Back to Journals » Local and Regional Anesthesia » Volume 8
Comparative evaluation of continuous intercostal nerve block or epidural analgesia on the rate of respiratory complications, intensive care unit, and hospital stay following traumatic rib fractures: a retrospective review
Authors Britt T, Sturm R, Ricardi R, Labond V
Received 7 January 2015
Accepted for publication 15 March 2015
Published 27 October 2015 Volume 2015:8 Pages 79—84
DOI https://doi.org/10.2147/LRA.S80498
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Stefan Wirz
Todd Britt, Ryan Sturm, Rick Ricardi, Virginia Labond
Department of Emergency Medicine, Genesys Regional Medical Center, Grand Blanc, MI, USA
Background: Thoracic trauma accounts for 10%–15% of all trauma admissions. Rib fractures are the most common injury following blunt thoracic trauma. Epidural analgesia improves patient outcomes but is not without problems. The use of continuous intercostal nerve blockade (CINB) may offer superior pain control with fewer side effects. This study's objective was to compare the rate of pulmonary complications when traumatic rib fractures were treated with CINB vs epidurals.
Methods: A hospital trauma registry provided retrospective data from 2008 to 2013 for patients with 2 or more traumatic rib fractures. All subjects were admitted and were treated with either an epidural or a subcutaneously placed catheter for continuous intercostal nerve blockade. Our primary outcome was a composite of either pneumonia or respiratory failure. Secondary outcomes included total hospital days, total ICU days, and days on the ventilator.
Results: 12.5% (N=8) of the CINB group developed pneumonia or had respiratory failure compared to 16.3% (N=7) in the epidural group. No statistical difference (P=0.58) in the incidence of pneumonia or vent dependent respiratory failure was observed. There was a significant reduction (P=0.05) in hospital days from 9.72 (SD 9.98) in the epidural compared to 6.98 (SD 4.67) in the CINB group. The rest of our secondary outcomes showed no significant difference.
Conclusion: This study did not show a difference in the rate of pneumonia or ventilator-dependent respiratory failure in the CINB vs epidural groups. It was not sufficiently powered. Our data supports a reduction in hospital days when CINB is used vs epidural. CINB may have advantages over epidurals such as fewer complications, fewer contraindications, and a shorter time to placement. Further studies are needed to confirm these statements.
Keywords: thoracic trauma, complications, analgesic, rib fractures
Introduction
Thoracic trauma accounts for 10%–15% of all trauma admissions.1 Rib fractures are the most common injury following thoracic trauma, with morbidity and mortality increasing with each additional rib fractured.1–4 A review of 64,750 traumatic rib fracture patients in the National Trauma Data Bank revealed an all-cause mortality rate of 5.8% with those who sustained a single traumatic rib fracture.1 This increased to 34% in patients with seven or more ribs fractured. Adequate pain control for traumatic rib fractures improves respiratory mechanics and thus decreases pulmonary complications such as atelectasis, pneumonia, and respiratory failure.3–5 Effective analgesia remains one of the critical components of the treatment plan.6,7 The most common and historically used method for pain control of multiple rib fractures has been the use of intermittent intravenous (IV) opioids.5 Several other methods are used for pain control in this patient population including continuous IV opioid infusions, patient-controlled IV analgesia, paravertebral blocks, intermittent intercostal nerve blocks, epidural analgesia, and intrapleural anesthesia.8–13 Many of these treatment modalities are invasive and carry significant potential side effects such as cost, development of an epidural abscess, and the sedative effects of IV opioids. In 2005, Kieninger et al14 demonstrated that the use of epidural analgesia increased the length of hospital stay, as well as complications in elderly patients that were treated for rib fractures.
In the last few years, a new concept for acute pain management following thoracic trauma has been utilized. A subcutaneous, extrathoracic catheter is placed bedside by a member of the trauma team. Following placement, infusion of a local anesthetic via this catheter results in a continuous intercostal nerve block (CINB). This method for analgesia has shown promising results, but it is backed by few studies. A nonrandomized, prospective study done by Truitt et al15 in 2010 looked at 30 consecutive trauma patients who sustained three or more traumatic rib fractures and were treated with an extrathoracic, subcutaneously placed catheter with continuous infusion of local anesthetic for intercostal nerve blockade. The authors showed a significant improvement of sustained maximal inspiration and numeric pain scores and reported no complications of its use. Another nonrandomized, prospective study by Truitt et al16 in 2011 studied 102 trauma patients with three or more unilateral rib fractures and compared the outcomes to historical controls of patients treated with epidural analgesia. The authors showed a significant improvement in pulmonary function, pain control, and length of hospital stay. The purpose of this study is to compare CINB versus epidural anesthesia as it relates to respiratory complications and hospital stay.
