Back to Journals » International Medical Case Reports Journal » Volume 16
Combination of Crusted Scabies with Bullous Scabies: A Rare Case
Authors Asnawi V, Maulida M, Hidayati A, Gunawan H , Dwiyana RF , Hindritiani R
Received 24 November 2022
Accepted for publication 15 February 2023
Published 11 March 2023 Volume 2023:16 Pages 153—158
DOI https://doi.org/10.2147/IMCRJ.S396234
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Vella Asnawi,1,2 Mimi Maulida,1,2 Arie Hidayati,1,2 Hendra Gunawan,3,4 Reiva Farah Dwiyana,3,4 Reti Hindritiani3,4
1Department of Dermatology and Venereology, Faculty of Medicine, Universitas Syiah Kuala, Banda Aceh, Aceh, Indonesia; 2Department of Dermatology and Venereology, Dr. Zainoel Abidin General Hospital, Banda Aceh, Aceh, Indonesia; 3Department of Dermatology and Venereology, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia; 4Department of Dermatology and Venereology, Hasan Sadikin General Hospital, Bandung, West Java, Indonesia
Correspondence: Vella Asnawi, Department of Dermatology and Venereology, Dr. Zainoel Abidin General Hospital, Jl. Tgk.Daud Beureueh No. 108, Banda Aceh, Aceh, Indonesia, Tel +6281938199931, Email [email protected]
Abstract: Scabies is a parasitic skin disease caused by Sarcoptes scabiei var. hominis. Crusted scabies, also known as Norwegian scabies, is a rare and severe form of scabies that occurs more frequently in immunocompromised, elderly, disabled, and debilitated patients. The present study reports a case of crusted scabies combined with bullous scabies. A 44-year-old man was admitted with the chief complaint of red, thick, scaly patches of skin accompanied by crusting that felt itchy and worsened at night. The lesions had appeared all over his body intermittently for the last 10 years; however, the complaints worsened in the last 2 months. From dermatological status, the anterior and posterior thoracic regions and between the fingers of both hands showed generalized distribution of erythematous, yellowish, hyperkeratotic plaques with clear boundaries, pustules, and blisters on an erythematous base with multiple erosions and excoriations. S. scabiei were found on skin scraping examination, and histopathological examination supported the diagnosis of bullous scabies. The patient received 5% permethrin lotion topical therapy and systemic ivermectin therapy. In addition, the patient was given systemic antibiotics. The lesions improved after 2 weeks of therapy, and no S. scabiei were found on the subsequent microscopic examination. Treatment with a combination of topical and systemic scabicidal agents produced a favorable outcome in this patient.
Keywords: Norwegian scabies, bullous, permethrin, ivermectin, Sarcoptes
Introduction
Scabies is a highly contagious, ectoparasitic skin disease caused by the Sarcoptes scabiei var. hominis parasite.1 It is transmitted through direct skin-to-skin contact. The condition is characterized by the symptoms of very itchy skin lesions at night accompanied by skin eruptions with varying degrees of severity.1,2 Scabies is divided into three subtypes based on the clinical appearance as: classic scabies, crusted scabies, and bullous scabies.3 Classic scabies is also known as typical, standard, or common scabies. The clinical manifestations are scattered papules that are itchy followed by excoriated lesion with predilection on finger webspaces, hands, volar wrists, axillae, feet, waistline, inner thighs, areola in women, and genitalia in men.1,3 The crusted subtype or known as Norwegian scabies, has more severe symptoms and most commonly found in immunocompromised patients.3 The immune system fails to defend against mites in the skin, resulting in mite hyper-infestation in the host skin.1,2 Crusted scabies may also occur in patients with neurological diseases that cause decreased sensation, in immobile patients with reduced scratching ability, and in genetically susceptible patients. The most severe subtype of scabies is bullous scabies, which has atypical symptoms resembling bullous pemphigoid disease.2 Norwegian scabies or crusted scabies is rare; the incidence was reported to be around 0.5% in one study.4 Until recently, reports of crusted scabies accompanied by bullous scabies case were limited. We report a case of a man with clinical manifestations of crusted scabies combined with bullous scabies. The patient provided informed consent to publish their case details and any accompanying images. No institutional approval is needed to publish this case.
