) during the first eight weeks, which is of the same magnitude as in our study. Slightly greater improvement of average accommodative facility was found in a subsample of children 9- to 14-years old in, the CITT-ART study.27 However, a direct comparison is not straight forward because convergence insufficiency was not a criteria for inclusion in our study.
Plus lenses are listed as an optional treatment of accommodation infacility in the Clinical guidelines of the American Optometry Association.7 The primary purpose is to decrease the demand on the accommodative system and to alleviate associated symptoms. The role of plus lenses is said to also reduce blur to an extent where it helps the adaptive mechanism within the accommodative system to regain normal capacity.16 There is, however, no consensus on what an appropriate power for the plus lenses is. Studies that have investigated the effect of plus lenses in the treatment of accommodative insufficiency have indicated similar improvements on accommodative performance and symptoms as for vision therapy when using a +1.00 D addition,28 although less effect when using a higher addition, i.e., +2.00 D.20,28,29 In this study a +0.50 D addition was chosen in a single vision correction. The argument for this choice in optometric practice is to avoid extensive blur at distance and increase the likelihood for compliance since distance vision is important in schoolwork. To the best of our knowledge there are no studies that have investigated the effect of such a low addition, nor in comparison with vision therapy or in patients with AIF as the most significant accommodative dysfunction. Hence, the presented results provide a first-time indication of a poorer short term effect of treatment with a plus lens correction in comparison with vision therapy on AF and symptoms in children with recently diagnosed AIF.
The study design was chosen to make it possible to investigate short term effect of different interventions and to compare results between groups. However, allocation to different interventions was not randomized. This may have caused a selection bias due to unequal distribution of factors that modify adherence with, or the response to the interventions. Socio-economic factors such as parental fluency in the national language, level of education, and acuity at the start of treatment have been shown to influence compliance in amblyopia therapy of youngsters,30 whereas severity of uncorrected refractive error and lower levels of uncorrected visual acuity may influence compliance of spectacle wear.31 The fact that the socio-economic status of parents was not addressed weakens the results of this study. However, refractive, and visual status were included and did not indicate a differential bias for the treatment groups. Nevertheless, the interventions themselves may have caused differences in compliance. This risk come to the forefront when comparing passive intervention of wearing glasses with active intervention that requires recurrent visual therapy exercises. Studies of children in the western world have indicated that up to 86% may be compliant with wearing glasses.32 In this study compliance was encouraged by follow-up visits in the clinic every 14th day throughout the intervention period but was not assessed or measured in any way. This weakens the validity of the findings. Measurements were obtained unmasked by one observer, which may have induced bias if instructions were different in the two treatment groups because of expectations of the observer. This too weakens the validity of the results. However, blinded measurements were not practically possible in this study and hence, results must be viewed with this kept in mind. Regarding factors that may modify the response to interventions it is apparent that binocular status is a potential candidate due to the close relationship between accommodation and convergence. NPC was the only measurement that was statistically significant different in the two groups. Children in the VT group had higher median NPC compared with children in the ADD group. Hart Chart exercises were performed monocularly and would not be affected by an increased NPC. Most likely the same holds true for monocular outcome measurements such as MAF. On the other hand, there is a possibility that binocular outcome measurements could be adversely affected by the increased NPC. Since BAF is affected by both accommodative and vergence function, and VT in the study was monocular, the effect on BAF was expected as seen in the VT treatment group. The same may hold true for subjective symptoms measured with the CISS, which reflects both binocular and accommodative challenges associated with near work.16 In summary, repeated study design and a defined homogenous cohort of participating children are major strengths whereas unmasked data collection and lack of control of compliance and influencing factors are major weaknesses of this study. The short period, 6 weeks of VT, may be too short for subjects to achieve permanent relief, which should be considered when judging the results.