Materials and methods
This study was approved by the hospital’s institutional review board on September 18, 2013. This retrospective study took place at a level 2 trauma center in Grand Blanc, MI, USA. Data are routinely collected on all patients evaluated by the trauma team. The data are recorded on a standardized trauma form. This form includes, but is not limited to, time and date, patient demographics, history and physical findings, test results, procedures, diagnosis, hospital course, and disposition. It was updated daily by members of the trauma service during admission until patient discharge. Data from these forms are then stored in a hospital data registry, which is then submitted to the National Trauma Data Bank.
We searched the trauma registry data from 2008 to 2013 for all patients 18 years and older that presented to our trauma center with two or more traumatic rib fractures following blunt thoracic trauma. All subjects studied were admitted to the hospital and had their pain treated with either an epidural or a subcutaneously placed CINB. The On-Q pump provided the continuous intercostal nerve blockade (Kimberly-Clark Corporation, Irvine, CA, USA). The On-Q pump, available for many years, is one of several intercostal pumps designed for analgesia. It is a 19-gauge multihole catheter designed to provide even distribution along the infusion segment. At the study site, the catheter was placed either in the emergency department or on the hospital floor by the trauma team. Once the catheter was placed, an infusion of local anesthetic was initiated. All subjects were monitored for any adverse reactions throughout their admission.
Epidurals at the study site were placed by the anesthesia department after being consulted by the trauma team. These catheters were placed to infuse anesthetic into the epidural space. The anesthetic mixture used was bupivacaine 0.1% with 5 μg/mL of fentanyl. The rate is set at a rate of 8 mL/hour as a continuous infusion through the catheter. Placement of these catheters was done after admission. The institutional protocol for the management of trauma patients with rib fractures included treatment with enoxaparin. All patients in the study received enoxaparin. The placement technique for either method was determined by the physician providing treatment and may have varied based on practitioner preference.
At our institution, the On-Q pump system replaced epidural analgesia as a treatment strategy for rib fractures in 2011. The On-Q system uses 0.5% bupivacaine infused at a continuous rate of 4 mL/hour. Data were collected and analyzed for the epidural group from the years 2008 to 2010 and the CINB group from the years 2011 to 2013.
The confounding factors between groups were controlled for by comparing the demographic data for each group, which included age, sex, smoker versus nonsmoker, and injury severity score (ISS). Pre-existing comorbidities of congestive heart failure, anticoagulant use, and the presence of a primary respiratory disorder were noted. A primary respiratory disorder in our study refers to COPD, emphysema, or asthma. Anticoagulant use excludes aspirin.
Subjects were excluded if they had fractures determined to be old or pathologic, the subjects were less than 18 years of age, or they were placed on a ventilator for reasons other than thoracic trauma.
Our primary outcome was a composite of the development of either pneumonia or respiratory failure, as defined by the patient having to be placed on a ventilator. The diagnosis of pneumonia was defined by the trauma team based on specific criteria. A diagnosis of pneumonia could be made by the fulfillment of either criteria 1 or criteria 2, which will be discussed. Intubation by the treating physician for the management of respiratory compromise (not intracranial trauma, etc) was considered as respiratory failure.
Criteria 1 included rales or dullness to percussion on physical exam, plus any one of the following: new onset of purulent sputum or change in sputum character; an organism isolated from culture; or isolation of a pathogen in the sputum. Criteria 2 included new chest X-ray findings of an infiltrate, cavitation, or pleural effusion, plus any one of the following: new purulent sputum (defined by >25 neutrophils and <10 squamous cells per low power field) or change in character; an organism isolated from culture; a diagnostic antibody or antigen; or histopathologic evidence of pneumonia.
Secondary outcomes of this study included the total number of days in the hospital (non-ICU + ICU), total ICU days, and number of days on the ventilator.
