Back to Journals » Clinical Ophthalmology » Volume 13
Comparing the long-term impact on health care resources utilization and costs due to various single-piece acrylic monofocal intraocular lens implantation during cataract surgery: a cost-consequence analysis for the United Kingdom, Italy, and Denmark
Authors Dhariwal M , Bouchet C, Jawla S
Received 13 October 2018
Accepted for publication 13 December 2018
Published 14 January 2019 Volume 2019:13 Pages 169—176
DOI https://doi.org/10.2147/OPTH.S190754
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mukesh Dhariwal,1 Christine Bouchet,2 Shantanu Jawla3
1Global Health Economics & Outcomes Research, Alcon Laboratories, Inc., Fort Worth, TX, USA; 2Global Patient Access, Novartis Pharma AG, Basel, Switzerland; 3Patient Access Services, Novartis Healthcare Private Limited, Hyderabad, India
Purpose: The objective of this study was to estimate the cost impact of neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy and its complications due to single-piece acrylic monofocal intraocular lenses (IOLs) in the healthcare setting of United Kingdom, Italy, and Denmark.
Materials and methods: A hypothetical cost-consequence model was developed to estimate economic burden of Nd:YAG laser capsulotomy due to different single-piece acrylic monofocal IOLs. Cumulative incidence of Nd:YAG laser capsulotomy at 3 years after cataract surgery with five single-piece monofocal acrylic IOLs was sourced from retrospective data analysis of electronic medical records of cataract patients in the United Kingdom. Risk probability of post-Nd:YAG laser complications, ie, retinal detachment, glaucoma, and cystoid macular edema at 3 years was derived using published literature. Unit costs were taken from publicly available sources with all costs converted to euro (€). Number of cataract procedures per year for each country was sourced from Eurostat statistics.
Results: For the estimated cataract procedures carried out nationally every year, single-piece monofocal hydrophobic AcrySof IOL was associated with substantially lower cases of Nd:YAG laser capsulotomy procedures and subsequent complications in 3 years after cataract surgery when compared to other single-piece monofocal acrylic IOLs. The total cost savings with the use of AcrySof over other IOLs in countries assessed ranged from €0.5 to €4.7 million (vs AMO Tecnis) and €2.1 to €17.9 million (vs Rayner C-/Super-flex).
Conclusion: Incidence of Nd:YAG capsulotomy due to the choice of IOL could significantly affect healthcare budgets in the post-cataract surgery period. Our analysis indicates that single-piece monofocal AcrySof IOLs is the most cost-saving treatment option for health care systems when compared to other acrylic single-piece IOLs.
Keywords: AcrySof, cost, Nd:YAG capsulotomy, cataract, PCO, IOL
Introduction
Cataract surgery is one of the most common surgical procedures performed globally with reported rates of 4,000–10,000 per million in developed countries to 500–2,000 per million in developing countries.1 Posterior capsule opacification (PCO) is the most common postsurgical complication of cataract surgery which can present several months to years after surgery.2 PCO reduces patients’ visual acuity, impairs contrast sensitivity, and increases glare disability. PCO is usually treated by neodymium-doped yttrium aluminum garnet laser (Nd:YAG) capsulotomy.3 This procedure is generally considered safe but could occasionally lead to complications such as retinal detachment (RD), glaucoma, cystoid macular edema (CME), intraocular lens (IOL) pitting, iritis, and uveitis,4–8 which can further impact patients’ visual function and vision-related quality of life.