Case
A 44-year-old married Acehnese man presented to the dermatology and venereology outpatient clinic of Zainoel Abidin Hospital on November 8, 2021, with the chief complaint of thick, red, scaly patches and scabs all over the body that felt itchy, especially at night. The symptoms had appeared intermittently for the last 10 years; however, the condition had worsened in the last 2 months. The initial lesions were red patches and small blisters filled with cloudy fluid that were noted on the elbow and left leg in 2011. The lesions then spread to the abdomen, buttocks, thighs, and calves, accompanied by itching at night. The patient lives with his wife and children in the same house. The patient’s child also complained of itchy, red spots between the fingers, especially at night, for the last 2 months. The patient sought primary health care and was referred to a dermatologist, but the symptoms persisted. No history of diabetes mellitus, HIV/AIDS, leprosy, or other autoimmune diseases was noted. There was no history of allergies to food, drugs, or other allergens. The patient works as a bus driver and often interacts with many people. The patient has children who attend the Islamic boarding schools. The patient bathes twice daily and uses different towels than other family members. The patient’s clothes were not washed separately from other family members and were washed with normal-temperature water.
Based on the physical examination, the patient was fully alert and the vital sign within normal limit. From dermatological status multiple hyperpigmented macules, erythematous papules, excoriation, erosion, scales, and crusts were generalized distributed entire the body (Figure 1). Other physical examination within normal limit. Additional examinations were performed for this patient, including a COVID-19 rapid antigen serology test with a negative result and an HIV test with non-reactive result. Skin scraping examination was performed, and Sarcoptes scabiei mites were found (Figure 2). On the 8th day of follow-up examination, several blisters were found on the leg, and on dermatological examination, we found multiple yellowish erythematous and hyperkeratotic plaques with well-defined, irregular edges of varying sizes accompanied by thick scales, vesicles, bullae, crusting, erosion, and excoriation with generalized distribution on the anterior, posterior, inferior extremity, and manus regions. Histopathological examination was performed with microscopic results of tissue preparations that revealed a stratified, encrusted epithelium with mild hyperkeratosis. In the infra-basal layer, one or two bullae were found with lymphocytes. The subepithelium contained fibromyxoid tissue. The impression of the histopathological examination was scabies bullosa (Figure 3), and pus culture analysis revealed the bacterium Kocuria kristinae, a gram-positive coccus from the Micrococcaceae family, and penicillin-class medications were recommended (Figure 4). Based on the results of supporting examinations, the diagnosis of this patient was erythroderma with Norwegian scabies and bullous scabies.
 |
Figure 1 Clinical presentation of patient when admitted to the hospital (November 8, 2021). |
 |
Figure 3 Histopathological result showed subepidermal blister with lymphocytes infiltration in fibromyxoid tissue. |
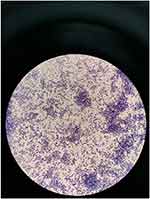 |
Figure 4 Result of pus culture showed Kocuria kristinae colony. |
The patient was treated with permethrin lotion 5% administered at night on days 1, 6, 9, 10, 11, and 12; mupirocin ointment 2% administered topically in the morning, afternoon, and evening; salicylic acid 3% combined with clobetasol propionate ointment applied topically during the day; and salicylic acid 3% combined with desoximetasone 0.25% ointment applied topically in the morning. Sofra-Tulle® was applied topically to areas with open, wet wounds, and salicylic acid 10% + vaseline was applied topically in the morning and evening.
As systemic treatment patient was received intravenous ceftriaxone 1 g/12 hours for 10 days, cetirizine tablet 3×50 mg orally, and ivermectin 24 mg orally on days 1, 2, 8, 9, 15, 27, and 29. After obtaining the pus culture results, clindamycin 2×300 mg was added for the treatment. After day 8, new vesicles and blisters appeared on the lower extremities, and the patient received methylprednisolone 3×8 mg/8 hours orally (Figure 5). The patient was then discharged from the hospital and continued the therapy at home. He gradually improved, with some lesions becoming dry, leaving only hyperpigmented and hypopigmented macules (Figure 6). The prognosis of the patient in terms of quo ad vitam, quo ad functionam, and quo ad sanationam was dubia ad bonam.
