Back to Journals » Research and Reports in Urology » Volume 12
Comparison Between Processus Vaginalis Sac Tightening Technique and the Conventional Technique in Orchiopexy Surgery Over 10 Years
Authors Shirazi M, Safavi S, Makarem A , Malekmakan L
Received 14 November 2019
Accepted for publication 9 March 2020
Published 18 March 2020 Volume 2020:12 Pages 129—136
DOI https://doi.org/10.2147/RRU.S237824
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Mehdi Shirazi,1,2 Salar Safavi,1,3 Alireza Makarem,1 Leila Malekmakan3
1Department of Urology, Shiraz University of Medical Sciences, Shiraz, Iran; 2Histomorphometry and Stereology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran; 3Shiraz Nephro-Urology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
Correspondence: Salar Safavi
Department of Urology, Shiraz University of Medical Sciences, Shiraz, Iran
Tel/Fax +98-713-2326645
Email [email protected]
Background: Undescended testis (UDT) is a common congenital urogenital anomaly that is treated by orchiopexy. We aimed to introduce patent processus vaginalis (PPV) sac tightening (PVST) technique and compare it to the conventional technique.
Methods: We retrospectively studied all the operated UDT patients during 10 years. In the conventional technique, it was necessary to ligate PPV sac after being peeled off from the spermatic cord. PVST was dissected longitudinally from the two sides of where the PPV sac wall was attached to the spermatic cord till the proximal part, and only a narrow thin layer sticking to the spermatic cord was left and the proximal PVV sac opening was tightened as much as possible with vicryl suture at the internal inguinal ring level. The significance level was < 0.05.
Results: Of 821 orchiopexy (mean age 24.5± 24.2 months), 36.3% were done by conventional and 63.7% by PVST technique. Hematoma, edema, hydrocele, and wound infection were lower in the PVST technique, but it was not significant (p> 0.05). Testicular atrophy and operation time were significantly lower in the PVST than the conventional technique (p< 0.001).
Conclusion: The orchiopexy PVST technique has lower complications and seems to be easier, faster and safer than the conventional technique.
Keywords: UDT, orchiopexy, testis atrophy, hernia, PVST technique
Introduction
Cryptorchidism or undescended testis (UDT) is one of the most common congenital anomalies of the genitalia and endocrine system in male children1–4 that is the third most common urogenital abnormality affecting primary school children in Iran.4 Its prevalence is 3.4% to 5.8% in the newborn term and up to 30% in preterm infants, reducing to 0.8% at one year of age and remaining approximately at the same rate until puberty. The prevalence was reversely associated with increased gestational age in preterm and increased age in term infants.1,3-7
Since UDT increases the risk of malignancy and infertility and the affected person is more vulnerable to trauma, orchiopexy surgery is treatment of choice through various laparoscopy or open surgical techniques.1,2,8,9 These techniques have undergone different modifications during recent years to minimize intra and post-operative complications including hernia, testicular atrophy, hydrocele, hematoma, and infection.10
For preventing postoperative hernia, in the conventional as the standard technique, it is necessary to ligate the patent processus vaginalis (PPV) sac in the proximal part after being peeled off from other components of the spermatic cord;7,8 this increases the risk of subsequent damage to the spermatic cord superfine vessels, vas deferens, and secondary testicular atrophy.10–12 To prevent this problem, some studies have suggested that the proximal area should be left unligated after peeling the PPV sac off the cord.1,12,13 However, this method may result in inguinal hernia in the first postoperative days when the PPV sac peritonealization is being completed.14
Given the importance of preventing the aforementioned complications caused by the techniques detailed above, we designed this study to introduce a new technique as PPV sac tightening (PVST), in which the PPV sac opening in the proximal part is tightened at the internal inguinal ring level instead of being peeled off and ligated. We aimed to compare the intra- and post-operative complications in the conventional and new techniques.
Patients and Methods
This retrospective study was conducted in Namazi and Shahid-Faghihi hospitals during 2007 to 2016. Our sample included all UDT patients who underwent non-urgent and elective open orchiopexy surgery using standard conventional and new technique by a single surgeon who also served as the senior pediatric urologist during the ten past years. In this study, we excluded the patients with very short spermatic cord, testicular and spermatic cord torsion, other serious congenital disorders, nubbin or absent testis, history of previous urologic surgery, incomplete follow up post-operation and medical records information. The remaining patients were divided into two groups: ligation group as the conventional technique and tightening group as the new technique.