Plan of analysis
Treatment groups were based on the time periods for which one or the other nerve block method was exclusively used. To test for an association between complications and the nerve block method, the rate of complications between treatment groups was compared by chi-squared analysis with significance set at P<0.05. Length of stay data were analyzed by a Student’s t-test for independent groups. A multiple regression analysis was calculated to control for potential confounding factors (age, sex, ISS, and number of fractures). A power calculation determined that a total of 90 patients was needed to achieve a minimum power of 82% to detect a 35% relative difference in complication rates as significant.
Results
One hundred and seven subjects met the inclusion criteria with 59% (number [N] =64) in the CINB group and 41% (N=43) in the epidural group. Both groups were similar in terms of sex (P=0.29), prevalence of COPD (P=0.16), tobacco use (P=0.86), and ISS (P=0.33). There was a significant difference (P=0.01) in the age between groups. The patients in the CINB group had a mean age of 70.5 (standard deviation [SD] =16.9) years when compared to that of 60.9 (SD =17.3) years in the epidural group. There was a difference in the prevalence of diabetes, which approached significance (P=0.09) with 21.9% (N=14) in the CINB group and 9.3% (N=4) in the epidural group. There was also a significant difference (P=0.02) with respect to the presence of anticoagulants in the CINB group (15.6%) compared to the epidural group (2.3%). The number of ribs fractured and the ISS were found to be similar between the two groups. However, bilateral presentation differed significantly (Table 1).
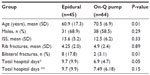  | Table 1 Characteristics by Treatment Group |
Regarding our primary outcome, 12.5% (N=8) of subjects treated with the CINB pump developed pneumonia or had respiratory failure requiring a ventilator compared to 16.3% (N=7) of subjects in the epidural group. A regression analysis controlling for age, diabetes, and fractures was performed and found no difference between the groups in terms of the incidence of pneumonia or ventilator-dependent respiratory failure (odds ratio =1.8; 95% confidence interval: 0.5–5.8; P=0.32). These findings represent the data after exclusion of one outlier in the CINB group. All subjects fell into the range of 0–20 total ventilator days. The outlier had a total of 32 ventilator days and represented an extreme outlier for this dataset (Table 1).
The other secondary outcomes including ventilator days for all subjects (P=0.61), ventilator days for intubated subjects (P=0.66), and total ICU days (P=0.51) showed no significant differences.
Discussion
This study demonstrated a trend toward a lower rate of pneumonia or ventilator-dependent respiratory failure in the CINB group, but the findings did not reach statistical significance. The time period of CINB use was not sufficient at this site to allow for a higher incidence rate of complications to accrue. We did observe a significant (P=0.05) difference in mean hospital days in the CINB group (6.9 days) when compared to the epidural group (9.72 days). However, there was no difference in the number of days on the ventilator or total ICU days (P=0.51).
Regarding our one outlier, the inclusion of this subject changes the total hospital days in the CINB group to 7.49 (SD =6.18) days, and that of the epidural group remains at 9.72 (SD =9.98) days. The reduction in total hospital days would no longer be significant (P=0.15) with this subject included in the data. No significant changes are seen in terms of the incidence of pneumonia or ventilator-dependent respiratory failure (P=0.72), the total days on the ventilator for all subjects (P=0.35), or the days on the ventilator for intubated subjects (P=0.43).
