Back to Journals » Risk Management and Healthcare Policy » Volume 15
Clinical Nurses’ Knowledge, Attitude and Practice of Catheter-Related Thrombosis and Its Influencing Factors: A Cross-Sectional Survey
Authors Peng S, Kong X , Ma G, Hou J, Luo L, Xu R , Fan Y , Zhang J
Received 22 August 2022
Accepted for publication 18 November 2022
Published 30 November 2022 Volume 2022:15 Pages 2257—2268
DOI https://doi.org/10.2147/RMHP.S387124
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Sha Peng,1,2 Xiaoya Kong,1,2 Guiyuan Ma,1,2 Jianmei Hou,1 Lingxia Luo,1 Ran Xu,1,2 Yuhua Fan,1 Jinghui Zhang1– 3
1Teaching and Research Section of Clinical Nursing, Xiangya Hospital of Central South University, Changsha, Hunan, People’s Republic of China; 2Xiangya Nursing School, Central South University, Changsha, Hunan, People’s Republic of China; 3National Clinical Research Center for Geriatric Disorders, Xiangya Hospital of Central South University, Changsha, Hunan, People’s Republic of China
Correspondence: Jinghui Zhang, Email [email protected]
Purpose: The present study aims to evaluate the current situation of knowledge, attitude and practice of clinical nurses in catheter-related thrombosis, analyze its influencing factors, enhance the attention of nursing managers and clinical nurses about catheter-related thrombosis, and provide a basis for formulating catheter-related thrombosis training plan.
Patients and Methods: The research was conducted from January 1 to February 31, 2022, we recruited 549 nurses from two hospitals in Hunan province in this cross-sectional study using a two-stage random sampling method. We used a self-designed questionnaire with good reliability and validity to measure clinical nurses’ knowledge, attitudes, and practice toward catheter-related thrombosis. We used χ2 test, Welch t-test, and multiple linear regression analysis to analyze the data.
Results: The knowledge of clinical nurses about catheter-related thrombosis was insufficient (55.00%), while the attitude was positive (88.49%) and the practice was inadequate (68.62%). Knowledge of clinical nurses was significantly associated with job title (β: 1.069, P< 0.001), educational level (β: 0.094, P< 0.05), and training times (β: 0.085, P< 0.05), which were positive factors while whether they are specialized nurses in intravenous therapy (β: − 0.126, P< 0.05), and hospital level (β: − 0.101, P< 0.05) were negative factors. Training times (β: 0.166, P< 0.001), job title (β: 0.099, P< 0.019), and hospital level (β: 0.090, P< 0.05) were associated factors of attitude. Moreover, training times (β: 0.255, P< 0.001) was the only factor associated with the practice.
Conclusion: Although clinical nurses hold a positive attitude towards catheter-related thrombosis, their knowledge level was unsatisfactory and their practice was affected by many factors, suggesting that nursing managers should strengthen the training and skill assessment of catheter-related thrombosis. At the same time, the hospital can formulate relevant rules, regulations, and guidelines to reduce the incidence of catheter-related thrombosis.
Keywords: knowledge, attitude, practice, clinical nurses, catheter-related thrombosis
Introduction
Catheter-related thrombosis (CRT) is venous thromboembolism (VTE) related to venous catheters,1 it refers to the venous blood clot formation in the vessel and vessel wall where the catheter is located because of a puncture or mechanical injury of the vessel intima or the patient’s disease.2 With the rapid development of intravenous infusion technology, central venous catheterization has become one of the indispensable technologies in modern medicine. Central venous catheter (CVC), peripherally inserted central venous catheter (PICC), and infusion port (PORT) have established effective venous treatment channels for patients in first aid, intensive care, and chemotherapy.3 It has solved many problems of medium and long-term infusion patients with peripheral venous puncture difficulties. Still, its accompanying catheter-related complications can not be ignored, especially CRT. CRT incidents will prolong the hospitalization time of patients, increase the hospitalization expenses of patients, and delay the treatment cycle of patients.4,5 Once the thrombus falls off, it will migrate to the pulmonary artery with blood flow, leading to pulmonary embolism and affection.2 Research shows that the risk factors of CRT involve multiple dimensions of patients, operators, and catheters. The average time of occurrence is 10 days, and the diagnostic time of most CRT is within 100 days, and the incidence of CRT reported in domestic and foreign literature is 16 ~ 66%,6 which is related to the different study design, study population, catheter type, and location, retention time, follow-up time, diagnostic methods, etc.6 Therefore, it is essential to strengthen the prevention and control of CRT and reduce the risk of CRT.