The incidence rates of PCO have been reported to vary from 11% to 43% within the first year of surgery and from 23% to 38% within 2–4 years after cataract surgery.9–11 Higher incidence of PCO after cataract surgery increases health care resource utilization and costs.2 According to the Centre for Medicare Services (CMS) data for year 2010, estimated costs for Nd:YAG laser capsulotomy accounted for $187 million in the CMS population.12 Further, costs of PCO are not limited to the cost of performing Nd:YAG capsulotomy but also include the cost of managing its complications. Health care consumption due to these complications include consultations and examinations and may also result in additional surgical procedures for treatment.2 A retrospective study conducted in France estimated the indirect costs associated with the risk of blindness due to Nd:YAG capsulotomy complications particularly glaucoma and persistent elevation of intraocular pressure to be 21% of the total costs of Nd:YAG laser capsulotomy and management of its complications.2 These data imply that Nd:YAG capsulotomy not only increases the clinical burden but also poses a significant economic burden on patients, caregivers, and third-party payers.
Risk factor for PCOs include age, surgical technique, ocular comorbid diseases but the most important one is IOL material and design.13,14 Many published studies have reported significantly lower incidence of Nd:YAG capsulotomy in patients implanted with hydrophobic IOLs during cataract surgery compared to patients implanted with silicone and hydrophilic acrylic IOLs.15–20 AcrySof IOLs (Alcon Laboratories, Inc.) are made from a hydrophobic acrylic material with higher fibronectin bioadhesion properties and a sharp optic edge.21 Recently, a real-world evidence study evaluated the long-term incidence of Nd:YAG laser capsulotomy and PCO following age-related cataract surgery, comparing 3-year outcomes for hydrophobic acrylic AcrySof IOLs vs cohorts of other hydrophilic and hydrophobic acrylic monofocal IOLs.22 Published results from this study suggested that AcrySof IOLs are associated with significantly lower incidence of Nd:YAG laser capsulotomy compared to other hydrophilic and hydrophobic acrylic IOLs. The aim of the present study was therefore to estimate the cost impact of Nd:YAG capsulotomy due to the use of different single-piece monofocal acrylic IOLs.
Materials and methods
A cost-consequence model was developed in Microsoft Excel to estimate the health care resource utilization and cost impact of Nd:YAG capsulotomy due to different single-piece monofocal acrylic IOLs – AcrySof, AMO Tecnis, B&L Akreos, Lenstec Softec, and Rayner C-/Super-flex. The model was developed per guidance from the National Institute for Health and Care Excellence on Medical Technologies Evaluation Programme methods.23 The economic perspective adopted in the study was that of the national health care system of the United Kingdom, Italy, and Denmark. These selected countries largely have similar single national payer health care systems and the geographical spread provides a broad picture of European Union.
Patient population
Patients undergoing cataract surgery were assessed for the current economic evaluation. The data for the annualized cataract surgeries for each country were taken from the Eurostat and were available till 2015.24
Model inputs
The 3-year incidence of Nd:YAG laser capsulotomy after cataract surgery with single-piece monofocal acrylic AcrySof IOLs and comparator IOLs was derived from the post hoc analysis of the data available from a real-world evidence study.25 3-year risk probability of post-Nd:YAG capsulotomy complications of RD, glaucoma, and CME were derived from the published rates in studies (retrieved through a systematic literature search) using weighted average and probability equation methodology.26 Various input parameters used for the analysis along with their sources have been illustrated in Figures 1 and 2. These input parameters were considered common for all the countries assessed.
  | Figure 1 Three years cumulative Nd:YAG capsulotomy incidence. |
  | Figure 2 Estimated rates of complications at 3 years after Nd:YAG capsulotomy. |
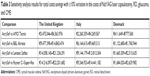
The national average of published Nd:YAG laser capsulotomy and vitrectomy diagnosis-related groups (DRGs) tariffs was used whereas average medical treatment costs for glaucoma and CME were sourced from the literature (Table 1). For performing analysis, Nd:YAG laser capsulotomy rates post 3 years of cataract surgery and rates of complications post 3 years of Nd:YAG laser capsulotomy were considered.
