Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Co-existence of COPD and bronchiectasis: a risk factor for a high ratio of main pulmonary artery to aorta diameter (PA:A) from computed tomography in COPD patients
Authors Dou S , Zheng C, Ji X, Wang W, Xie M , Cui L , Xiao W
Received 5 November 2017
Accepted for publication 17 January 2018
Published 26 February 2018 Volume 2018:13 Pages 675—681
DOI https://doi.org/10.2147/COPD.S156126
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chunxue Bai
Shuang Dou,1 Chunyan Zheng,1 Xiuli Ji,2 Wei Wang,1 Mengshuang Xie,1 Liwei Cui,1 Wei Xiao1
1Department of Pulmonary Medicine, Qilu Hospital, Shandong University, Jinan, People’s Republic of China; 2Department of Pulmonary Disease, Jinan Traditional Chinese Medicine Hospital, Jinan, People’s Republic of China
Background: Pulmonary vascular disease, especially pulmonary hypertension, is an important complication of COPD. Bronchiectasis is considered not only a comorbidity of COPD, but also a risk factor for vascular diseases. The main pulmonary artery to aorta diameter ratio (PA:A ratio) has been found to be a reliable indicator of pulmonary vascular disease. It is hypothesized that the co-existence of COPD and bronchiectasis may be associated with relative pulmonary artery enlargement (PA:A ratio >1).
Methods: This retrospective study enrolled COPD patients from 2012 through 2016. Demographic and clinical data were collected. Bhalla score was used to determine the severity of bronchiectasis. Patient characteristics were analyzed in two ways: the high (PA:A >1) and low (PA:A ≤1) ratio groups; and COPD with and without bronchiectasis groups. Logistic regression analysis was used to assess risk factors for high PA:A ratios.
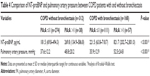
Results: In this study, 480 COPD patients were included, of whom 168 had radiographic bronchiectasis. Patients with pulmonary artery enlargement presented with poorer nutrition (albumin, 35.6±5.1 vs 38.3±4.9, P<0.001), lower oxygen partial pressure (74.4±34.5 vs 81.3±25.4, P<0.001), more severe airflow obstruction (FEV1.0, 0.9±0.5 vs 1.1±0.6, P=0.004), and a higher frequency of bronchiectasis (60% vs 28.8%, P<0.001) than patients in the low ratio group. Patients with both COPD and bronchiectasis had higher levels of systemic inflammation (erythrocyte sedimentation rate, P<0.001 and fibrinogen, P=0.006) and PA:A ratios (P<0.001). A higher PA:A ratio was significantly closely correlated with a higher Bhalla score (r=0.412, P<0.001). Patients with both COPD and bronchiectasis with high ratios presented higher levels of NT-proBNP (P<0.001) and systolic pulmonary artery pressure (P<0.001). Multiple logistic analyses have indicated that bronchiectasis is an independent risk factor for high PA:A ratios in COPD patients (OR =3.707; 95% CI =1.888–7.278; P<0.001).
Conclusion: Bronchiectasis in COPD has been demonstrated to be independently associated with relative pulmonary artery enlargement.
Keywords: COPD, bronchiectasis, main pulmonary artery to aorta diameter ratio, pulmonary vascular disease, CT
Introduction
Pulmonary vascular disease is a common comorbidity of end-stage COPD and a common cause of poor prognosis. Approximately 50% of patients with severe COPD develop pulmonary hypertension (PH),1 while out-of-proportion PH was also noted in patients with mild airflow obstruction.2 PH has been found to be associated with increased risk of exacerbation and death of COPD.3,4 It also places a huge economic burden on patients.5 This indicates that insight into the pulmonary vascular disease of COPD patients is of major importance.