 |
Figure 5 Clinical presentation of patient after 8 days of hospitalization (November 17, 2021). |
 |
Figure 6 Clinical presentation of patient after 15 days of hospitalization (November 23, 2021). |
Discussion
In this case, a 44-year-old male patient presented with the complaint of thick, red, scaly patches and itchy scabs that had been present for 10 years and had worsened in the last 2 months. The initial complaint began with the appearance of itchy, red, watery spots on the elbows followed by widespread itching accompanied by thickened skin over most of the body. The itching was worst at night leading to sores and blisters caused by heavy scratching. The literature mentions that Norwegian scabies is a severe and highly contagious type of scabies, characterized by generalized crusted lesions resembling psoriasis.5 Norwegian scabies is caused by the same mites as classic scabies, but in very large numbers, ranging from thousands to millions.6,7 This type of scabies is found in immunocompromised patients, patients on long-term immunosuppressive therapy (organ transplant recipients, long-term corticosteroid therapy), patients with impaired T-cell response (HIV or HTLV-1 virus infection), patients with decreased sensation (leprosy or sensory neuropathy), and patients with physical and mental disabilities (eg, debility due to critical illness, dementia, mental retardation, or Down syndrome).1,2 Most of the lesions were crusted in the present patient. Some patients experience no itching; however, about 50% of patients report itching of varying severity.1,7–9 Patients with a history of long-term drug use have fewer complaints. On physical examination, the skin contained generalized multiple hyperpigmented macules, erythematous papules, excoriations, erosions, scales, and crusts. This is consistent with the theory that the initial lesions in Norwegian scabies are poorly circumscribed, erythematous patches that rapidly develop into diffuse hyperkeratotic plaques, especially in the palmoplantar region.7,8 These symptoms may be accompanied by generalized erythema and scaling on the face, neck, scalp, and trunk, with the appearance of erythroderma.9,10 Nail abnormalities, such as hyperkeratotic or dystrophic nails, and an accumulation of thick, psoriasis-like scales under the nails, are characteristic features of this disease. Mites often survive on the subungual material, which increases the risk of re-infestation.11 The emergence of clinical manifestations of crustacean scabies is based on the ability of the natural, cellular, and humoral immune response to fight against the mite antigens.11,12 The failure of the immune response to suppress the proliferation of mites causes classic scabies to develop into crusts. Bullous scabies is characterized by the existence of various inflammatory infiltrates, mainly neutrophil or eosinophilic spongiosis, or both, with subepidermal cleavage, and intraepidermal blisters have also been reported.13,14 This pathological feature is similar to bullous pemphigoid, which can sometimes be found with the appearance of scabies, mites, and bullae.13,14 Based on the history, dermatological physical examination, and investigations, the diagnosis in this patient was Norwegian scabies and bullous scabies. Patients with bullous scabies are often misdiagnosed with bullous pemphigoid. It is clinically difficult to differentiate between bullous pemphigoid and bullous scabies; in these patients, the disease cannot be diagnosed early.13,15
The main goals of scabies therapy are to find the most appropriate scabicidal agents for the patient, simultaneously treat close-contact persons, environmental decontamination, and symptomatic treatment.13 The choice of therapy depends on the effectiveness, toxicity, type of scabies, and age of the patient.13 In this case, the patient was treated with ivermectin 24 mg/day and permethrin lotion 5% as anti-scabicidal agent which were in accordance with the Centers for Disease Control and Prevention (CDC) recommendations. The CDC recommendation for the treatment of crusted and bullous scabies is a combination of oral ivermectin and a topical scabicidal agent (permethrin or benzyl benzoate) with a topical keratolytic agent.13 Oral ivermectin is administered in five doses (on days 1, 2, 8, 9, and 15) or seven doses (added on days 22 and 29) for severe cases.13,14 In the treatment of bullous scabies, topical gamma benzene hexachloride, sulfur ointment/cream, malathion, benzyl benzoate, oral permethrin or ivermectin, or topical ointment combined with oral ivermectin have also been used in some studies.13,15 This patient also received antibiotics including ceftriaxone 1 g/12 hours, clindamycin 2×300 mg, and topical mupirocin. On the pus culture examination, K. kristinae was found, which indicated a secondary infection in the patient. Secondary infections by bacteria should be treated with the appropriate antibiotics, and if septicemia develops, aggressive treatment with broad-spectrum antibiotics is required.2 Antihistamines, keratolytic agents, topical and systemic corticosteroids, and emollients were given as the symptomatic therapy. Based on the literature, a short course of oral steroid therapy is required in some cases of bullous scabies.14 Oral corticosteroid administration in this case was based on the pathogenesis of bullous scabies; bullae appear due to a type 1 immune response to antigens from the saliva of the mite. It is likely that the development of bullous allergy in scabies lesions is a hypersensitivity reaction to mite bites mediated by immunoglobulin E (IgE).14,15 Topical anti-scabicidal therapy can cause skin irritation and xerosis; therefore, it should be followed by the administration of emollients.10,11
The prognosis for this patient in terms of quo ad vitam, quo ad functionam, and quo ad sanationam was dubia ad bonam. Prognosis in this case was closely related to treatment and various factors that supported the patient’s recovery.13 Because this disease takes a long time to heal and the recurrence rate is high, patience and compliance are needed for successful treatment.