Considering the budget owner’s perspective, direct treatment costs were considered for the analysis. The components included under direct costs were Nd:YAG laser capsulotomy costs and costs of treating complications due to Nd:YAG laser capsulotomy, ie, RD, glaucoma, and CME. Costs were expressed as 2018 euros. Costs available in pounds and Danish krone were converted to euros using currency exchange rates dated May 30, 2018.37
Assumptions
Prices for AcrySof and competitor brands were considered equivalent in the present analysis because IOL costs are covered under cataract DRGs so overall costs to national payers per cataract procedure remain same regardless of the IOL model used during surgery. This is aligned with the approach used in earlier published studies.38,39 CME treatment costs data for Denmark and the United Kingdom were considered equivalent to Italian CME treatment costs given the lack of reliable published data in these countries.36
Model outputs
The model outputs analyzed in terms of health system benefits were reduction in the incidence of Nd:YAG laser capsulotomy and its subsequent complications with the use of single-piece monofocal acrylic AcrySof IOL vs comparator IOLs for all three countries. As weighted average of published rates was used to estimate probabilities of complications, 95% CIs available for the estimated probabilities of Nd:YAG capsulotomy procedure rates were used to calculate the lower and upper values of different complications. Total cost savings were assessed with respect to reduction in Nd:YAG laser capsulotomy and its complications between single-piece monofocal acrylic AcrySof and comparator IOLs.
Sensitivity analysis
Sensitivity analysis was conducted to obtain a range of minimum and maximum savings for the comparisons in order to test the robustness of the results. The lower and upper values for Nd:YAG capsulotomy rates were derived from the available CI values, and for complications (RD, glaucoma, and CME), the lower and upper values were derived using the Nd:YAG capsulotomy rates. Further, the ±10% variation in costs was applied to the lower and upper values for all the events to derive the minimum and maximum cost differences between comparators.
Results
Health system benefits
In hypothetical scenarios considered in the model, if the national cohort of cataract surgery eligible patients in a given year were to be implanted with any of the five single-piece monofocal acrylic IOLs, in 3 years after cataract surgery, the highest cases of Nd:YAG laser capsulotomy would be observed in patients implanted with Rayner C-/Super-flex (the United Kingdom: 60,598; Italy: 66,327; and Denmark: 7,150) followed by Lenstec Softec (the United Kingdom: 59,155; Italy: 64,748; and Denmark: 6,980), B&L Akreos (the United Kingdom: 44,246; Italy: 48,429; and Denmark: 5,521), AMO Tecnis (the United Kingdom: 24,528; Italy: 26,847; and Denmark: 2,894), and the lowest with AcrySof (the United Kingdom: 11,542; Italy: 12,634; and Denmark: 1,362). Subsequently, Rayner C-/Super-flex IOLs would be associated with the highest frequency of complications due to Nd:YAG capsulotomy followed by Lenstec Softec, B&L Akreos, AMO Tecnis, and the least by AcrySof. Differences in number of Nd:YAG capsulotomy procedures and its complications between single-piece monofocal acrylic AcrySof IOL and each comparator IOL are presented in Table 2.
Cost results
The total national health care costs of Nd:YAG capsulotomy procedure and its complications associated with each IOL considered in the analysis were as follow: AcrySof (the United Kingdom: €4.2 million; Italy: €2.7 million; and Denmark: €0.4 million); AMO Tecnis (the United Kingdom: €8.9 million; Italy: €5.8 million; and Denmark: €1.0 million), B&L Akreos (the United Kingdom: €16.1 million; Italy: €10.5 million; and Denmark: €1.9 million), Lenstec Softec (the United Kingdom: €21.5 million; Italy: €14.0 million; and Denmark: €2.5 million), Rayner C-/Super-flex (the United Kingdom: €22.1 million; Italy: €14.3 million; and Denmark: €2.6 million).
