Back to Journals » Clinical Ophthalmology » Volume 16
Comparison of Refractive Outcomes in Small-Incision Lenticule Extraction Performed with One or Two Incisions
Authors Elsaadani IA , Hamed AM, Elshahat A, Heikal MA
Received 13 December 2021
Accepted for publication 16 January 2022
Published 5 February 2022 Volume 2022:16 Pages 281—291
DOI https://doi.org/10.2147/OPTH.S352341
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ibrahim Abdelkalek Elsaadani, Abdelmonem Mahmoud Hamed, Ahmed Elshahat, Mohamed Amin Heikal
Ophthalmology Department, Benha College of Medicine, Benha University, Benha, Qalyopia, Egypt
Correspondence: Abdelmonem Mahmoud Hamed
Ophthalmology Department, Benha College of Medicine, Benha University, Alansar Tower, Science of College St, Benha, Qalopia, Egypt
, Tel +201221640288
, Email [email protected]
Purpose: To retrospectively compare the refractive outcomes between two groups of small-incision lenticule extraction (SMILE), one with a single incision and the second one with dual-incisions.
Setting: Ebsar Eye Center, Benha, Qalyopia, Egypt.
Design: A retrospective cohort study.
Methods: This study was made up of two groups (162 eyes each): all eyes in group 1 had one SMILE cut at 120°, and all eyes in group 2 had double SMILE incisions, the first incision at 120° and the second one at 270°. Refractive outcomes between the two groups were compared at 3, 6, and 12 months after surgery.
Results: The mean preoperative refractive spherical equivalent (MRSE) was − 5.75 ± 2.59 D and − 6.38 ± 2.18 D in group 1 and 2, respectively (P = 0.73), and a cylinder of 1.25 ± 0.83 D and 0.75 ± 0.81 D, respectively (P = 0.85). At 12 months postoperatively, in group 1, 162 eyes (100%) achieved a UCVA of 20/25, 154 eyes (95.06%) achieved a UCVA of 20/20, and 110 eyes (67.90%) achieved 20/16. In group 2, 162 eyes (100%) achieved a UCVA of 20/25, 156 eyes (96.29%) achieved a UCVA of 20/20, and 113 eyes (69.75%) achieved 20/16. The mean MRSE at 12 months postoperatively was − 0.25 ± 0.33 D in group 1 and − 0.5 ± 0.33 D in group 2 (P = 0.62).
Conclusion: Dual-incision SMILE is safe and effective as single-incision SMILE, with a predictable and stable effect in correcting myopia and myopic astigmatism.
Keywords: ReSMILE, ReLEX, SMILE, SMILE technique, kerato-refractive, LASER vision correction, small incision lenticule extraction
Introduction
Small-incision lenticule extraction (SMILE) is one of the new techniques for the correction of myopia and myopic astigmatism. In SMILE, a corneal lenticule is made using a VisuMax® femtosecond laser (Carl Zeiss Meditec, Jena, Germany) and extracted through a single small corneal incision.1,2
The SMILE technique alleviates the possibility of flap-related intraoperative complications, including incomplete, irregular flaps, buttonholes, and free caps, as well as flap-related postoperative complications such as flap displacement, striae, and dislocation. Also, since the anterior lamellae remain intact including the Bowman’s membrane after SMILE, a less postoperative dry eye with SMILE had been reported in comparison to LASIK.2,3 This leads to higher surgeon confidence with the safety, stability, and efficacy of SMILE and higher patient satisfaction postoperatively.4,5
Epithelial ingrowth after SMILE within the corneal pocket interface has been reported in 0.5% of the patients,5 and pocket inflammatory cells in 0.3%.6 On the other hand, some surgeons prefer to irrigate the pocket to get rid of any debris at the end of SMILE surgery, and sometimes SMILE is combined with corneal collagen cross-linkage.7 Doing SMILE with two incisions8 instead of one should facilitate the irrigation of the SMILE pocket in most of the above-mentioned situations.