Conclusion
This pilot study indicates that active treatment with accommodative exercises for 6 weeks gives greater short-term relief of symptoms and improvement of binocular accommodative facility compared to passive treatment with spectacle single vision correction with a weak plus addition in children with newly diagnosed accommodative infacility. Further studies on the sustained effect are advised.
Acknowledgments
Our acknowledgement goes to the study participants and their parents/guardians for their willingness to take part in this study. Data published in this article has been presented as a conference abstract at ARVO Annual Meeting in 2018.
Disclosure
Göran Skjöld is via HB Sekon, the distributor of HTS software in the Nordic countries. The authors report no other conflicts or competing interest in this work.
References
1. Duane A. Anomalies of the accommodation clinically considered. Trans Am Ophthalmol Soc. 1915;14(Pt 1):386.
2. Hokoda S. General binocular dysfunctions in an urban optometry clinic. J Am Optom Assoc. 1985;56(7):560–562.
3. Daum K. Accommodative dysfunction. Doc Ophthalmol. 1983;55(3):177–198. doi:10.1007/BF00140808
4. Cooper J, Feldman J, Selenow A, et al. Reduction of asthenopia after accommodative facility training. Optometry Vision Sci. 1987;64(6):430–436. doi:10.1097/00006324-198706000-00008
5. Scheiman M, Wick B. Clinical Management of Binocular Vision: Heterophoric, Accommodative, and Eye Movement Disorders.
6. Kiely PM, Crewther SG, Crewther DP. Is there an association between functional vision and learning to read? Clin Exp Optom. 2001;84(6):346–353. PMID: 12366360. doi:10.1111/j.1444-0938.2006.00090.x
7. Cooper JS, Burns CR, Cotter SA, Daum KM, Griffin JR, Scheiman M. Care of the patient with accommodative and vergence dysfunction. USA: American Optometric Association; 2010. Available from: https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/Consensus-based%20guidelines/Care%20of%20Patient%20with%20Accommodative%20and%20Vergence%20Dysfunction.pdf.
8. Garzia RP, Richman JE. Accommodative facility: a study of young adults. J Am Optom Assoc. 1982;53(10):821–825.
9. Dwyer P, Bentleigh V. The prevalence of vergence accommodation disorders in a school‐age population. Clin Exp Optom. 1992;75(1):10–18. doi:10.1111/j.1444-0938.1992.tb01010.x
10. Hennessey D, Iosue RA, Rouse MW. Relation of symptoms to accommodative infacility of school-aged children. Optometry Vision Sci. 1984;61(3):177–183. doi:10.1097/00006324-198403000-00005
11. Montés-Micó, R. Prevalence of general dysfunctions in binocular vision. Ann Ophthalmol. 2001;33:205–208. doi:10.1007/s12009-001-0027-8.
12. Zellers JA, Alpert TL, Rouse MW. A review of the literature and a normative study of accommodative facility. J Am Optom Assoc. 1984;55(1):31–37. PMID: 6699343.
13. Rouse MW. Management of binocular anomalies: efficacy of vision therapy in the treatment of accommodative deficiencies. Optometry Vision Sci. 1987;64(6):415–420. doi:10.1097/00006324-198706000-00006
14. Rutstein RP, Daum KM. Anomalies of Binocular Vision: Diagnosis & Management. Mosby Incorporated; 1998.
15. Dwyer P, Wick B. The influence of refractive correction upon disorders of vergence and accommodation. Optometry Vision Sci. 1995;72(4):224–232. doi:10.1097/00006324-199504000-00002
16. Ciuffreda KJ. The scientific basis for and efficacy of optometric vision therapy in nonstrabismic accommodative and vergence disorders. Optometry. 2002;73(12):735–762. PMID: 12498561.