Data Collection
To collect the required data, we prepared a form with three sections. The first section addressed the basic information; age at the time of operation, history of previous surgery, and date of operation. The second section included information about the testis location (based on the post-anesthesia induction exam and before starting the procedure), surgery time (defined as the time from skin incision till skin closure), the operation side, the type of orchiopexy surgery (scrotal, inguinal, abdominal exploration), and intraoperative complications (PPV sac tearing, the vas deferens damage, and damage to the spermatic cord superfine vessels). The third section included information about the postoperative complications: hematoma, edema, wound infections, testicular atrophy, reascendance of testis, hernia, and hydrocele in the one, six and twelve-month follow up visits.
Testicular atrophy has been defined as 25% decrease in the volume of the operated testis (measured in pre-operation visit and post-operation follow up visits by orchidometer) compared to the contralateral normally descended testis. Therefore, the patients with bilateral undescended testes were excluded from the final analysis.15,16 The above data were extracted from the patients’ medical records such as operation report sheets and their medical cases recorded in the hospital and clinic before and after the operation. Incomplete information was supplemented through phone calls with the patients’ parents.
Surgical Technique (Figures 1–4)
The patients underwent surgery using the conventional orchiopexy technique from 2007 to 2010 and then using our new technique (PVST). After general anesthesia induction, palpability and testis site were checked and the orchiopexy was done through inguinal or scrotal incision based on the preoperative examination. Orchiectomy was performed for nubbin testes. Figure 1 shows the schematic cross-section view of the spermatic cord and PPV sac in PVST technique.
 |
Figure 1 Schematic cross-section view of the spermatic cord and PPV sac in PVST technique. |
 |
Figure 2 PPV sac proximal opening with a narrow thin layer of sac wall left on the spermatic cord after dissection in PVST technique. |
 |
Figure 3 Closed PPV sac opening by PVST technique. |
 |
Figure 4 PVST technique steps. |
Conventional Technique (Ligation Group)
Upon the localization of the testis and spermatic cord, after cutting the gubernaculum, these structures were released from the inguinal canal walls. Then, the tunica vaginalis was dissected and the patent processus vaginalis sac was carefully peeled off from the vas deferens and the spermatic cord superfine vessels up to the level of internal inguinal ring, and at this level it was clamped. Afterwards, the PPV sac was cut distal to the clamp and its proximal part was twisted and ligated with vicryl suture.
PVST Technique (Tightening Group)
For preventing any possible damages to the spermatic cord superfine vessels and vas deferens and also preventing the tearing of patent processus vaginalis sac with a very thin wall, in this technique after cutting the gubernaculum and opening of the PV, the testis was delivered, PV was incised till the closest edge of the spermatic cord structures, and then PV sac was dissected longitudinally from the sides till the proximal part and only a narrow thin layer sticking to the spermatic cord was left (Figure 2). Then, the proximal opening of the PPV sac was tightened to the possible extent, using the vicryl suture 4–0 at the internal inguinal ring level without removing the sticking layer on the spermatic cord and its fine structures (Figure 3). To evaluate the tightening adequacy for preventing the subsequent inguinal hernia development, a pressure on the lower abdominal part was applied and if any abdominal fluid leakage was seen from the tightened proximal opening of the PPV sac, the tightening level would be increased till no leakage was seen by this maneuver. In the scrotal orchiopexy procedure which was performed on the lower lying undescended testes, through a scrotal incision of the testis, the spermatic cord, and the PPV sac were pulled out of the external inguinal ring by applying sufficient traction force and the mentioned procedures and techniques were done on the PPV sac. Then, the traction force was released and the structures were retracted back into the canal. The next steps of the testicular lowering procedure and fixing it to the scrotal wall were common among all types of techniques detailed above and similar to the standard technique. Steps of PVST technique is presented in Figure 4.