Methods
This is a single-center retrospective cohort study. The study adheres to the tenants of the declaration of Helsinki and was approved by the ethical committee of Benha University, Benha, Egypt (approval number Rc 7.7.2020). Informed consent was taken from all patients included in this study.
Data from 324 consecutive subjects who were seeking SMILE surgery in Ebsar Eye Center, Benha, Egypt, in the period between 1st of May 2018 to 31th of December 2019 was studied. All SMILE surgeries were performed by two surgeons (I.A.E, M.A.H). Each surgeon had an equal number of surgeries (162 eyes). Each subject underwent manifest and cycloplegic refraction, uncorrected and corrected distance visual acuity (UDVA and CDVA), slit-lamp biomicroscopy, and corneal topography (Pentacam HR Scheimpflug tomography, Oculus GmbH, Wetzlar, Germany).
Inclusion Criteria for the SMILE Surgeries
Female and male subjects 21 years or older with stable refraction for 1 year with spherical equivalent up to −10.0 D, contact lens discontinued for 1 week and rigid gas-permeable lens discontinued for 3 weeks before the surgery, the minimum thickness of the cornea was 510 μm at the thinnest location, and a residual corneal stromal thickness (bed) of at least 300 μm. Only patients who completed 12 months of follow-up visits were included in this study.
Exclusion Criteria for the SMILE Surgeries
Unstable refraction, active ocular disease like severe dry eyes, severe allergic eye disease, uveitis, visually significant cataract or retinal disease, family history of keratoconus, past history of systemic or autoimmune diseases, previous corneal surgery, or pregnant or nursing females.
Surgical Technique
All subjects were required to sign an informed consent before the SMILE surgery.
After the application of topical anaesthesia, standard sterile draping, and insertion of the speculum, the patient’s eye was centred and the cornea was docked with a small size curved interface cone. The surgeon pressed-on the joystick button for automatic suction, then the foot pedal was pressed on to activate the femtosecond laser (VisuMax®; Carl Zeiss Meditec, Jena, Germany) to create the lenticule and incisions.
The repetition rate of femtosecond laser ultra-short pulses was 500 kHz with a pulse energy of 125 nJ, which is focused at an accurate depth in the cornea. Initially, it cuts the lenticule posterior surface. This is followed by the lenticule side cut, then the lenticule anterior surface is created. Finally, in group one, a 3.0 mm side-cut incision is created and centred at 120°. In group two, dual side-cut incisions are produced; a primary main incision of 3.0 mm created at 120°, and a secondary incision (3.0 mm) created at 270°, in order to be positioned at the most lower location of the corneal pocket for better drainage of the fluidics (Figure 1) (Dr Abdelmonem Hamed technique).8
 |
Figure 1 SMILE with double incisions, the main incision at 120°, and the second incision at 270°. |
The ReSMILE push-up technique9,10 was then utilized to identify the lenticule edge; where an instrument with a Y-shaped tip; Bechert Nucleus Rotator (STORZ® ophthalmic instrument, Product Number: E4937) was inserted through the small incision, which thus caught the edge of the lenticule between its two limbs. The caught edge of the lenticule is then pushed up from its bed so that it was easily recognizable in the pocket, the lenticule was then extracted after dissection. The following parameters had fixed for all SMILE procedures: cap thickness was 100 µm, anterior-plane (cap) cut diameter was 7.5 mm, and the lenticule optical zone was 6.5 mm. The target postoperative sphere was Plano.
Postoperative Evaluation
Patients have been instructed to instil Tobradex eye drops (tobramycin and dexamethasone; Alcon Laboratories, Inc., Fort Worth, TX, USA) five times daily for 7 days. The follow-up regimen was at 1 day, and 1, 3, 6, and 12 months after the surgery. All visits of follow-up included manifest refraction, measurements uncorrected distance visual acuity (UDVA), and corrected distance visual acuity (CDVA), as well as examination by the slit-lamp, and corneal topography by Pentacam.
Statistical Analysis
Outcome analysis was performed according to the standard graphs for reporting refractive surgery.11 The outcomes were analysed. Data from the 12-month visit were used for analysis. Student’s unpaired t-test was used to calculate the statistical significance. Microsoft Excel master sheet 2010 (Microsoft Corporation, Redmond, WA, USA) was used for data entry and statistical analysis. A P-value of less than 0.05 was defined as statistically significant.