With the extensive use of high-resolution computed tomography (HRCT), the presence of bronchiectasis, a previously unrecognized comorbidity, has been identified.6 The prevalence of bronchiectasis ranged from 4% to 57% in COPD patients.7,8 Patients with both COPD and bronchiectasis experience more frequent exacerbations and have a worse health status.9 The occurrence of bronchiectasis was based on the destruction of the airway wall, which also combined with repair and remodeling of the vascular bed. Recently, there has been increased interest in the relationship between bronchiectasis and vascular diseases.10–12 Bronchiectasis was recognized as a risk factor for vascular diseases,10 and PH was demonstrated to be a prognostic indicator of bronchiectasis patients.12 Possible mechanisms underlying the process include hypoxia, systemic inflammation, and arterial stiffness.10 In theory, there may be a close crosstalk between bronchiectasis and pulmonary vascular disease. Given this, we here assumed that the co-existence of COPD and bronchiectasis may be a risk factor for pulmonary vascular disease.
The main pulmonary artery to aorta diameter ratio (PA:A ratio) has been shown to be a reliable index of pulmonary vascular disease4 and a predictor of frequent exacerbations of COPD.4,13 Patients with PA:A ratios of more than 1 were recognized as having relative pulmonary artery enlargement. They were characterized with impaired physical activity14 and PH.15 However, it remains unknown which characteristic of COPD patients is the risk factor for relative pulmonary artery enlargement.
In the present study, we hypothesized that COPD-bronchiectasis co-existence patients would be the risk population for relative pulmonary artery enlargement.
Methods
Study population
Patients who attended Qilu Hospital of Shandong University from April 2012 to December 2016 were retrospectively reviewed. COPD was diagnosed based on Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines,16 with respiratory symptoms, physical signs, and persistent airflow limitation (post-BD FEV1/FVC <0.70). Patients with HRCT scans and pulmonary function tests of stable state within 12 months were included. Patients with other respiratory diseases influencing the incidence of pulmonary vascular enlargement, such as interstitial lung disease and pulmonary thromboembolism, were excluded from the study. Other exclusion criteria included asthma, thoracic pleural disease, community-acquired pneumonia, or pulmonary masses >3 cm on a chest CT. All of the demographic and clinical characteristics were collected, including age, gender, smoking history, history of illness, comorbidities, peripheral blood tests (PH value, PaO2, PaCO2, white blood cells, neutrophils, eosinophils, albumin (ALB), erythrocyte sedimentation rate (ESR), fibrinogen, and N-terminal pro-B-type natriuretic peptide), HRCT scans, systolic pulmonary arterial pressure of echocardiography, and pulmonary function test data.
The study was approved by the Ethics Committee of our hospital, Qilu Hospital of Shandong University (approval number: 2015091). The data were anonymous, and retrospective, the Ethics Committee of Qilu Hospital of Shandong University agreed that written informed consent from participants was not required.
Pulmonary function testing (PFT)
A computerized spirometer (MasterScreen, Jaeger, Hoechberg, Germany) was used for PFT, according to recommendations issued by the American Thoracic Society and European Respiratory Society (ATS/ERS).17 Basic information (age, height, and weight) and spirometry parameters (FVC, FEV1.0, and FEV1.0/FVC) were collected.
HRCT scan
Chest HRCT scans were performed on a 64-slice spiral CT scanner (SOMATOM Definition AS, Siemens Healthcare, Erlangen, Germany) at full inspiration. Tube voltage was 120 kV and tube current varied between 20 and 500 mA by automatic regulation. All scans were acquired using the standard parameters: 0.5 s rotation time and 512×512 pixels. Consecutive images with a 1 mm slice thickness were reconstructed.
Diagnosis and assessment of bronchiectasis
The presence of bronchiectasis was confirmed by an experienced respiratory radiologist and a respiratory physician, according to criteria published by Naidich et al:20 (1) lack of tapering of bronchi, (2) dilation of bronchi when the internal diameter was larger than that of the adjacent pulmonary artery, or (3) visualization of the peripheral bronchi within 1 cm of the costal pleural surface or adjacent mediastinal pleural surface.18–20 The severity of bronchiectasis was evaluated using Bhalla score,21 which analyzed nine radiological characteristics of the lesions. Lingula was considered an independent lobe. Bronchiectasis in a single pulmonary segment was not included because it could appear in healthy individuals.8 Bronchiectasis occurring before age 40 was also excluded from the group.