These results indicate that the use of single-piece monofocal acrylic AcrySof IOL would be a cost-saving approach for budget owners in all three countries. For the United Kingdom, Italy, and Denmark, the total cost savings with the use of single-piece monofocal acrylic AcrySof IOL over other IOLs ranged from €4.7, €3.0, and €0.5 million (vs AMO Tecnis) to €17.9, €11.6, and €2.1 million (vs Rayner C-/Super-flex), respectively (Figure 3A).
Sensitivity analysis
The results of sensitivity analysis are presented in Table 3. The biggest driver affecting cost savings is the Nd:YAG laser capsulotomy rates.
Discussion
This analysis aimed at assessing the cost impact of Nd:YAG laser capsulotomy and its complications due to the use of different single-piece monofocal acrylic IOLs.
Results indicate that using single-piece monofocal acrylic AcrySof IOL during cataract surgery could substantially offset the treatment burden of Nd:YAG capsulotomy procedures and subsequent complications when compared with other single-piece monofocal acrylic IOLs resulting in cost savings of €4.7–17.9 million in the United Kingdom, €3.0–11.6 million in Italy, and €0.5–2.1 million in Denmark. The findings indicate that Nd:YAG laser capsulotomy rates after cataract surgery should be considered an important clinical and economic criterion in selecting IOLs.
The 3-year Nd:YAG laser capsulotomy rates used in this study are in accordance with the previously published evidence that showed AcrySof IOLs and hydrophobic IOLs in general had lower incidence of Nd:YAG rates as compared to hydrophilic acrylic IOLs.15–20
Results from our study are in agreement with the earlier published economic evaluations. AcrySof IOLs were found to be the most cost-effective IOLs compared to other hydrophobic, polymethylmethacrylate, hydrophilic acrylic, and silicone IOLs in an analysis conducted from French, Italian, and Spanish health care systems’ perspective.36 Similarly, a study conducted in Sweden reported that risk of PCO and Nd:YAG laser capsulotomy and resulting costs were higher with hydrophilic IOLs than hydrophobic IOLs.40
The present analysis considered equivalent prices for all IOL brands since IOL costs are covered under cataract DRGs. We computed the cost difference per cataract procedure comparing AcrySof IOL with other IOLs realized due to downward cost savings by reduction in Nd:YAG capsulotomy procedures and treatment for YAG complications. As shown in Figure 3B, cost difference per IOL between AcrySof and AMO Tecnis were €9.85, €5.86, and €9.89, vs B&L Akreos were €24.82, €14.75, and €24.91, vs Lenstec Softec were €36.13, €21.47, and €36.27, and vs Rayner C-/Super-flex were €37.22, €22.12, and €37.37 in the United Kingdom, Italy, and Denmark, respectively. Important to note, IOLs are procured under tendering system in hospitals in which IOL procurement price is an important selection criterion. Therefore, if the price difference between AcrySof and other IOLs matches with the numbers described above, estimated cost savings for budget owners would be neutralized.
The main strength of this study is data sources considered for the analysis. Data for Nd:YAG laser capsulotomy rates were taken from a longitudinal, real-world evidence study with a large sample size and representative patient population,22 while risk probabilities of complications secondary to Nd:YAG laser capsulotomy were calculated from published studies retrieved through a recently conducted comprehensive systematic literature review. The current study employed a cost-consequence approach presenting disaggregated data for costs and outcomes thereby allowing decision makers to form their own opinion in a relevant context. Nevertheless, the study also has certain limitations. First, the Nd:YAG laser capsulotomy rates were derived from the UK-based study. Second, CME treatment costs data for Denmark and the United Kingdom were considered equivalent to Italian CME treatment costs, as we were unable to retrieve reliable cost estimates from published sources. Third, the usual demerits of data usage from a retrospective study such as susceptibility to confounding and issues such as missing data and lack of validation cannot be overlooked. Lastly, most recent data for the annualized cataract surgeries for each country were available only until the year 2015.