Results
This study included 162 eyes in each group. The average age of the patients in group 1 was 46.65 ± 11.58 years, with a range of 25–53 years. However, in group 2 it was 41.84 ± 10.36 years, with a range of 23–49 years. Table 1 demonstrates the demographic and refractive data for the studied population in both groups. The mean preoperative refractive spherical equivalent (MRSE) was −5.75 ± 2.59 D and −6.38 ± 2.18 D in group 1 and 2, respectively, and a cylinder of 1.25 ±0.83 D and 0.75±0.81 D, respectively. There is a statistically non-significant difference between the studied groups regarding preoperative MRSE (P = 0.73), and manifest cylinder (P = 0.85).
 |
Table 1 Preoperative Demographic and Refractive Characteristics of the Included Patients |
Efficacy
At 1 year postoperatively, in group 1, 162 eyes (100%) accomplished a UCVA of 20/25, 154 eyes (95.06%) achieved a UCVA of 20/20, and 110 eyes (67.90%) accomplished 20/16. In group 2, 162 eyes (100%) accomplished a UCVA of 20/25, 156 eyes (96.29%) accomplished a UCVA of 20/20, and 113 eyes (69.75%) accomplished 20/16. Figure 2 demonstrates cumulative percentages of eyes where target refraction was zero getting particular levels of uncorrected distance visual acuity (UDVA) 1 year after SMILE.
 |
Figure 2 Distribution of uncorrected distance visual acuity in both groups. |
Figure 3 demonstrates the difference between postoperative UDVA and preoperative corrected distance visual acuity (CDVA), in group 1, where 80.0% of the eyes gained UCDV within 1 line of CDVA, and 95% of the eyes gained UCDV within 2 lines of CDVA. In group 2, 81.17% of the eyes gained UDVA within 1 line of CDVA, and 97.17% of the eyes gained UDVA within 2 lines of CDVA.
 |
Figure 3 Uncorrected distance visual acuity versus corrected distance visual acuity in both groups. |
Safety
The gain or loss of CDVA at one-year follow-up showed that 24.76% of the eyes in group 1 versus 17.28% in group 2 gained one line (P=0.07), and 2.86% of the eyes in group 1 versus 7.41% in group 2 gained 2 lines (P=0.08). While 63.81% in group 1 showed no change in CDVA while 72.22% in group 2 showed no change in CDVA. 5.56% in group 1 showed a loss of 1 line of CDVA while 3.09% in group 2 showed a loss of 1 line of CDVA (P = 0.92) (Figure 4).
 |
Figure 4 Changes in corrected distance visual acuity in both groups. |
Predictability
Figure 5 shows the scatter plot analysis comparing attempted and achieved spherical equivalent refraction in group 1 and group 2, respectively. The grade of definition between the attempted and achieved MRSE was similar between group 1 (R2 = 0.97) and group 2 (R2 = 0.89) (P = 0.73). Both groups led to a predictable outcome, which was indicated by the higher R2.
 |
Figure 5 Achieved versus attempted spherical equivalent refraction in both groups. |
The accuracy and predictability of the residual manifest SE within ± 0.5D was 77.78% of eyes in group 1, and 77.77% in group 2 (P = 0.85, Figure 6).
 |
Figure 6 Spherical equivalent refraction accuracy in both groups. |
Stability
Figure 7 demonstrates the long-term stability in both groups between 3 and 12 months. Only 5.71% and 6.66% had a change greater than 0.5 D in groups 1 and 2, respectively (P= 0.8). However, the spherical equivalent had insignificant change from −0.5 ± 0.41 D at 3rd month to −0.25 ± 0.33 D at 12th month in group 1 and from −0.75 ± 0.40 D at 3rd month to −0.5 ± 0.33 D at 12th month in group 2 (P = 0.62). In each group, there is a significant decrease in the manifest sphere over time. However, the manifest sphere value did not change at 12 months from sixth month.
 |
Figure 7 Stability of spherical equivalent refraction in both groups. |
Astigmatism Analysis
Figure 8 shows refractive astigmatism at 12 months postoperatively where 80% of the eyes were ≤0.5 astigmatism dioptre, while 97.15% of the eyes were ≤1.0 astigmatism dioptre in group 1; however, 88.23% of the eyes were ≤0.5 astigmatism dioptre, while all eyes (100% of the eyes) were ≤1.0 astigmatism dioptre in group 2 (162 eyes) (P = 0.72).