A few studies have compared epidural versus CINB in traumatic rib fractures. CINB had improved pain scores, pulmonary function, and hospital length of stay with less overall complications when compared to epidurals.17,18 This study supports a reduction of total days in the hospital, as shown in these previous studies. No significant change was seen in the incidence of respiratory failure or pneumonia, but these finding may still be of benefit to the trauma community. As mentioned previously, the use of epidurals comes with several contraindications and complications of use. These potential complications of placement are an even greater concern in the trauma patient. These complications include failed catheter placement, inadequate analgesia, hypotension, epidural hematoma, epidural abscess, meningitis, and respiratory failure.12,13 A retrospective review by Christie and McCabe13 in 2006 looked at 8,100 postoperative patients receiving epidural pain control. Although the subjects were not blunt trauma patients, the study showed epidural abscess, meningitis, and epidural hematoma to be the most common of these complications.13 Epidurals also have several contraindications for placement, many of which are relevant to trauma patients. Some of these contraindications that pertain to trauma patients include coagulopathy, spinal cord injury, intracranial hemorrhage, fever, and altered mental status.6
Age is an independent risk factor for increased morbidity and mortality following traumatic rib fractures.3,4,17–20 A cohort study by Bergeron in 2003 showed a mortality rate that was five times higher in patients ≥65 years old compared to those <65 years old in 409 patients following traumatic rib fractures. This was despite a lower ISS seen in the ≥65-year-old group.21 This accentuates the importance of adequate pain control in this specific population. Unfortunately, the elderly are more likely to possess one or more of the contraindications to epidural placement. It has been reported that at least 10% of Americans over 65 years are on anticoagulant medications as of 2007.22 The study by Kieninger et al14 in 2005 concluded that epidural use in the elderly is associated with a prolonged length of stay and an increased incidence of pulmonary complications when compared to IV narcotics, particularly in patients with lower ISS.
Placement of a subcutaneous, extrathoracic catheter for continuous peripheral intercostal nerve blockade thus poses a theoretical advantage over epidurals. There are fewer contraindications for its use, making it ideal for trauma patients, especially the elderly. The manufacturer of the On-Q pump lists no specific absolute contraindications for this specific use.23 Complications are thought to be rare, but they may include the development of cellulitis, an adverse reaction to local anesthetic. No patients in this study or previous studies of CINBs have reported any complications from its placement or use.15,16 Although the time to initiation of the primary pain control method was not looked at in our study, or in any others we could find, there may be an advantage to using the CINB versus the traditional epidural. CINB can be placed at the bedside relatively easily by the trauma surgeon or surgery resident. This is common practice at the study site, and a significantly reduced time to placement has been anecdotally reported when compared to epidurals. A large, multicenter, prospective study examining failure rates and complications could aid in supporting these claims.
It is interesting that there was a lower overall length of stay in the CINB group, while there was no difference in the incidence of pneumonia, respiratory failure, ventilator days, ventilator days for intubated subjects, or total ICU days between groups. The lack of consistency regarding the significant differences of these measures may represent a chance finding or the existence of an outlier with a 66-day length of stay. When this outlier was removed from the analysis, the difference in hospital length of stay was no longer significant (Table 1). If that is the case, we can feel comfortable using either therapy to improve the prevention of pulmonary complications of traumatic rib fractures. Further studies on the true incidence of complications and effective pain control would be required in order to conclude overall equality between the two methods.
A few study limitations are worth noting. First, this is a single-center, retrospective examination of data. Second, although the study was powered sufficiently overall, the magnitude of difference in the complication rates between groups was underestimated. The finding of a lower incidence rate among the CINB pump may have reached statistical significance in a study powered at a magnitude difference of 20% rather than our 35% estimate. Additionally, subjects who were on anticoagulation when they presented to the emergency department were not excluded from the On-Q group. A total of 15.6% (N=10) of subjects in the On-Q group were on anticoagulant medications, excluding aspirin, compared to 2.3% (N=1) of patients in the epidural group. This same group of patients was mostly excluded from epidural placement. Based on this, it could be argued that this specific group has comorbidities that can result in an increased morbidity and mortality following blunt thoracic trauma. The inclusion of this patient population in the On-Q group alone may have skewed the results in favor of epidurals. It is important to note that while anticoagulation of 15% of the On-Q group creates bias in terms of bleeding, the parameters we studied – respiratory failure and pneumonia – are not related to this complication.
Conclusion
This study did not demonstrate a statistically significant difference in the rate of pneumonia or ventilator-dependent respiratory failure between patients given intercostal nerve block or epidural anesthesia. Although the low incidence of complications may have caused the study to be underpowered for significance, our data did support a significant finding in the reduction in hospital days when intercostal nerve block is used versus epidural anesthesia in traumatic rib fractures. CINB may have additional theoretical advantages over epidurals, such as fewer complications of catheter placement, fewer contraindications for use, and a shorter time to placement. Further studies are needed to confirm these statements.
Disclosure
The authors report no conflicts of interest in this work.