PA:A ratio measurements
The PA:A ratio was measured using previously widely used methods.4,22–24 Briefly, pulmonary artery (PA) and aorta (A) diameters were measured at the same level of pulmonary artery bifurcation. The PA diameter was perpendicular to the long axis of the pulmonary artery at the tangent of PA and A, with two perpendicular lines averaged for the A diameter by use of a CT scale. In order to collect accurate data, two blinded reviewers worked independently. As in previous reports,4,23 PA:A ratios of more than 1 were considered high.
Statistical analysis
Statistical analyses were performed using SPSS version 19.0 (IBM Corporation, Armonk, NY, USA). Data are presented as mean ± SD for continuous variables and as a percentage for categorical variables. The Student’s t-test was used for normally distributed values and Mann–Whitney U-test was used for non-normally distributed values. Quantitative data from three or more groups were compared using Kruskal–Wallis test followed by Bonferroni correction. Considering categorical variables, the chi-square test was used to determine statistical differences. The Pearson’s r coefficient was used to evaluate the linear correlation between severity of bronchiectasis and PA:A ratios. Multivariate logistic regression analysis was used to identify predictive values for PA:A ratios >1. Variables found to be statistically significant in bivariate analysis and those of clinical interest were included in the multivariate analysis. P<0.05 was considered statistically significant.
Results
Baseline characteristics of the study population
A total of 480 COPD patients were included in this study. Mean age was 69.5±9.6 years, and approximately 76% of the patients were male. Of all the subjects, 70.6% were smokers or ex-smokers. Mean FEV1, FVC, and FEV1/FVC were 1.1 L, 2.2 L, and 50.0%, respectively. In this study population, there were 168 (35%) patients with radiographic bronchiectasis. Other clinical characteristics are shown in Table 1.
Comparisons of clinical features between patients with and without relative pulmonary artery enlargement
As previously reported,4,23,25 a PA:A ratio >1 was designated as relative pulmonary artery enlargement. Out of the 480 patients with measurable CT ratios, 95 were in the high ratio group, and the others were in the low ratio one. Patients with relative pulmonary artery enlargement were more likely to be younger (P=0.003) and female (P<0.001) and had fewer pack-years of smoking (P=0.016). These patients also presented with lower levels of PaO2 (P<0.001), higher levels of PaCO2 (P<0.001), and worse nutrition (ALB, 35.6±5.1 vs 38.3±4.9, P<0.001). Considering the pulmonary function test, patients with a PA:A ratio of more than 1 had worse pulmonary function parameters, including FVC (P=0.003), FEV1.0 (P=0.004), and FEV1% predicted (P=0.008). As for underlying diseases, the high PA:A ratio group had more patients with bronchiectasis (60% vs 28.8%, P<0.001) and diabetes mellitus (23.2% vs 8.6%, P<0.001). With respect to CT measurement data, the PA (P<0.001) and PA:A ratio (P<0.001) were absolutely larger in the high ratio group, regardless of the slightly shorter A diameter (Table 2).
Clinical characteristics of the study population with bronchiectasis
Of all the subjects in our study, 168 had the diagnosis of bronchiectasis, and the other 312 did not. Clinical characteristics are shown in Table 3. Compared with patients without bronchiectasis, patients with both conditions were less likely to be current or former smokers (P=0.026) and under a worse nutritional status (ALB, P<0.001). These patients also presented with higher peripheral levels of ESR (P<0.001) and fibrinogen (P=0.006), which suggested greater systemic inflammation. CT signs of pulmonary vascular changes were significantly different. PA (32.5±5.7 vs 30.0±5.6, P<0.001) and PA:A ratios (0.95±0.17 vs 0.83±0.15, P<0.001) were greater in patients with bronchiectasis, despite the slightly shorter aorta diameter observed in this group. Besides that, the proportion of sex, BMI (body mass index), and impairment of pulmonary function did not show prominent differences between two groups.