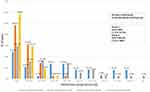 |
Figure 8 Refractive astigmatism in both groups. |
Discussion
With the growing demand for SMILE for people with refractive error, there is an increased requirement to wash the SMILE pocket, especially in cases with SMILE XTRA, intraoperative complications like incision bleeding that enter inside the SMILE pocket, and postoperative complications like epithelial ingrowth.12,13 If the epithelial cells are localized to the periphery and do not cause visual degradation, those can be left alone and may subsequently spontaneously subside. However, if the epithelial cells have encroached onto the center of the cornea or are causing significant astigmatism or visual acuity diminution, they require surgical scraping and removal. However, in some cases of recurrent epithelial ingrowth, the SMILE cap may be converted into a flap to be able to effectively get rid of the epithelial. Recently, some refractive surgeons started creating SMILE with dual incisions in all cases, to allow draining the fluidics throughout the incision located at 270°.8 Thus, the stromal pocket is no longer a closed space and the hydraulic current can get rid of the scrapped epithelial cells and pump them out through the draining incision instead of being trapped inside the closed space of the stromal pocket. The same thing happens when we irrigate the SMILE pocket in cases with intraoperative bleeding, SMILE XTRA (SMILE with corneal collagen cross-linkage) to wash out the Riboflavin, or with postoperative complications like inflammation.
Major previous research studies on the large number of patients receiving SMILE are summarized in Table 2.1,4,6,8,16–20 Our findings were compared, or slightly better than those in previous studies on safety and efficacy.
 |
Table 2 Previous Studies on Refractive Outcomes in a Cohort of Patients Undergoing SMILE |
In this study, we could not find a statistically significant difference between the two groups in terms of change in UDVA, SE, or refractive astigmatism, indicating that the second SMILE incision did not affect refractive outcomes. Hence, we encourage using the dual-incisions SMILE technique (double SMILE) as a potentially valuable alternative to the ordinary SMILE technique. We think that, adding the second incision to ordinary SMILE will simplify management of intraoperative and postoperative complications, like intraoperative bleeding inside the SMILE pocket and SMILE XTRA, and postoperative complications like epithelial ingrowth, and inflammatory infiltrates,7,14,15 thus saving money to buy a license (circle license) to convert the cap into a flap. The limitation of this study is the small number of eyes in each group. So, more detailed research studies with a bigger number of eyes are required to evaluate the dual-incision SMILE technique and to get out its advantages and disadvantages to light.
Disclosure
The authors did not receive any financial support from any public or private sources. The authors have no financial or proprietary interest in a product, method, or material described herein.
References
1. Sekundo W, Kunert KS, Blum M. Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study. Br J Ophthalmol. 2011;95(3):335–339. doi:10.1136/bjo.2009.174284
2. Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: all-in-one. femtosecond laser refractive surgery. J Cataract Refract Surg. 2011;37(1):127–137. doi:10.1016/j.jcrs.2010.07.033
3. Wang Y, Wu Z, Tang X, et al. Two-millimeter micro-incision lenticule extraction surgery with minimal invasion: a preliminary clinical report. Zhonghua Yan Ke Za Zhi. 2014;50(9):671–680.