Statistical Analysis
The collected data were analyzed using SPSS Software (Version 18). The qualitative data were expressed in number and percentage and analyzed through the Chi-square test. The quantitative data were expressed as the mean and standard deviation and analyzed using t-test. The significance level was considered less than 0.05.
Results
The participants in this study were 643 boys aged 6 months to 12 years with the mean age of 24.5±24.2 months who underwent surgery with the primary diagnosis (impression) of UDT. With regard to the fact that 225 of all patients suffered bilateral UDT, a total number of 868 operated testes were reviewed in this study. Of the total number of testicles under analysis, 450 testicles (51.8%) were bilateral UDT, and of unilateral ones 196 (22.6%) were at the right side and 222 (25.6%) were at the left side. Besides, 679 testicles (78.2%) were palpable after induction of anesthesia, of which 39 (4.5%) were diagnosed as nubbin and underwent orchiectomy. No testicle was found after inguinal and abdominal exploration in 8(0.9%) cases.
Of 868 operated testes, 202 (23.2%) were scrotal orchiopexy, 524 (60.3%) inguinal orchiopexy, 95 (11.4%) abdominal exploration and orchiopexy, and 39 (4.5%) orchiectomy of nubbin testis.
After excluding orchiectomy cases and those with absent testis, a total number of 821 cases were assessed in the study. In addition, 298 (36.3%) patients underwent surgery using the conventional technique (ligation group) and 523 (63.7%) patients by the PVST technique (tightening group).
Table 1 shows the comparison of the two groups in terms of postoperative complications and different pre-operation testis positions and surgical approaches. As can be seen, reascending and hernia were not observed in either group. In addition, there were no significant differences between the groups in terms of the postoperative complications, except for testicular atrophy (p>0.05).
 |
Table 1 Comparison of the Two Groups in Terms of Postoperative Complications, Different Pre-Operation Testis Positions and Surgical Approaches |
In order to assess the testicular atrophy as the most important postoperative complication, due to the necessity of comparing the affected operated testis size with the normally descended opposite one, the patients with orchiopexy for bilateral UDT were excluded from the final analysis. Postoperative testicular atrophy occurred significantly more in the conventional than PVST technique: 7 (2.3%) cases compared to 2 (0.4%) cases, respectively (p=0.030). No significant difference in post-operation complications was seen between different pre-operation testes positions and surgical approaches (scrotal, inguinal, abdominal) in both groups. The mean operation time was 22.8±3.5 mins in the conventional and 17.8±2.8 mins in the PVST group (p=0.001). In Table 2, the mean age of patients with and without post-operative complications is presented in both groups. The number of patients operated by each technique and surgical approaches, also laterality and palpability of them are presented in Table 3.
 |
Table 2 The Mean Age of the Patients with and Without Post-Operative Complications in Both Groups |
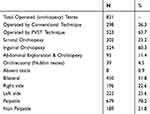 |
Table 3 The Number of Operated Testes in Each Group and Their Laterality and Palpability |
Discussion
In the standard orchiopexy, peeling off the PPV sac from other subtle structures of the spermatic cord, cutting and ligation of its most proximal part to prevent a hernia is recommended as a necessary step of this procedure.7,8 However, it seems that there is a risk of spermatic cord damage (its vessels and vas deferens), especially at lower ages that may result in delayed secondary testicular atrophy.10,12 There is another risk of tearing and retracting of PPV sac wall that increases the surgery time for repairing.1
Therefore, in order to prevent these complications, some studies have proposed the san ligation technique in which the proximal part of the PPV sac is left unligated after the PPV sac is peeled off the spermatic cord.1,12,13 Many researchers who have proposed san ligation technique believed that the metamorphosis of the mesodermal cells leads to peritonealization of the PPV sac opening. However, it should be noted that the peritoneal repair of the defect in the PPV sac opening starts after 48 hrs and takes 2–3 weeks to be completed.14 Nevertheless, during the mentioned period, especially within the first 48 hrs, one cannot be assured of the non-development of a hernia through the PPV sac opening;1,12,13 there are some reports on the risk of the occurrence of a postoperative hernia if the sac opening is left open. Even in one reported case, the incarcerated hernia led to the intestinal resection during a few days after the operation.6,17 Given the potential risk of development of the postoperative hernia in the cases in whom the PPV sac opening is not closed and considering the pathology of the peritoneal repair, the duration of spontaneous closure of its defect and the reports related to cases with post-operation hernia development, especially when the PPV sac has a wide opening and the defect is large, the san ligation technique cannot be recommended with full confidence.