Conclusion
Use of single-piece monofocal acrylic AcrySof IOLs over other hydrophobic and hydrophilic acrylic IOLs is associated with substantially lower incidence of Nd:YAG laser capsulotomy procedures and its complications in 3 years after cataract surgery resulting in lower health care resource utilization and cost savings to health care system.
Acknowledgments
The authors would like to thank Purnima Pathak (Novartis Healthcare Pvt. Ltd.) for managing and providing writing assistance in the development of this manuscript. This study was funded by Alcon Laboratories, Inc., Fort Worth, TX, USA.
Disclosure
MD (Alcon Laboratories, Inc.), CB (Novartis Pharma AG), and SJ (Novartis Healthcare Pvt. Ltd.) are Novartis employees. The authors report no other conflicts of interest in this work.
References
Wang W, Yan W, Fotis K, et al. Cataract surgical rate and socioeconomics: a global study. Invest Ophthalmol Vis Sci. 2016;57(14):5872–5881. | ||
Boureau C, Lafuma A, Jeanbat V, Smith AF, Berdeaux G. Cost of cataract surgery after implantation of three intraocular lenses. Clin Ophthalmol. 2009;3:277–285. | ||
Karahan E, Er D, Kaynak S. An overview of Nd:YAG laser capsulotomy. Med Hypothesis Discov Innov Ophthalmol. 2014;3(2):45–50. | ||
Lundström M, Barry P, Henry Y, Rosen P, Stenevi U. Evidence-based guidelines for cataract surgery: guidelines based on data in the European registry of quality outcomes for cataract and refractive surgery database. J Cataract Refract Surg. 2012;38(6):1086–1093. | ||
Bhargava R, Kumar P, Sharma SK, Kaur A. A randomized controlled trial of peeling and aspiration of Elschnig pearls and neodymium: yttrium-aluminium-garnet laser capsulotomy. Int J Ophthalmol. 2015;8(3):590–596. | ||
Özyol E, Özyol P, Doğanay Erdoğan B, Önen M. The role of anterior hyaloid face integrity on retinal complications during Nd: YAG laser capsulotomy. Graefes Arch Clin Exp Ophthalmol. 2014;252(1):71–75. | ||
Sheard RM, Goodburn SF, Comer MB, Scott JD, Snead MP. Posterior vitreous detachment after neodymium:YAG laser posterior capsulotomy. J Cataract Refract Surg. 2003;29(5):930–934. | ||
Ge J, Wand M, Chiang R, Paranhos A, Shields MB. Long-term effect of Nd:YAG laser posterior capsulotomy on intraocular pressure. Arch Ophthalmol. 2000;118(10):1334–1337. | ||
Maedel S, Buehl W, Findl O; Cochrane Eyes and Vision Group. Intraocular lens optic edge design for the prevention of posterior capsule opacification after cataract surgery. Cochrane Database Syst Rev. 2017;2:CD003738. | ||
Auffarth GU, Brezin A, Caporossi A, et al. Comparison of Nd:YAG capsulotomy rates following phacoemulsification with implantation of PMMA, silicone, or acrylic intra-ocular lenses in four European countries. Ophthalmic Epidemiol. 2004;11(4):319–329. | ||
Fong CS, Mitchell P, Rochtchina E, Cugati S, Hong T, Wang JJ. Three-year incidence and factors associated with posterior capsule opacification after cataract surgery: the Australian prospective cataract surgery and age-related macular degeneration study. Am J Ophthalmol. 2014;157(1):171–179. | ||
Centers for Medicare and Medicaid Services. Data compendium (updated 2013, April 4). Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/DataCompendium/2011_Data_Compendium.html. Accessed August 7, 2018. | ||