References
Flagel BT, Luchette FA, Reed RL, et al. Half-a-dozen ribs: the breakpoint for mortality. Surgery. 2005;138(4):717–723. | |
Sirmali M, Türüt H, Topçu S, et al. A comprehensive analysis of traumatic rib fractures: morbidity, mortality and management. Eur J Cardiothorac Surg. 2003;24(1):133–138. | |
Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma. 2000;48(6):1040–1046. | |
Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma. 1994;37(6):975–979. | |
Easter A. Management of patients with multiple rib fractures. Am J Crit Care. 2001;10(5):320–327. | |
Simon BJ, Cushman J, Barraco R, et al; EAST Practice Management Guidelines Work Group. Pain management guidelines for blunt thoracic trauma. J Trauma. 2005;59(5):1256–1267. | |
Osinowo OA, Zahrani M, Softah A. Effect of intercostal nerve block with 0.5% bupivacaine on peak expiratory flow rate and arterial oxygen saturation in rib fractures. J Trauma. 2004;56(2):345–347. | |
Wisner DH. A stepwise logistic regression analysis of factors affecting morbidity and mortality after thoracic trauma: effect of epidural analgesia. J Trauma. 1990;30(7):799–804. | |
Ullman DA, Fortune JB, Greenhouse BB, Wimpy RE, Kennedy TM. The treatment of patients with multiple rib fractures using continuous thoracic epidural narcotic infusion. Reg Anesth. 1989;14(1):43–47. | |
Bulger EM, Edwards T, Klotz P, Jurkovich GJ. Epidural analgesia improves outcome after multiple rib fractures. Surgery. 2004;136(2):426–430. | |
Wu CL, Jani ND, Perkins FM, Barquist E. Thoracic epidural analgesia versus intravenous patient-controlled analgesia for the treatment of rib fracture pain after motor vehicle crash. J Trauma. 1999;47(3):564–567. | |
Paech MJ, Godkin R, Webster S. Complications of obstetric epidural analgesia and anaesthesia: a prospective analysis of 10,995 cases. Int J Obstet Anesth. 1998;7(1):5–11. | |
Christie IW, McCabe S. Major complications of epidural analgesia after surgery: results of a six-year survey. Anaesthesia. 2007;62(4):335–341. | |
Kieninger AN, Bair HA, Bendick PJ, Howells GA. Epidural versus intravenous pain control in elderly patients with rib fractures. Am J Surg. 2005;189(3):327–330. | |
Truitt MS, Mooty RC, Amos J, Lorenzo M, Mangram A, Dunn E. Out with the old, in with the new: a novel approach to treating pain associated with rib fractures. World J Surg. 2010;34(10):2359–2362. | |
Truitt MS, Murry J, Amos J, et al. Continuous intercostal nerve blockade for rib fractures: ready for primetime? J Trauma. 2011;71(6):1548–1552. | |
Mohta M, Verma P, Saxena AK, Sethi AK, Tyagi A, Girotra G. Prospective, randomized comparison of continuous thoracic epidural and thoracic paravertebral infusion in patients with unilateral multiple fractured ribs – a pilot study. J Trauma. 2009;66(4):1096–1101. | |
Holcomb JB, McMullin NR, Kozar RA, Lygas MH, Moore FA. Morbidity from rib fractures increases after age 45. J Am Coll Surg. 2003;196(4):549–555. | |
Byun JH, Kim HY. Factors affecting pneumonia occurring to patients with multiple rib fractures. Korean J Thorac Cardiovasc Surg. 2013; 46(2):130–134. | |
Brasel KJ, Guse CE, Layde P, Weigelt JA. Rib fractures: relationship with pneumonia and mortality. Crit Care Med. 2006;34(6):1642–1646. | |
Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma. 2003;54(3):478–485. | |
U.S Department of Health and Human Services. [webpage on the Internet]. Agency for healthcare research and quality. U.S spends nearly $1 billion on blood thinners for adults. Available from: http://archive.ahrq.gov/news/newsroom/news-and-numbers/111209.html. Accessed November 1, 2013. | |
Kimberly Clark Health Care Company (US). [webpage on the Internet]. On-Q®PainBuster®Post-Op Pain Relief System, 2004 [cited Dec 1, 2013]. Available from: http://www.iflo.com/prod_onq_classic.php. Accessed November 1, 2013. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