As the principal operator of central venous catheterization, clinical nurses are closely related to the occurrence of CRT. Clinical nurses play a vital role in the prevention and treatment of CRT and in reducing the risk of CRT. Specialized nurses of intravenous therapy carry out Central venous catheterization, and catheter maintenance is the participation of nurses in the ward. If any nurse fails to provide adequate care, CRT may occur. Research shows that nurses’ catheter maintenance knowledge and skills are closely related to the occurrence of CRT.7–9 However, although some experts formulated relevant practice guidelines and pointed out the importance of preventing complications of central venous catheterization at home and abroad,10 clinical nurses’ cognitive level of CRT is still uneven.11 At the same time, studies have found that central venous catheterization without professional nursing team maintenance is more likely to form venous thrombosis.12 If clinical medical staff ignore thrombosis or rapid extubation, it can easily cause venous thrombosis falling off and vascular embolism, and even life-threatening in severe cases. Therefore, the vital role of clinical nurses in preventing and treating CRT cannot be ignored.
Research has shown that the application of the knowledge, attitude, and practice (KAP) management model in improving the overall quality of nurses in dealing with venous thromboembolism is practical.13 Therefore, the key to reducing the incidence of CRT is to improve the mastery rate of clinical nurses’ knowledge of the prevention and treatment of CRT, correct the attitude of clinical nurses to prevent and treat CRT, and strengthen the practice of clinical nurses to prevent and treat CRT actively.
Currently, the research mainly focused on the investigation of nurses’ KAP of central venous catheterization, the investigation of knowledge and practice of catheter insertion and maintenance, and the improvement of PICC nursing experience and nursing quality, etc.14–17 In addition, there are also some researches primarily focused on investigating nurses’ KAP in preventing deep vein thrombosis, and venous thromboembolism which focused on the single catheter in individual departments, such as oncology nurses, geriatric nurses, etc.18–21 To sum up, clinical nurses still need to understand CRT knowledge, attitude, and behavior. How clinical nurses view CRT, and what factors will influence clinical nurses’ KAP of CRT are important and still unanswered questions. And this question is closely related to patient safety. Research shows that nurses’ and doctors’ patient safety attitude is closely related to patient safety,22,23 so knowing the KAP of clinical nurses about CRT and formulating corresponding measures are very important for reducing the occurrence of CRT and improving patient safety.
To bridge this knowledge gap, we conducted a cross-sectional study to evaluate the clinical nurses’ CRT knowledge, attitude, and practice and analyze its influencing factors which may strengthen the cognition and attention of clinical nurses about CRT, and provide a scientific basis for the formulation of CRT prevention and treatment training programs.
Materials and Methods
Study Design
This cross-sectional research was conducted in Hunan Province, China, from January 1 to February 31, 2022.
Participants
In the present study, the participants were registered nurses (RNs) working in hospitals in Hunan province, China. The inclusion criteria were: (a) RNs aged more than 18 but less than 60 years old, (b) RNs were given informed consent and participated voluntarily, and (c) RNs with more than one year of clinical working experience. Exclusion criteria: (a) RNs on medication for mental illness, (b) RNs absent from work due to sick leave, personal leave, study abroad, or other reasons, and (c) RNs in the medical technology department and other functional departments. Rejection criteria: (a) Incomplete answers to the questionnaire, (b) The answer options are consistent, and (c) The time for answering the questionnaire is too short.