The Balla score was used to quantify the severity of bronchiectasis in this study. As shown in Figure 1, correlation analysis showed that PA:A ratios increased as the Balla score increased (r=0.412, P<0.001). The NT-proBNP and pulmonary artery pressure of echocardiography were more severe in COPD-bronchiectasis co-existence patients who had high ratios than those who had lower ratios (Table 4).
  | Figure 1 The association between the severity of bronchiectasis and PA:A ratio in COPD-bronchiectasis co-existence patients. |
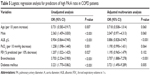
Logistic regression analysis of the risk factors of the PA:A ratio
Seven variables (age, sex, ALB, PaO2, FEV1% predicted, bronchiectasis, and diabetes mellitus) were included in the logistic regression analysis (Table 5). Multivariate logistic regression analysis showed that bronchiectasis (OR =3.707; 95% CI =1.888–7.278; P<0.001) and diabetes mellitus (OR =3.721; 95% CI =1.490–9.289; P=0.005) correlated with a PA:A ratio of more than 1 in COPD patients. COPD patients with better nutrition (higher level of ALB) were more likely to have low PA:A ratios.
Discussion
To the best of our knowledge, this is the first report to establish a relationship between bronchiectasis and the marker of pulmonary vascular disease in COPD patients. In this study, COPD patients with concomitant radiographic bronchiectasis were demonstrated to be at increased risk of relative pulmonary artery enlargement, regardless of the severity of spirometry impairment.
PA:A ratio, the ratio of the diameter of the pulmonary artery to that of the aorta, is a remarkable marker indicating pulmonary vascular disease, especially PH.15,22,23 Unlike right heart catheterization and echocardiography, the PA:A ratio is recorded as a reproducible and reliable measurement.4,26 A PA:A ratio of more than 1 is considered an independent predictor of mortality in COPD patients,27 and these patients tend to have worse airflow obstruction and suffer exacerbation more frequently.4,13 It has been reported that about 5%–50% of COPD patients have PH.28 In addition, the prevalence of cardiovascular disease in COPD patients was 20%–22%, and 13%–28% deaths were cardiac-related.5 The significance of focusing on the PA:A ratio might lie in the ability to identify patients at risk of pulmonary vascular disease or cardiac-related exacerbations.4
PA and A diameters may also correlate with age, causing a decrease in PA:A ratio with aging. In our study, patients with relative pulmonary artery enlargement tended to be younger than patients without (66.8±9.5 vs 70.1±9.5, P=0.003). However, when we focused on the influence that bronchiectasis had on the PA:A ratio in COPD patients, age showed no significant difference between the two groups (P=0.188). Bronchiectasis was still the risk factor for high PA:A ratios in COPD patients after adjusting for confounding factors, including age.
This is the first study to explore whether bronchiectasis in COPD patients is a risk factor for high PA:A ratios. Although the co-existence of COPD and bronchiectasis has recently been recognized as an overlap syndrome, it is still not clear how bronchiectasis participates in the development of COPD progress and vice versa. Recently, researchers have reported that the severity of bronchiectasis was independently associated with the development of vascular diseases.10,12 Thus, it is intriguing to illustrate the impact that bronchiectasis had on pulmonary vascular disease in COPD patients.
The mechanism underlying pulmonary vascular disease in patients with both COPD and bronchiectasis has not been elucidated clearly. Hypoxia has been recognized as an important cause.29 COPD patients often require increasing oxygen when conditions deteriorate, and bronchiectasis might exacerbate this situation. The poorer pulmonary ventilation and gas exchange in overlap patients render them more susceptible to PH. Inevitably, patients with overlap syndrome suffer not only from impairment of the parenchyma, but also destruction of the airway wall, both of which can destroy the vascular bed and induce hemodynamic alterations.30,31
Nowadays, endothelial dysfunction has been recognized as a major mechanism underlying chronic pulmonary and vascular disease.28 COPD patients with concomitant bronchiectasis have been reported to have higher levels of inflammation in the airway and peripheral blood,32 which might influence the blood vessel endothelium. In this study, COPD and bronchiectasis co-existence patients had higher levels of peripheral ESR and fibrinogen, which reflected the higher level of systemic inflammation. This might destroy the microenvironment and function of endothelial cells, resulting in imbalanced release of vasoactive mediators.28 This is in accordance with the newly proposed concept of “sick lung circulation”.33,34 Information from the sick lung is transported to the myocardium via blood circulation, which, thus, brings about physical dysfunction of the heart, such as abating systolic function. Right heart dysfunction, in turn, causes congestion of pulmonary circulation, and PH may eventually develop. Studies examining the information from the affected lungs of patients with both COPD and bronchiectasis, including levels of cytokine, microRNA, and microparticles, should be encouraged.33
Despite regular assessment of pulmonary function and airway inflammation, clinicians should pay attention to the impact that bronchiectasis has on vascular disease in COPD patients. More prospective studies are needed to define the significance of high PA:A ratios in patients with COPD and bronchiectasis.
