Back to Journals » Open Access Surgery » Volume 14
Closed Technique with Suction Drain versus Partial Closure Technique in Midline Repair of Pilonidal Sinus: A Comparative Study
Authors Aly Khalil A , Elshawy M , Elbarbary M, Elghamrini Y
Received 24 February 2021
Accepted for publication 20 April 2021
Published 10 May 2021 Volume 2021:14 Pages 21—27
DOI https://doi.org/10.2147/OAS.S308212
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Luigi Bonavina
Ahmed Aly Khalil, Mohamed Elshawy, Mohab Elbarbary, Yasser Elghamrini
Department of General Surgery, Faculty of Medicine, Ain Shams University, Cairo, Egypt
Correspondence: Ahmed Aly Khalil
Department of General Surgery, Faculty of Medicine, Ain Shams University, Cairo, Egypt
Email [email protected]
Background: Pilonidal sinus (PNS) is a common disorder that mainly affects young adults. It can be asymptomatic or presented by discomfort, inflammation, abscess or sinus formation. Despite current advances in surgical techniques, the best option to treat PNS is not yet well defined. Many studies reported techniques that involved excision of the sinus and closure of the deep and superficial layers but leaving the skin open.
Aim: We aim to compare between the excision and primary midline closure with suction drain versus the partial closure technique as treatment options for PNS in terms of recovery, wound complications and recurrence rate.
Patients and Methods: A prospective comparative study at Ain Shams University Hospitals that included 80 patients with PNS was conducted from January 2018 to June 2019. They were divided randomly into group A; 40 patients that had the midline closed method with suction drain and group B; 40 patients that underwent the partial closure technique. Both groups were followed up for 1 year, detecting healing time, wound complications, return to usual activities and recurrence rate.
Results: We detected significant differences between both groups as regards to pain and discomfort postoperatively, favoring the partial closure group. Mean time to wound healing was significantly shorter among group A (14.43 ± 3.13) though mean time of return to usual activities was faster among the partial closure group (14.45 ± 1.15). There were no statistically significant differences between both groups as regards to wound infection, dehiscence or hematoma formation. Wound seroma was more among group A.
Conclusion: The partial midline closure technique showed comparable results to the closed method with suction drain in management of PNS disease. Indeed, it shows less postoperative complications and a faster return to usual daily activity. Yet, more studies are required to demonstrate its reproducibility.
Keywords: pilonidal sinus, primary midline closure, partial closure, wound complications
Introduction
Chronic pilonidal sinus (PNS) is a common disorder that affects mainly young adults. Due to different hair characteristics and growth patterns, PNS has a higher incidence in some countries, particularly in the Middle East and Gulf region.1 Some theories suggested that it results from the invasion of fallen hair into the skin.2 It can be asymptomatic or presented by discomfort, inflammation, abscess or sinus formation.3
There are several surgical procedures described for the treatment of PNS including incision and drainage, excision and healing by second intention excision4 and primary closure or excision with reconstructive flap techniques.5 Less commonly described techniques include cryosurgery, phenol injection6 and electrocauterization.7 Despite the current advances in surgical techniques, the best surgical technique to treat PNS is not yet well defined. However characteristics of the ideal operation should also be simple, require a short hospitalization stay and allow rapid return to usual daily activities.8 Nada et al had a new vision in the surgical management of PNS. In their report, they described a technique that involved excision of the sinus and side tracts then elevating flaps over the glutei and subsequent closure of the deep layer as well as approximating the superficial subcutaneous layer. They left the skin open.9
The aim of our study was to compare between the excision and primary midline closure (closed method) with applying suction drain versus the partial midline closure technique. We evaluated the efficacy of the two techniques in management of pilonidal sinus disease in terms of recovery, wound complications and recurrence rate.
Patients and Methods
We conducted a prospective comparative study at Ain Shams University Hospital in Egypt that included eighty patients with pilonidal sinus disease from January 2018 to June 2019. The patients were 67 males and 13 females with an age range from 16 to 43 years. An approval, from the ethical committee of the Faculty of Medicine, Ain Shams University was obtained and the study was conducted in accordance to the Declaration of Helsinki. The procedure was clearly explained to the patients with preoperative written informed consent as well. A parent or guardian of patients under 18 years old provided an informed consent to participate in the study. All the patients were presented by chronic non-recurrent uncomplicated PNS at the time of operation, classified as type III or IV by Tezel classification. The mean duration of the disease prior to surgery was 1.6 years. Patients with complicated PNS as abscess formation, fistulous tract communicating with the anorectal canal or suspected malignant transformation were excluded.