Sample Size and Sampling Technique
The sample size of this study was calculated according to the Kendall estimation method: the sample size should be 5–10 times the number of questionnaire items (55 items in total). Thus the sample size was estimated to range between 275–550. We considered non-response and invalid response subjects and increased the sample size by 20%, corresponding to the range between 330 and 660.
We enrolled participants through a two-stage random sampling method. We adopted a two-stage random sampling method to select two hospitals in Hunan province. We selected 549 nurses from 2 hospitals randomly as the survey subjects. The specific sampling method was as follows: In the first stage, we set one Prefecture randomly from 13 prefecture-level cities and one Autonomous Prefecture in Hunan Province using the random number table method. In the second stage, we randomly selected one tertiary hospital and one secondary hospital from the prefecture-level city determined by the first stage sampling using the random number table method. We carried out this study in these two hospitals finally. We recruited RNs according to the study inclusion and exclusion criteria following the principle of informed consent and voluntary.
Ethical Considerations
The Medical Ethics Committee of Xiangya Hospital, Central South University, Changsha, China, approved this study (Ethics Review and Approval No: 202014123). Informed consent was obtained from all participants before data collection, and all participants’ clinical data and basic information were strictly confidential. All procedures complied with the Declaration of Helsinki.
Instrument
The questionnaire for this study was developed through literature review, focus group discussions, pre-tested and Delphi expert consultation, which consists of two sections. Section one is the General Information Collection Form. Section two is the questionnaire on knowledge, attitude, and practice of CRT. This section has three dimensions (55 items): Knowledge, attitude, and practice questionnaire. The knowledge questionnaire covers seven aspects, with a total of 25 items. All items are single-choice questions, with 1 point for correct answers and 0 points for wrong choices. The higher the score, the better the clinical nurses’ mastery of CRT knowledge. The attitude questionnaire includes 13 items in total using the Likert 5-level scoring method, five options of “strongly agree”, “agree”, “neutral”, “disagree”, and “strongly disagree” are set, which are calculated as (5, 4, 3, 2, 1) points respectively. The higher the score, the more positive the clinical nurse’s attitude in CRT. The practice questionnaire includes 17 items, all of which are frequency problems. Five options are set, including “always”, “often”, “sometimes”, “rarely”, and “never”, which are calculated as (5, 4, 3, 2, 1) points respectively. The higher the score, the more sufficient the clinical nurses are in preventing and treating CRT.
The questionnaire was confirmed to have good reliability and validity in the preliminary survey, with a Cronbach’s alpha coefficient of 0.939 and content validity of 0.813, which can be used in relevant research and practice.
Data Collection
The data were collected by four postgraduate students in our research group from January 1 to February 31, 2022. The specific steps used were as follows: initially, the investigators contacted the nursing managers in 2 selected hospitals and explained the purpose of the survey to obtain permission and support. At this stage, the investigators determined the total number of RNs in 2 hospitals. Subsequently, the investigators selected the eligible participants according to the study inclusion and exclusion criteria, following the principle of informed consent and voluntary with the help of the head nurses. A total of 587 RNs were selected and recruited. Finally, the investigators sent the questionnaires to 587 recruited RNs through a popular online questionnaire platform in China, Wen Juan Xing, and instructed them to fill them out.
Quality Control
Before the actual data collection period, we conducted pretesting of the questionnaire on 20 individuals and we made necessary modifications before applying it to the study participants and we excluded those who pretested from the actual study. To diminish the risk of selection bias, we determined explicit inclusion and exclusion criteria of the research objects and selected the participants strictly following these criteria. Besides, we ensured that the questionnaire was straightforward and did not involve sensitive questions to reduce the non-response rate. We set all questions must be answered before submitting the questionnaire when uploading the questionnaire to the background of Wen Juan Xing. To control information bias (also called observational bias), we provided unified training for the investigators on the study inclusion and exclusion criteria, the questionnaire content, and how to fill out the questionnaire. Also, we took measures to diminish the risk of reporting bias, including guaranteeing the anonymity of the participants and the confidentiality of data. We assured the participants that the questionnaire was answered anonymously, that their information would be kept confidential and only be used for research, and that their scores on the questionnaire would not influence their career and promotion as their employers could not see them.