Limitations
The present study has some limitations. First, because right heart catheterization is not a regular test for COPD patients, it is not possible to confirm that patients with high PA:A ratios actually have PH. However, regardless of whether they have PH, COPD patients with PA:A ratios of more than 1 tend to experience poor outcomes.4 This makes it important to focus on patients at risk for relative pulmonary artery enlargement. Second, as a retrospective study, information about bacterial infection, long-term prognosis, and history of exacerbation of COPD-bronchiectasis co-existence patients with high PA:A ratios was absent. Future prospective studies focusing on these aspects and a large population of patients with both stable and exacerbated conditions are needed. Third, these results showed that diabetes mellitus might also influence the PA:A ratio, which was not the main focus of the current study. Future studies focusing on the impact that diabetes mellitus has on pulmonary vascular disease in COPD patients are also needed.
Conclusion
COPD and bronchiectasis co-existence subjects are considered at risk for relative pulmonary artery enlargement (PA:A ratio >1). Future comprehensive assessment should pay close attention to the prevalence of and mechanisms underlying pulmonary vascular disease in patients with COPD and concomitant bronchiectasis.
Acknowledgments
This work was supported by the National Natural Science Foundation of the People’s Republic of China (No 81370148).
Disclosure
The authors report no conflicts of interest in this work.
References
Thabut G, Dauriat G, Stern JB, et al. Pulmonary hemodynamics in advanced COPD candidates for lung volume reduction surgery or lung transplantation. Chest. 2005;127(5):1531–1536. | ||
Chaouat A, Naeije R, Weitzenblum E. Pulmonary hypertension in COPD. Eur Respir J. 2008;32(5):1371–1385. | ||
Hurdman J, Condliffe R, Elliot CA, et al. ASPIRE registry: assessing the Spectrum of Pulmonary hypertension Identified at a REferral centre. Eur Respir J. 2012;39(4):945–955. | ||
Wells JM, Washko GR, Han MK, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367(10):913–921. | ||
Decramer M, Janssens W. Chronic obstructive pulmonary disease and comorbidities. Lancet Respir Med. 2013;1(1):73–83. | ||
O’Brien C, Guest PJ, Hill SL, Stockley RA. Physiological and radiological characterisation of patients diagnosed with chronic obstructive pulmonary disease in primary care. Thorax. 2000;55(8):635–642. | ||
Agusti A, Calverley PM, Celli B, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122. | ||
Martínez-García MA, Soler-Cataluña JJ, Donat Sanz Y, et al. Factors associated with bronchiectasis in patients with COPD. Chest. 2011;140(5):1130–1137. | ||
Gatheral T, Kumar N, Sansom B, et al. COPD-related bronchiectasis; independent impact on disease course and outcomes. COPD. 2014;11(6):605–614. | ||
Evans IE, Bedi P, Quinn TM, Hill AT. Bronchiectasis severity is an independent risk factor for vascular disease in a bronchiectasis cohort. Chest. 2017;151(2):383–388. | ||
Öcal S, Portakal O, Öcal A, Demir AU, Topeli A, Çoplü L. Factors associated with pulmonary hypertension and long-term survival in bronchiectasis subjects. Respir Med. 2016;119:109–114. | ||
Devaraj A, Wells AU, Meister MG, Loebinger MR, Wilson R, Hansell DM. Pulmonary hypertension in patients with bronchiectasis: prognostic significance of CT signs. AJR Am J Roentgenol. 2011;196(6):1300–1304. | ||
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2017. Available from: http://goldcopdorg. Accessed January 13, 2017. | ||