The mean age of our patients was close to the age recommended for surgery in the related studies (under 1–2 years),6 and the patients who underwent surgery at a higher age were those who had delayed diagnosis and referral from the primary medical centers.
To prevent the complications associated with both ligation and san ligation techniques, we suggest PVST technique in which the PPV sac is dissected longitudinally from the two sides of where the PPV sac wall is attached to the spermatic cord till the proximal part, and the proximal PPV sac is tightened to the possible extent. This can somehow prevent the possible damages made to the subtle structures of the spermatic cord as the result of peeling off the PPV sac from the spermatic cord and ligation of its proximal opening in the conventional standard techniques. However, the PVST technique closes the PPV sac opening and prevents the incidence of a secondary hernia. Thus, to ensure the safety of our technique, we compared the postoperative complications among the patients who had undergone surgery using the conventional ligation as the standard technique and the proposed tightening technique during ten years.
Testicular reascending, as a postoperative complication, was not seen in our both groups; it was predictable because in both surgical techniques we fixed the testis to the scrotal wall.1,6,8 Another post-operative complication that could potentially occur in the case of the non-closure of the PPV sac opening was a secondary hernia. However, it was not seen in the two groups due to the closure of the PPV sac opening in both, that was the same as the results in other studies.1,8 The occurrence rate of the other postoperative complications including hydrocele, hematoma, edema, and infection of operation site was lower in the new technique. However, this difference was not significant and it was the same in previous studies.1,10 The current results showed that testicular atrophy in the conventional group was similar to the previous studies.8,16,18 However, its rate was significantly lower in our PVST technique, so it may confirm our hypothesis about the safety of the tightening technique that may prevent possible damages to the subtle structures of the spermatic cord, especially its superfine vessels. There was no significant difference between the mean age of the patients with post-operative complications in both groups.
Duration of PVST surgery, as a new technique, was significantly shorter than the conventional technique. Given the ease of implementing the introduced technique compared to the standard technique and the elimination of the time-consuming nature of the operation for the complete peeling off the PPV sac from the spermatic cord, it seems that the use of the proposed technique may reduce the operation time compared to the conventional technique.
Altogether, the proposed PVST technique is easier to perform compared to the conventional sac ligation technique; if its safety is confirmed in the subsequent prospective studies, it will appear to have a lower learning curve than the standard technique and it can be used easily even by inexperienced general urologists with no considerable complications.
Limitation
This is a retrospective study, so it was impossible to find some complications such as tearing the PPV sac wall or damage to the spermatic cord superfine vessels. Also, duo to shortcomings of the study, we lacked data on the follow-up postoperative visits in some cases. Also, Marcaine was administered in the surgery site as the local anesthesia to reduce pain, and pain could not be examined.
Conclusion
Based on this study results, it seems that PVST technique in comparison to the standard orchiopexy technique is safer with lower complications and also easier and faster to do, so this technique is recommended if prospective studies confirm these results.
Ethical Approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the local ethics committee of Shiraz University of Medical Sciences (IR.sums.med.rec.1397.117) on June 2, 2018 written informed consent was obtained from a parent for each of the participants.
Acknowledgment
The authors would like to thank Dr Nasrin Shokrpour for the editorial assistance in the Research Consulting Center (RCC) of Shiraz University of Medical Science and improvement of the use of English in the manuscript and Afsaneh Ghasemi for helping to extract data.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the final version to be published, and agreed to be accountable for all aspects of the work.
Funding
The Vice-Chancellery of Research and Technology of Shiraz University of Medical Sciences, Shiraz, Iran financially supported this study (grants No 15600) that was extracted from the thesis of Salar Safavi M.D.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Salimi A, Shahmoradi S, Nia SR, Eftekhari SS. Beneficial impression of san-ligation over high-ligation during orchidopexy; a cross-sectional of 2659 patients. Int J Pediat Mashhad. 2017;5(6):5145–5152.