Data Analysis
Data were analyzed using SPSS version 25.0 software. Descriptive statistics (frequency, percentage, mean, and standard deviation) were used to summarize the participant characteristics and the KAP score of CRT. The KAP scores among nurses with different characteristics were compared using the Wilcoxon rank-sum test for two-group comparisons and the Kruskal–Wallis H-test for multiple comparisons. We used Multiple linear regression analysis to analyze the influencing factors of nurses’ KAP towards CRT. The inclusion criteria of variables were 0.05, the exclusion criteria were 0.10, and p <0.05 was considered statistically significant. We used the Pearson correlation coefficient to analyze the relevance among the three dimensions of KAP, with p <0.05 considered statistically significant.
Results
Demographic Information of Participants
A total of 587 nurses were eligible to answer the questionnaire, and 549 nurses completed it, with a response rate of 93.53%. Among the 549 respondents, 239 nurses (43.5%) were from secondary hospitals, 310 nurses (56.5%) were from tertiary hospitals, and the majority were women. (97.1%). The largest age group was 40 and under (89.6%), followed by the range between 41 and 50 (9.5%). 52.3% of those who had been engaged in nursing work for less than 10 years, and 38.3% for 10–20 years. The majority exhibited an intermediate professional title (51.9%) and an education level of undergraduate (80.5%). Most of them were not specialized nurses in intravenous therapy (91.4%), and most had participated in the training for infusion catheter-related thrombosis. More nurses had participated 1–2 times (54.3%) and 2-4 times (30.6%), and fewer nurses had participated more than 4 times (15.1%). Further socio-demographic information is available in Table 1.
 |
Table 1 Demographics of the Participants (N=549) |
Knowledge, Attitude, and Practice Towards CRT Among Participants
The questionnaire survey showed that the total CRT knowledge, attitude and practice score of clinical nurses was (138.11 ± 18.11), and the average accounted for 78.92% of the total score. The scores of knowledge, attitude, and practice were (13.75 ± 3.15), (57.52 ± 8.42), (66.83 ± 12.52), respectively, and the average accounted for 55.00%, 88.49%, and 78.62% of the total score. Descriptive statistical analysis was carried out on the scores of secondary items in the three dimensions of knowledge, attitude, and practice. The two secondary items with the highest score rate of knowledge dimension were clinical manifestation (3.28 ± 0.92) and complication prevention and treatment (1.17 ± 0.68). The two secondary items with the highest score rate of attitude dimension were knowledge training (13.62 ± 2.02) and patient education (13.49 ± 2.02); The two secondary items with the highest scoring rate of practice dimension were health education practice (20.30 ± 4.11) and prevention and treatment practice (31.45 ± 5.98). (Table 2).
 |
Table 2 Score of Secondary Items in Each Dimension of CRT Knowledge, Attitude and Practice |
Factors Associated with Knowledge, Attitude, and Practice Towards CRT Among Participants
The results showed that there were significant differences in the scores of clinical nurses’ CRT knowledge at the hospital level, the educational level, the job title, and whether they are specialized nurses in intravenous therapy (p<0.05). There were significant differences in CRT attitude scores in the educational level, professional title, and training times about CRT (p <0.05). There were significant differences in CRT practice scores regarding job title, whether they are specialized nurses in intravenous therapy, and training times about CRT (p <0.05). (Table 3).
 |
Table 3 Analysis on the Current Situation of CRT Knowledge, Attitude and Practice of Nurses with Different Characteristics |
The results of multiple linear regression analysis showed that knowledge of clinical nurses was significantly associated with job title (β: 1.069, P<0.001), educational level (β: 0.094, P<0.05), and training times (β: 0.085, P<0.05), which were positive factors while whether they are specialized nurses in intravenous therapy (β: −0.126, P<0.05,) and hospital level (β: −0.101, P<0.05) were negative factors. Training times (β: 0.166, P<0.001), job title (β: 0.099, P<0.019), and hospital level (β: 0.090, P<0.05) were associated factors of attitude. Moreover, training times (β: 0.255, P<0.001) was the only factor associated with the practice. (Table 4). The Pearson correlation coefficient of clinical nurses’ CRT knowledge, attitude and practice showed that the correlation coefficient between attitude and knowledge was r = 0.092, p <0.05, showing a significant positive correlation. The correlation coefficient between attitude and practice was r=0.418, p <0.05, showing a significant positive correlation. (Table 5).