Chung KS, Kim YS, Kim SK, et al. Functional and prognostic implications of the main pulmonary artery diameter to aorta diameter ratio from chest computed tomography in Korean COPD patients. PLoS One. 2016;11(5):e0154584. | ||
Wells JM, Dransfield MT. Pathophysiology and clinical implications of pulmonary arterial enlargement in COPD. Int J Chron Obstruct Pulmon Dis. 2013;8:509–521. | ||
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2012. Available from: http://wwwgoldcopdorg/. Accessed June 20, 2012. | ||
Laszlo G. Standardisation of lung function testing: helpful guidance from the ATS/ERS Task Force. Thorax. 2006;61(9):744–746. | ||
Martínez-García MA, de la Rosa Carrillo D, Soler-Cataluña JJ, et al. Prognostic value of bronchiectasis in patients with moderate-to-severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(8):823–831. | ||
Mao B, Lu HW, Li MH, et al. The existence of bronchiectasis predicts worse prognosis in patients with COPD. Sci Rep. 2015;5:10961. | ||
Naidich DP, McCauley DI, Khouri NF, Stitik FP, Siegelman SS. Computed tomography of bronchiectasis. J Comput Assist Tomogr. 1982;6(3):437–444. | ||
Bhalla M, Turcios N, Aponte V, et al. Cystic fibrosis: scoring system with thin-section CT. Radiology. 1991;179(3):783–788. | ||
Ng CS, Wells AU, Padley SP. A CT sign of chronic pulmonary arterial hypertension: the ratio of main pulmonary artery to aortic diameter. J Thorac Imaging. 1999;14(4):270–278. | ||
Iyer AS, Wells JM, Vishin S, Bhatt SP, Wille KM, Dransfield MT. CT scan-measured pulmonary artery to aorta ratio and echocardiography for detecting pulmonary hypertension in severe COPD. Chest. 2014;145(4):824–832. | ||
Ortaç Ersoy E, Durusu Tanriover M, Öcal S, Gulsun Akpinar M, Topeli A. Measurement of pulmonary artery to aorta ratio in computed tomography is correlated with pulmonary artery pressure in critically ill chronic obstructive pulmonary disease patients. J Crit Care. 2016;33:42–46. | ||
Wells JM, Morrison JB, Bhatt SP, Nath H, Dransfield MT. Pulmonary artery enlargement is associated with cardiac injury during severe exacerbations of COPD. Chest. 2016;149(5):1197–1204. | ||
Devaraj A, Wells AU, Meister MG, Corte TJ, Wort SJ, Hansell DM. Detection of pulmonary hypertension with multidetector CT and echocardiography alone and in combination. Radiology. 2010;254(2):609–616. | ||
Shin S, King CS, Brown AW, et al. Pulmonary artery size as a predictor of pulmonary hypertension and outcomes in patients with chronic obstructive pulmonary disease. Respir Med. 2014;108(11):1626–1632. | ||
Blanco I, Piccari L, Barberà JA. Pulmonary vasculature in COPD: the silent component. Respirology. 2016;21(6):984–994. | ||
Barberà JA. Mechanisms of development of chronic obstructive pulmonary disease-associated pulmonary hypertension. Pulm Circ. 2013;3(1):160–164. | ||
Alzeer AH, Al-Mobeirek AF, Al-Otair HA, Elzamzamy UA, Joherjy IA, Shaffi AS. Right and left ventricular function and pulmonary artery pressure in patients with bronchiectasis. Chest. 2008;133(2):468–473. | ||
Dournes G, Laurent F, Coste F, et al. Computed tomographic measurement of airway remodeling and emphysema in advanced chronic obstructive pulmonary disease. Correlation with pulmonary hypertension. Am J Respir Crit Care Med. 2015;191(1):63–70. | ||
Ni Y, Shi G, Yu Y, Hao J, Chen T, Song H. Clinical characteristics of patients with chronic obstructive pulmonary disease with comorbid bronchiectasis: a systemic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2015;10:1465–1475. | ||
Voelkel NF, Gomez-Arroyo J, Mizuno S. COPD/emphysema: the vascular story. Pulm Circ. 2011;1(3):320–326. | ||
Voelkel NF, Natarajan R, Drake JI, Bogaard HJ. Right ventricle in pulmonary hypertension. Compr Physiol. 2011;1(1):525–540. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.