17. Scheiman M, Cotter S, Kulp MT, et al. Treatment of accommodative dysfunction in children: results from a random clinical trial. Optom Vis Sci. 2011;88(11):1343. doi:10.1097/OPX.0b013e31822f4d7c
18. Clinical guidelines, Standard Optometric Examination (2017) of the Norwegian Association of Optometry (NAO), [Kliniske retningslinjer - Rutineundersøkelser R1 (2017), Norges Optikerforbund]. Available from: https://www.optikerne.no/getFile.php?ID=5a0bef51c9e6dee843fc62c0b9aceb4c39031179168594dcfd25ad2b418134e44095f064.
19. Borsting EJ, Rouse MW, Mitchell GL, et al. Validity and reliability of the revised convergence insufficiency symptom survey in children aged 9 to 18 years. Optom Vis Sci. 2003;80. doi:10.1097/00006324-200312000-00014
20. Daum KM. Orthoptic treatment in patients with inertia of a commodation. Aust J Optom. 1983;66(2):68–72. doi:10.1111/j.1444-0938.1983.tb01537.x
21. Hoffman L, Cohen AH. Effectiveness of non strabismic optometric vision training in a private practice. Am J Optom Physiol Arch Am Acad Opt. 1973;50:813–816. doi:10.1097/00006324-197310000-00008
22. Levine S, Ciuffreda K, Selenow A, Flax N. Clinical assessment of accommodative facility in symptomatic and asymptomatic individuals. J Am Optom Assoc. 1985;56(4):286–290.
23. Liu J, Lee M, Jang J, et al. Objective assessment of accommodation orthoptics I. Dynamic insufficiency. Amer J Optom Physiol Opt. 1979;56:285–294. doi:10.1097/00006324-197905000-00002
24. Wold RM, Pierce JR, Keddington J. Effectiveness of optometric vision therapy. J Am Optom Assoc. 1978;49:1047–1059.
25. Sterner B, Abrahamsson M, Sjöström A. Accommodative facility training with a long term follow up in a sample of school aged children showing accommodative dysfunction. Doc Ophthalmol. 1999;99(1):93–101. doi:10.1023/A:1002623107251
26. Brautaset R, Wahlberg M, Abdi S, Pansell T. Accommodation insufficiency in children: are exercises better than reading glasses? Strabismus. 2008;16(2):65. doi:10.1080/09273970802039763
27. CITT-ART Investigator Group, Scheiman, M., Mitchell, G. L., Cotter, S. A., Kulp, M., Chase, C., Borsting, E., Arnold, E., Denton, C., & Hertle, R. (2015). Convergence Insufficiency Treatment Trial - Attention and Reading Trial (CITT-ART): Design and Methods. Vision development and rehabilitation, 1(3), 214–228.
28. Abdi S, Brautaset R, Rydberg A, Pansell T. The influence of accommodative insufficiency on reading. Clin Exp Optom. 2007;90:36–43. doi:10.1111/j.1444-0938.2006.00090.x
29. Wahlberg M, Abdi S, Brautaset R. Treatment of accommodative insufficiency with plus lens reading addition: is +1.00 D better than +2.00 D? Strabismus. 2010;18(2):67–71. doi:10.3109/09273972.2010.485243
30. Loudon SE, Fronius M, Looman CW, Awan M, Simonsz HJ, Simonsz H. Predictors and a remedy for noncompliance with amblyopia therapy in children measured with the occlusion dose monitor. Invest Ophthalmol Vis Sci. 2006;47(10):4393–4400. doi:10.1167/iovs.05-1428
31. Morjaria P, McCormick I, Gilbert C. Compliance and predictors of spectacle wear in schoolchildren and reasons for non-wear: a review of the literature. Ophthalmic Epidemiol. 2019;26(6):367–377. PMID: 31181970. doi:10.1080/09286586.2019.1628282
32. Kodjebacheva GD, Maliski S, Coleman AL. Use of eyeglasses among children in elementary school: perceptions, behaviors, and interventions discussed by parents, school nurses, and teachers during focus groups. Am J Health Promot. 2015;29(5):324–331. doi:10.4278/ajhp.120315-QUAL-140
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.