 |
Table 4 Multiple Linear Regression Analysis of Influencing Factors of CRT Knowledge, Attitude and Practice of Clinical Nurses with Different Characteristics |
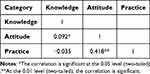 |
Table 5 Pearson Correlation Coefficient of CRT Knowledge, Attitude and Practice Scores |
Discussion
In this survey of 549 nurses in 2 hospitals across Hunan province, we examined clinical nurses’ KAP toward CRT and analyzed its influencing factors. To the best of our knowledge, this study is the first questionnaire about CRT knowledge, attitude, and practice of clinical nurses compiled at home and abroad. Only by knowing the KAP level of clinical nurses about CRT and the influencing factors, we can better formulate relevant policies and measures to improve the KAP level of nurses and apply them to clinical work, reduce the incidence of CRT and improve the quality of life of patients. From this study, We found that clinical nurses have a positive attitude towards CRT, but their knowledge and practice were insufficient, consistent with that previous study.24–27 The present study demonstrated that job title, training times, educational level, whether they are specialized nurses in intravenous therapy, and hospital level are associated factors to knowledge while the job title, training times, and hospital level are associated with the attitude. The training times is the only factor associated with the practice.
The results show that clinical nurses’ knowledge of CRT is insufficient, which is similar to the research results of Lu Lina and others.26,28,29 The reasons may be related to the rapid development of central venous catheter insertion technology. Still, the teaching resources of hospital nursing specialty need to be in line with clinical operations, inadequate training on central venous catheter insertion technology and the prevention and treatment of catheter-related complications, and the lack of corresponding practice guidelines in local hospitals.30 Further analysis of the secondary items of CRT cognition shows that clinical nurses’ knowledge of CRT mostly stays in concept and clinical manifestation, and their cognition of CRT diagnosis, risk factors, preventive measures, and treatment measures is not comprehensive, which is similar to the research results of Hyunjin.24 Studies have shown that early identification of CRT risk factors, prevention, and diagnosis can significantly reduce the incidence rate of CRT.31 At the same time, the study found that clinical nurses play a key role in the prevention and treatment of venous thromboembolism by increasing knowledge and health education for patients.32
The results show that clinical nurses’ attitude toward CRT is positive, consistent with the previous study.25 The analysis of the scoring rate of each secondary item of the CRT attitude dimension shows that clinical nurses are willing to strengthen CRT knowledge training, they believe that medical staff should participate in CRT knowledge training and hope that hospital managers can actively and regularly organize CRT knowledge training. On the other hand, clinical nurses expect to improve their catheterization, maintenance, and catheter evaluation ability. Most clinical nurses believe that catheterization and maintenance skills are closely related to the occurrence of CRT, and improving clinical nurses’ maintenance skills can reduce the occurrence of CRT. Gibbs found that nurses’ CRT risk assessment and prevention can significantly reduce CRT cases and subsequent complications.27 Most clinical nurses believe that strengthening the health education of patients and caregivers, including knowing the time of catheter maintenance and mastering the correct methods of limb function exercise, may be beneficial to the prevention and treatment of CRT and reduce the incidence of CRT, consistent with previous study.33
The results show that clinical nurses’ practice of CRT is inadequate, consistent with the previous study.34 By analyzing the scoring rate of each secondary item of the CRT practice dimension, we know that clinical nurses are unskilled by the corresponding theoretical support when carrying out CRT knowledge publicity and education to patients and their caregivers. Hospital managers have fewer training times for nurses on the advanced technology of central venous catheterization and the prevention of complications. There are fewer guidelines, rules, and regulations on all aspects of CRT knowledge, so clinical nurses have low scores in CRT learning practice, the research shows that strengthened, standardized training may help clinical nurses to improve their comprehension of the relevant guidelines and may finally reduce the occurrence of VTE in ICUs and improve the prognosis of critically ill patients with VTE.35 A review shows that whether inpatients adhere to CRT treatment depends mainly on the health education of nurses.36 Stephanie suggests that patients require further information on VTE during their hospitalization to enhance their involvement in VTE prevention and recognition. The provision of written, patient-directed statements could address that lack of participation. This study also highlights the need to strengthen the nurses’ role in providing patient education about VTE.37 It can be seen that the practice of nurses has a significant impact on CRT treatment, so it is essential to standardize further the practical practice of clinical nurses in CRT treatment.