2. Dayanc M, Kibar Y, Irkilata HC, Demir E, Tahmaz L, Peker AF. Long-term outcome of scrotal incision orchiopexy for undescended testis. Urology. 2007;70(4):
3. Khazaeli M, Khazaeli D, Mombeini H, Asadinia P, Bahadoram M. Laparoscopic two stage fowler-stephens orchiopexy: a single center experience. Persian J Med Sci. 2016;3(1):137–141.
4. Yegane RA, Kheirollahi AR, Bashashati M, Rezaei N, Tarrahi MJ, Khoshdel JA. The prevalence of penoscrotal abnormalities and inguinal hernia in elementary-school boys in the west of Iran. Int J Urol. 2005;12(5):479–483. doi:10.1111/j.1442-2042.2005.01071.x
5. Sijstermans K, Hack WW, Meijer RW, van der Voort-doedens LM. The frequency of undescended testis from birth to adulthood: a review. Int J Androl. 2008;31(1):1–11. doi:10.1111/j.1365-2605.2007.00770.x
6. Al-Mandil M, Khoury AE, El-Hout Y, Kogon M, Dave S, Farhat WA. Potential complications with the prescrotal approach for the palpable undescended testis? A comparison of single prescrotal incision to the traditional inguinal approach. J Urol. 2008;180(2):686–689. doi:10.1016/j.juro.2008.04.040
7. Thorup J, Haugen S, Kollin C, et al. Surgical treatment of undescended testes. Acta Paediatr. 2007;96(5):631–637. doi:10.1111/j.1651-2227.2007.00239.x
8. Ceccanti S, Zani A, Mele E, Cozzi DA. Orchidopexy without ligation of the processus vaginalis is not associated with an increased risk of inguinal hernia. Hernia. 2014;18(3):339–342. doi:10.1007/s10029-013-1114-7
9. Guo J, Liang Z, Zhang H, et al. Laparoscopic versus open orchiopexy for non-palpable undescended testes in children: a systemic review and meta-analysis. Pediatr Surg Int. 2011;27(9):943–952. doi:10.1007/s00383-011-2889-1
10. Tabrizian F, Raisolsadat SMA, Houshmand B, Yaghubi MA. Assessment of the necessity of sac high ligation in inguinal hernia open surgery among children. J Pediat Surg. 2013;48:547–549. doi:10.1016/j.jpedsurg.2012.08.003
11. Taneja SS. Complications of Urologic Surgery: Prevention & Management.
12. Jain VK, Singh S, Garge S, Joshi M, Sanghvi J. Orchidopexy san ligation technique of orchidopexy. Afr J Paediatr Surg. 2011;8(1):112–114. doi:10.4103/0189-6725.79073
13. Mahomed A, Dunckley MG. Spontaneous peritoneal closure after orchidopexy in children: comment to: orchidopexy without ligation of the processus vaginalis is not associated with an increased risk of inguinal hernia. Ceccanti S, Zani A, Mele E and Cozzi DA (2013). Hernia. 2014;18(3):343–344. doi:10.1007/s10029-013-1160-1
14. Hubbard TB
15. Mohta A, Jain N, Irniraya KP, Saluja SS, Sharma S, Gupta A. Non-ligation of the hernial sac during herniotomy: a prospective study. Pediatr Surg Int. 2003;19(6):451–452. doi:10.1007/s00383-002-0940-y
16. Durell J, Johal N, Burge D, et al. Testicular atrophy following paediatric primary orchidopexy: a prospective study. J Pediatr Urol. 2016;12(4):243 e1–4. doi:10.1016/j.jpurol.2016.05.023
17. Metwalli AR, Cheng EY. Inguinal hernia after laparoscopic orchiopexy. J Urol. 2002;168(5):2163. doi:10.1016/S0022-5347(05)64343-1
18. Ein SH, Nasr A, Wales PW, Ein A. Testicular atrophy after attempted pediatric orchidopexy for true undescended testis. J Pediatr Surg. 2014;49(2):317–322. doi:10.1016/j.jpedsurg.2013.11.048
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