Conclusion
The combination of crusted scabies (Norwegian scabies) and bullous scabies is rare. Combination treatment with topical and systemic anti-scabicidal agents produced satisfactory results.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kang S, Amagai M, Bruckner AL, et al. Fitzpatrick’s Dermatology.
2. Talaga-Cwiertnia K. Sarcoptes infestation. What is already known, and what is new about scabies at the beginning of the third decade of the 21st century? Pathogens. 2021;10(7):868. doi:10.3390/pathogens10070868
3. Thomas C, Coates SJ, Engelman D, Chosidow O, Chang AY. Ectoparasites: scabies. J Am Acad Dermatol. 2020;82(3):533–548. doi:10.1016/j.jaad.2019.05.109
4. Su W, Fang S, Chen A, Shan K. A case of crusted scabies combined with bullous scabies. Exp Ther Med. 2015;10:1533–1535. doi:10.3892/etm.2015.2668
5. Karthikeyan K. Crusted scabies. Indian J Dermatol Venereol Leprol. 2009;75(4):340–347. doi:10.4103/0378-6323.53128
6. Golant AK, Levitt JO. Scabies: a review of diagnosis and management based on mite biology. Am Acad Pediatr. 2012;33(1):e1–e12.
7. Subramaniam G, Kaliapurumal K, Duraipandian J, Rengasamy G. Norwegian scabies in malnourished young adult: a case report. J Infect Dev Ctries. 2010;4(5):349–351. doi:10.3855/jidc.578
8. Rose W, Rajendran G, Peter J. Crusted scabies. Indian Pediatr. 2014;51(8):680.
9. Matsura H, Senoo A, Saito M, Fujimoto Y. Norwegian scabies. Cleve Clin J Med. 2019;86(3):163–164. doi:10.3949/ccjm.86a.18081
10. Thomas J, Peterson GM, Walto SF, Carson CF, Naunton M, Baby KE. Scabies: an ancient global disease with a need for new therapies. BMC Infect Dis. 2015;15(1):250. doi:10.1186/s12879-015-0983-z
11. Apap C, Piscopo T. Crusted (Norwegian) scabies treated with oral ivermectin: a case report and overview. Malta Med J. 2012;25(4):49–53.
12. Id TH, Krause VL, Id CJ, Id BJC. Crusted scabies; a 2-year prospective study from the Northern Territory of Australia. PLoS Negl Trop Dis. 2020;14(12):e0008994. doi:10.1371/journal.pntd.0008994
13. Centers for Disease Control and Prevention. Scabies. Centers for Disease Control and Prevention; 2010. Available from: https://www.cdc.gov/parasites/scabies/index.html.
14. Maan M, Sohail A, Arif M. Bullous scabies: a case report and review of the literature. BMC Res Notes. 2015;8(1):1–4. doi:10.1186/1756-0500-8-1
15. Li FZ, Jia M, Chen KJ, Ye Q, Fang S. Bullous scabies: clinical, dermoscopic, and pathologic characteristics of ten patients. Am J Trop Med Hyg. 2021;105(6):1798–1802. doi:10.4269/ajtmh.21-0516
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