The patients were randomly divided into two equal groups; group (A) underwent the closed midline closure technique with the application of a suction drain. Group (B) underwent the partial midline closure technique. Randomization was done by the closed envelop method. The patients were followed up for one year assessing wound complications and recurrence.
All patients were evaluated by a complete patient history and clinical examination. Baseline labs were performed on all patients including complete blood picture (CBC), baseline chemistry including hepatitis markers and blood urea/glucose levels and coagulation profile. Chest X-ray and electrocardiography (ECG) were done if the patient's age was more than 40 years. Intra-operatively, IV 3rd generation Cephalosporin was given. Patients were positioned in a prone position after taking general (57%) or spinal (43%) anesthesia. For good exposure of the inter gluteal region, lateral traction from the lateral margin of the gluteus using adhesive tape was performed. Disinfection using 10% povidone-iodine was done.
Group A (Closed Midline Technique with Suction Drain)
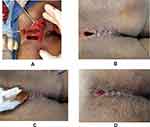
After visualization of all the sinus orifices, probing was done. Laying open the main tract and then all the visualized side tracts was made. Full excision around and just below the whole laid open tracts was done till the underneath healthy sacrococcygeal fascia was reached. Complete hemostasis was achieved using diathermy. Irrigation by normal saline was done. A high vacuum suction drain was placed in the wound cavity and was fixed out on the side of the main wound. Closure of the deep layer is started by interrupted stitches using absorbable stitch material through the deep subcutaneous fat and fascia elevated on both sides together with the central fascia over the sacrum to decrease the dead space. Finally, stitches were taken to approximate the superficial subcutaneous fat then the skin was closed using non absorbable polyproline stitch materials (Figure 1A–D).
Group B (Partial Midline Closure Technique)
Excision of the track was performed, ensuring good hemostasis as before. Closure of the deep layers was done using interrupted absorbable stitches approximating the subcutaneous tissue together except one end of the wound was left without closure. Then skin was closed with interrupted non-absorbable stitches leaving the same end without skin closure so that we obtained a wound with an open tunnel to be used for drainage and irrigation. There was application of a sterile pack in the open part of the wound (Figure 2A–D).
All Patients of both groups were discharged on postoperative day one and were followed-up once per week for 4 weeks and then after 3, 6 and 12 months from the operation. At each visit, wound examination was performed to assess postoperative pain, progression of wound healing, postoperative complications and recurrence. The early postoperative complications were assessed including postoperative bleeding, seroma, wound infection, wound dehiscence and hematoma formation. Recurrence rate among both groups was assessed clinically. Return to usual daily activities was compared between both groups.
For group A, the drain was removed on the 7th to 14th postoperative day. Removal of the sutures was done after 2–3 weeks if there were no wound complications. Postoperative pain was assessed via VAS on the 1st, 6th and 10th postoperative days. Postoperative seroma was assessed by soaked gauze during daily dressings; no seroma upon pressure over the wound indicated a clean wound with no seroma formation. One soaked gauze during dressing was considered minimal seroma, while more than one soaked gauze was considered mild seroma.
Statistical Analysis
Recorded data were analyzed using the statistical package for social sciences, version 20.0 (SPSS Inc., Chicago, Illinois, USA). Quantitative data were expressed as mean ± standard deviation (SD). Qualitative data were expressed as frequency and percentage. P-values less than 0.05 were considered to be statistically significant.
P-value: level of significance.
P > 0.05: Non-significant (NS).
P < 0.05: Significant (S).
P < 0.01: Highly significant (HS).
Results
Eighty patients presenting with uncomplicated PNS were enrolled in our study. Demographic data of the patients are shown in Table 1. They included 67 males and 13 females who underwent surgical excision of PNS from January 2018 to June 2019 at Ain Shams University Hospital. Their ages ranged from 16 to 38 years with mean ± SD of 24.43 ± 5.03 years. Both groups had a disease duration that varied from 10 to 19 months. Twenty-four patients had prior abscess drainage yet none of them presented with local signs of infection at time of surgery. The tract had a single opening in 18 patients (22.5%) and multiple openings in 62 patients (77.5%).
 |
Table 1 Demographic Data and Duration of Symptoms of Patients in the Two Groups |
The mean operative time was 58 ± 4.49 mins (range: 51–64 minutes) in group A and 48 ± 5.06 mins (range: 41–55 minutes) in group B which was not statistically significant. No intraoperative complications occurred in all patients. The mean hospital stay was 1.2 ± 0.7 days for group A and 1.4 ± 0.6 for group B. The mean time for return to normal daily activity was significantly shorter for group B (14.45 ± 1.15 days) than for group A (22.34 ± 1.6 days). The outcome of the patients in both groups was assessed as summarized in Table 2.