Wormstone IM, Wang L, Liu CS. Posterior capsule opacification. Exp Eye Res. 2009;88(2):257–269. | ||
Vasavada AR, Raj SM, Shah GD, Nanavaty MA. Posterior capsule opacification after lens implantation: incidence, risk factors and management. Expert Rev Ophthalmol. 2013;8(2):141–149. | ||
Ernest PH. Posterior capsule opacification and neodymium: YAG capsulotomy rates with AcrySof acrylic and PhacoFlex II silicone intraocular lenses. J Cataract Refract Surg. 2003;29(8):1546–1550. | ||
Gangwani V, Hirnschall N, Koshy J, et al. Posterior capsule opacification and capsular bag performance of a microincision intraocular lens. J Cataract Refract Surg. 2011;37(11):1988–1992. | ||
Iwase T, Nishi Y, Oveson BC, Jo YJ. Hydrophobic versus double-square-edged hydrophilic foldable acrylic intraocular lens: effect on posterior capsule opacification. J Cataract Refract Surg. 2011;37(6):1060–1068. | ||
Sacu S, Findl O, Menapace R, Buehl W, Wirtitsch M. Comparison of posterior capsule opacification between the 1-piece and 3-piece Acrysof intraocular lenses: two-year results of a randomized trial. Ophthalmology. 2004;111(10):1840–1846. | ||
Kugelberg M, Wejde G, Jayaram H, Zetterström C. Two-year follow-up of posterior capsule opacification after implantation of a hydrophilic or hydrophobic acrylic intraocular lens. Acta Ophthalmol. 2008;86(5):533–536. | ||
Vasavada AR, Raj SM, Shah A, Shah G, Vasavada V, Vasavada V. Comparison of posterior capsule opacification with hydrophobic acrylic and hydrophilic acrylic intraocular lenses. J Cataract Refract Surg. 2011;37(6):1050–1059. | ||
Linnola RJ, Sund M, Ylönen R, Pihlajaniemi T. Adhesion of soluble fibronectin, laminin, and collagen type IV to intraocular lens materials. J Cataract Refract Surg. 1999;25(11):1486–1491. | ||
Ursell PG, Dhariwal M, Majirska K, et al. Three-year incidence of Nd:YAG capsulotomy and posterior capsule opacification and its relationship to monofocal acrylic IOL biomaterial: a UK real world evidence study. Eye. 2018;32(10):1579–1589. | ||
NICE. Medical technologies evaluation programme methods guide. Process and methods (PMG33) (updated 2017). Available from: https://www.nice.org.uk/process/pmg33/chapter/evidence-synthesis-and-cost-consequence-analysis. Accessed June 06, 2018. | ||
Eurostat. Surgical operations and procedures performed in hospitals by ICD-9-CM (updated 2018 July 5). Available from: http://appsso.eurostat.ec.europa.eu/nui/show.do?query=BOOKMARK_DS-199606_QID_-18B7B52E_UID_-3F171EB0&layout=ICD9CM,L,X,0;TIME,C,Y,0;GEO,L,Y,1;UNIT,L,Z,0;ICHA_HC,L,Z,1;INDICATORS,C,Z,2;&zSelection=DS-199606INDICATORS,OBS_FLAG;DS-199606UNIT,P_HTHAB;DS-199606ICHA_HC,IN;&rankName1=ICHA-HC_1_2_-1_2&rankName2=UNIT_1_2_-1_2&rankName3=INDICATORS_1_2_-1_2&rankName4=ICD9CM_1_2_0_0&rankName5=TIME_1_0_0_1&rankName6=GEO_1_2_1_1&sortR=ASC_-1_FIRST&rStp=&cStp=&rDCh=&cDCh=&rDM=true&cDM=true&footnes=false&empty=false&wai=false&time_mode=ROLLING&time_most_recent=false&lang=EN&cfo=%23%23%23%2C%23%23%23.%23%23%23. Accessed August 7, 2018. | ||
Dhariwal M, Bouchet C, Boyle DO, Khan J, Venerus A, Muthutantri A. Incidence of Nd:YAG capsulotomy following single-piece monofocal acrylic IOL implantation: a retrospective real-world evidence study in the UK. 36th Congress of the European Society of Cataract and Refractive Surgeons (ESCRS), September 22–26, 2018; Vienna, Austria. | ||