4. Vestergaard A, Ivarsen AR, Asp S, Hjortdal JØ. Small-incision lenticule extraction for moderate to high myopia: predictability, safety, and patient satisfaction. J Cataract Refract Surg. 2012;38(11):2003–2010. doi:10.1016/j.jcrs.2012.07.021
5. Moshirfar M, McCaughey MV, Reinstein DZ, Shah R, Santiago-Caban L, Fenzl CR. Small incision lenticule extraction. J Cataract Refract Surg. 2015;41(3):652–665. doi:10.1016/j.jcrs.2015.02.006
6. Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision. Lenticule extraction procedures. Ophthalmology. 2014;121:822–828. doi:10.1016/j.ophtha.2013.11.006
7. Graue-Hernandez EO, Pagano GL, Garcia-de la Rosa G, et al. Combined small-incision lenticule extraction and intrastromal corneal collagen crosslinking to treat mild keratoconus: long-term follow-up. J Cataract Refract Surg. 2015;41(11):2524–2532. doi:10.1016/j.jcrs.2015.06.027
8. Abdelwahab S, Hamed A, Elshahat A, Rashad S, Elfauyomi M. Outcomes of small incision lenticule extraction with dual-incisions in myopic patients. Clin Ophthalmol. 2020;14:3067–3074. doi:10.2147/OPTH.S270032
9. Hamed A, Fekry A. Refractive small incision lenticule extraction: push-up and pushdown techniques. J Cataract Refract Surg. 2016;42:1713–1715. doi:10.1016/j.jcrs.2016.11.003
10. Hamed AM, Abdelwahab SM, Soliman TT. Intraoperative complications of refractive small incision lenticule extraction in the early learning curve. Clin Ophthalmol. 2018;12:665–668. doi:10.2147/OPTH.S157356
11. Reinstein DZ, Archer TJ, Randleman JB. JRS standard for reporting astigmatism outcomes of refractive surgery. J Refract Surg. 2014;30(10):654–659. doi:10.3928/1081597X-20140903-01
12. Hamed AM, Heikal MA, Soliman TT, Daifalla A, Said Ahmed KE. SMILE intraoperative complications: incidence and management. Int J Ophthalmol. 2019;12(2):280–283. doi:10.18240/ijo.2019.02.15
13. Wang Y, Ma J, Zhang J, et al. Incidence and management of intraoperative complications during small-incision lenticule extraction in 3004 cases. J Cataract Refract Surg. 2017;43(6):796–802. doi:10.1016/j.jcrs.2017.03.039
14. Osman IM, Helaly HA, Abou Shousha M, AbouSamra A, Ahmed I. Corneal safety and stability in cases of small incision lenticule extraction with collagen cross-linking (SMILE Xtra). J Ophthalmol. 2019;2019:1–10. doi:10.1155/2019/6808062
15. Ganesh S, Brar S. Clinical outcomes of small incision lenticule extraction with accelerated cross-linking (ReLEx SMILE Xtra) in patients with thin corneas and borderline topography. J Ophthalmol. 2015;2015:263412. doi:10.1155/2015/263412
16. Hjortdal JØ, Vestergaard AH, Ivarsen A, Ragunathan S, Asp S. Predictors for the outcome of small-incision lenticule extraction for myopia. J Refract Surg. 2012;28:865–871.13. doi:10.3928/1081597X-20121115-01
17. Reinstein DZ, Carp GI, Archer TJ, Gobbe M. Outcomes of small incision lenticule extraction (SMILE) in low myopia. J Refract Surg. 2014;30:812–818.14. doi:10.3928/1081597X-20141113-07
18. Pedersen IB, Ivarsen A, Hjortdal J. Tree-year results of small incision lenticule extraction for high myopia: refractive outcomes and aberrations. J Refract Surg. 2015;31:719–724.15. doi:10.3928/1081597X-20150923-11
19. Hansen RS, Lyhne N, Grauslund J, Vestergaard AH. Small-incision lenticule extraction (SMILE): outcomes of 722 eyes treated for myopia and myopic astigmatism. Graefes Arch Clin Exp Ophthalmol. 2016;254:399–405.16. doi:10.1007/s00417-015-3226-5
20. Elmassry A, Ibrahim O, Osman I, et al. Long-term refractive outcome of small incision lenticule extraction in very high myopia. Cornea. 2020;39(6):669–673. doi:10.1097/ICO.0000000000002288
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