 |
Table 2 Postoperative Clinical Outcome in the Two Groups |
VAS scores for pain on the 1st, 6th and 10th postoperative days showed statistically significantly more discomfort among group A. The mean time of wound healing duration was significantly shorter in group A (14.43 ± 3.13 days) than in group B (21.15 ± 4.35 days). The formation of postoperative seroma was significantly higher among group A, as 50.25% had no seroma, 28.55% had minimal seroma and 22.2% had mild seroma. In group B 67.53% had no seroma, 27.36% had minimal seroma and 6.11% had mild seroma. There was no statistically significant difference between both groups in terms of wound infection. Among group A, 4 cases (10%) had purulent discharge within 7 days, postoperatively, while there were 2 cases (5%) among group B. There was no statistically significant difference as regards wound dehiscence. It occurred in 5 cases among group A (12.5%) and 4 cases (10%) among group B. The wound dehiscence was related to either postoperative seroma or postoperative wound infection. In all cases, this was managed conservatively by frequent dressing and antibiotic treatment. After 1 year of follow up, Recurrence was found in 6 cases (15%) in group (A) compared to 5 cases (12.5%) in group (B). This rate was non-significant.
Discussion
PNS is most commonly observed in people aged 15–30 years with a 4:1 male to female ratio.10 It badly affects quality of life of the patients owing to accompanying pain, discharge and possible abscess formation. When evaluating means of age and sex between both groups, there was no statistically significant difference. The mean age of all patients was 26.43 which was close to the current literature.1,4,10
The debate on the best surgical technique of management of PNS disease is still unresolved. To minimize the incidence of recurrence, complete excision of the main tract and secondary tracts is essential.4 The ideal technique should achieve a minimal recurrence rate with better outcome results in terms of healing time, return to work and less incidence of complications.
Several reports concluded the advantages of primary midline closure in terms of quicker healing time, shorter time off work and fewer postoperative visits.11,12 However, it is associated with a higher rate of wound dehiscence due to excessive skin tension and a higher incidence of recurrence.13 Other reports advocate the lay open excision then the wound is left to granulate giving a lower rate of recurrence. However, this will lead to prolonged time of wound healing and delay in return to usual daily activity.14,15
As we mentioned, there is no consensus about the best or standard operation for PNS however, many centers all over the world adopt the flaps or lateral closure techniques as they have better outcomes in literature. In our institute, we prefer the midline closure techniques because they are easier, more cosmetic, less time consuming and have favorable outcomes in our series of patients. The main problems that we face in practicing such a technique are wound dehiscence, delayed wound healing and seroma. We believe that these issues happen due to tension with poor blood supply in the midline and high moisture in this area which is natural for its anatomical position. We assumed that making modification to the midline closure to be partial will allow better wound healing as it gives a window for drainage and irrigation, also this decreases the tension on the midline closure thus improving wound healing.
In their retrospective series, Arslan et al presented a modified primary closure technique for treatment of PNS. They reported infection, hematoma and wound dehiscence rates were 16.7%, 7.4% and 3.7%, respectively. Sahsamanis et al described a semi-closed technique for management of PNS disease. In their study on 29 patients, wound dehiscence and hemorrhage were 5.8% and 2.9%, respectively.10
Nada et al described a semi-open technique that included closure of the deep and superficial layers while left the skin opened. They reported mean postoperative hospital stay of one day and mean time of complete wound healing of about three weeks.9 In our study, we reported a similar mean time of wound healing of about 21 days in the partial closure group. However, this was statistically longer than the time to wound healing in closure methods with a suction drain.
In their study, Al-Jaberi et al stated that moderate postoperative pain had occurred after the excision and primary closure technique while moderate to severe postoperative pain was reported after the lay open technique.16 In our study, the partial closure technique reported less discomfort, a favorable VAS score for pain on the first and tenth postoperative days and better quality of life as regards comfortable sitting and early return to usual daily activities.
The development of wound seroma was higher among excision and primary closure groups than the partial closure technique which proved to be of statistical value. We believe that it is a big advantage of the partial closure technique. We found no statistically significant difference in terms of wound dehiscence, infection or hematoma formation between the two groups. All the patients with wound infection or wound dehiscence were managed conservatively with antibiotics and frequent dressing without the need for re-operating.