O’Boyle D, Vives CP, Samavedam S, et al. Post-Nd:YAG laser complications in cataract patients treated for posterior capsular opacification: a systematic literature review. ISPOR Europe 2018, Congress, Barcelona, Spain; 2018. | ||
NHS. National tariff payment system (HRG Code – BZ33Z) (updated 2018, February 23). Available from: https://improvement.nhs.uk/resources/national-tariff-1719/. Accessed August 7, 2018. | ||
Italian Ministry of Health. National Health Drug Tariff (Code – 13.64) (updated 2013, January 28). Available from: http://www.trovanorme.salute.gov.it/norme/renderPdf.spring?seriegu=SG&datagu=28/01/2013&redaz=13A00528&artp=3&art=1&subart=1&subart1=10&vers=1&prog=001. Accessed August 7, 2018. | ||
Denmark Health Data Agency. DRG Tariffs (DRG CODE – 02MP24) (updated 2018, May 15). Available from: https://ny.sundhedsdatastyrelsen.dk/sds/da/afregning-og-finansiering/takster-drg/takster-2018. Accessed August 7, 2018. | ||
NHS. National tariff payment system (HRG Code – BZ83B) (updated 2018, February 23). Available from: https://improvement.nhs.uk/resources/national-tariff-1719/. Accessed August 7, 2018. | ||
Italian Ministry of Health. National health drug tariff (DRG Code – 36) (updated 2013). Available from: http://www.gazzettaufficiale.it/do/atto/serie_generale/caricaPdf?cdimg=13A0052800100010110001&dgu=2013-01-28&art.dataPubblicazioneGazzetta=2013-01-28&art.codiceRedazionale=13A00528&art.num=1&art.tiposerie=SG. Accessed August 07, 2018. | ||
Denmark Health Data Agency. DRG tariffs (DRG Code – 02MP07) (updated 2018, May 15). Available from: https://ny.sundhedsdatastyrelsen.dk/sds/da/afregning-og-finansiering/takster-drg/takster-2018. Accessed August 7, 2018. | ||
Rahman MQ, Beard SM, Discombe R, Sharma R, Montgomery DM. Direct healthcare costs of glaucoma treatment. Br J Ophthalmol. 2013;97(6):720–724. | ||
Koleva D, Motterlini N, Schiavone M, Garattini L; Study Group GLAUCO. Medical costs of glaucoma and ocular hypertension in Italian referral centres: a prospective study. Ophthalmologica. 2007;221(5):340–347. | ||
Olsen J, Berdeaux G, Skov J. Glaucoma costs in Denmark in treatment naive patients. Acta Ophthalmol. 2013;91(1):25–31. | ||
Smith AF, Lafuma A, Berdeaux G, et al. Cost-effectiveness analysis of PMMA, silicone, or acrylic intra-ocular lenses in cataract surgery in four European countries. Ophthalmic Epidemiol. 2005;12(5):343–351. | ||
Bloomberg. Currencies; 2018. Available from: https://www.bloomberg.com/markets/currencies. Accessed August 7, 2018. | ||
Pineda R, Denevich S, Lee WC, Waycaster C, Pashos CL. Economic evaluation of toric intraocular lens: a short- and long-term decision analytic model. Arch Ophthalmol. 2010;128(7):834–840. | ||
Laurendeau C, Lafuma A, Berdeaux G. Modelling lifetime cost consequences of toric compared with standard IOLs in cataract surgery of astigmatic patients in four European countries. J Med Econ. 2009;12(3):230–237. | ||
Cullin F, Busch T, Lundström M. Economic considerations related to choice of intraocular lens (IOL) and posterior capsule opacification frequency – a comparison of three different IOLs. Acta Ophthalmol. 2014;92(2):179–183. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.