There was no significant difference between the 2 groups regarding recurrence. Recurrence is considered the most practical clue for operative success, especially in this type of disease as patients tolerate the nasty post-operative period hoping for complete cure. Recurrence rate was comparable with most of the published data describing similar techniques.
The ideal surgical technique for management of PNS disease should achieve minimal pain and discomfort and the best healing with least recurrence rate. In addition, it should require minimal wound care with a rapid return to usual daily activity.17
Conclusion
The partial midline closure technique in the management of PNS was found to be feasible and comfortable in our study. It showed superior results on the primary midline closure technique regarding post-operative pain and early return to daily activities with no significant difference in postoperative complications or recurrence. The partial midline closure technique seems to be fulfilling the criteria of the ideal operation for the management of PNS. More studies on bigger samples are needed to prove the efficacy and reproducibility of this technique.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Elserafy ME, Elserafy ME, Hamed HM, et al. Management of 634 consecutive patients with chronic pilonidal sinus: a nine-year experience of a single institute. Surg Sci. 2012;03:145–154. doi:10.4236/ss.2012.33029
2. Bertelsen CA. Cleft-lift operation for pilonidal sinuses under tumescent local anesthesia: a prospective cohort study of peri- and postoperative pain. Dis Colon Rectum. 2011;54:895–900. doi:10.1007/DCR.0b013e31820ee852
3. Surrell JA. Pilonidal disease. Surg Clin North Am. 1994;74:1309–1315. doi:10.1016/S0039-6109(16)46482-0
4. Lee HC, Ho YH, Seow CF, Eu KW, Nyam D. Pilonidal disease in Singapore: clinical features and management. Aust N Z J Surg. 2000;70:196–198. doi:10.1046/j.1440-1622.2000.01785.x
5. Müller K, Marti L, Tarantino I, et al. Prospective analysis of cosmesis, morbidity, and patient satisfaction following limberg flap for the treatment of sacrococcygeal pilonidal sinus. Dis Colon Rectum. 2011;54:487–494. doi:10.1007/DCR.0b013e3182051d96
6. Duchateau J, De Mol J, Bostoen H, Allegaert W. Pilonidal sinus. Excision–marsupialization–phenolization? Acta Chir Belg. 1985;325–328.
7. Shafik A. Electrocauterization in the treatment of pilonidal sinus. Int Surg. 1996;81((1)):83–84.
8. Neşşar G, Kayaalp C, Seven C. Elliptical rotation flap for pilonidal sinus. Am J Surg. 2004;187:300–303. doi:10.1016/j.amjsurg.2003.11.012
9. Nada M, Salama TMS. Pilonidal sinus excision: new vision. Surg Curr Res. 2016;6:5–7. doi:10.4172/2161-1076.1000274
10. Arslan S, Karadeniz E, Ozturk G, et al. Modified primary closure method for the treatment of pilonidal sinus pilonidal sinüs tedavisinde modifiye primer Kapama Yöntemi. Eurasian J Med. 2016. doi:10.5152/eurasianjmed.2015.0059
11. Lorant T, Ribbe I, Mahteme H, Gustafsson U-M, Graf W. Sinus excision and primary closure versus laying open in pilonidal disease: a prospective randomized trial. Dis Colon Rectum. 2011;54:300–305. doi:10.1007/DCR.0b013e31820246bf
12. Perruchoud C, Vuilleumier H, Givel JC. Pilonidal sinus: how to choose between excision and open granulation versus excision and primary closure? Study of a series of 141 patients operated on from 1991 to 1995. Swiss Surg. 2002;8:255–258. doi:10.1024/1023-9332.8.6.255
13. McLaren CA. Partial closure and other techniques in pilonidal surgery: an assessment of 157 cases. Br J Surg. 1984;71:561–562. doi:10.1002/bjs.1800710731
14. Notaras MJ. A review of three popular methods of treatment of postanal (pilonidal) sinus disease. Br J Surg. 1970;57:886–890. doi:10.1002/bjs.1800571204
15. Ortiz HH, Marti J, Sitges A. Pilonidal sinus: a claim for simple track incision. Dis Colon Rectum. 1977;20((4)):325–328. doi:10.1007/BF02586431
16. Al-Jaberi TMR. Excision and simple primary closure of chronic pilonidal sinus. Eur J Surg. 2001;167:133–135. doi:10.1080/110241501750070600
17. Darwish A, Eskandaros M, Hegab A. Sacrococcygeal pilonidal sinus: modified sinotomy versus lay-open, limited excision, and primary closure. Egypt J Surg. 2017;36:13. doi:10.4103/1110-1121.199901
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.