The higher the hospital level is, the higher the knowledge score of clinical nurses about CRT and vice versa. Hospital level and whether they are specialized nurses in intravenous therapy negatively correlate with CRT knowledge. This result may be because the lower the hospital level is, the poorer the medical resources of hospitals are. The higher the level of the hospital, the more advanced the medical equipment and medical technology are. Nurses not specialized in intravenous therapy know less about CRT knowledge, which is negatively related. The prevention and education of advanced central venous catheterization and related knowledge are more in place. In contrast, the equipment and technology of secondary hospitals and below are relatively slow to update. It is suggested that give more material, financial, and policy support to secondary and lower-level hospitals from the government level.8 On the other hand, due to the large gap in medical resources and technical levels between different cities and regions, it is suggested that tertiary hospitals can play a leading role, and “Internet + care” be used to set up online and offline training mechanisms.38 We can communicate and exchange experiences with each other, improving clinical nurses’ cognitive rate of CRT and narrowing the gap in understanding CRT in regional medical institutions.
The higher the education level, the higher the clinical nurses’ knowledge and attitude score in CRT, which may be because nurses with higher education levels receive more relevant practical training and theoretical knowledge about CRT in schools, consistent with the previous study.28,29 The higher the professional title and more training times, the higher the score of nurses on CRT knowledge, attitude, and practice, which is similar to the previous study.8,39 Research shows that nurses with more training times have higher scores on cognition and nursing of thrombus around indwelling venous catheter than nurses with fewer training times.29 And The better you understand the importance of CRT prevention and treatment through CRT training, your corresponding CRT practice is more active. People with higher professional titles are generally the backbone of the Department’s technical business, and their clinical experience and theoretical knowledge are relatively prosperous. Research shows that nursing experience is closely related to nurses’ practice,40 clinical nurses with more clinical experience can better combine theoretical knowledge with practical operation. Nursing managers can encourage experienced, highly educated, professional nurses to teach CRT knowledge to inexperienced clinical nurses. We should focus on improving the CRT cognitive rate of junior nurses and strengthening their subjective initiative. We can carry out various training methods, such as online or offline lectures, knowledge competitions, group case discussions, skill operations, and theoretical knowledge assessments. Nurses’ hierarchical and stage training can improve the quality of catheter nursing and reduce the complications of central venous indwelling catheter puncture and indwelling complications to improve the clinical nurses’ knowledge level of CRT and reduce the incidence of CRT.41
A surprising result was that there was no significant difference in the KAP of clinical nurses of different ages and working years towards CRT, inconsistent with previous studies.29 The reason for our result may be our sample size is small and unrepresentative, and the age is proportional to the length of service. Some older nurses who work long hours lack the personal initiative to learn and are unwilling to absorb new knowledge, which leads to the decline of their motivation to learn CRT, and cannot profoundly realize the importance of preventing CRT. The results of the Pearson correlation coefficient show that there is a significant positive correlation between clinical nurses’ CRT attitudes and knowledge and between attitudes and practice, indicating that the more clinical nurses understand the relevant knowledge of CRT, the stronger their attitudes about CRT, and the stronger their attitudes about CRT, the more active their practice about CRT. This is consistent with Piechowski’s research which shows that attitude can affect knowledge and practical practice, and education can change nurses’ attitudes.42
Strength and Limitation
The present study has some strengths. To the best of our knowledge, it is the first study to provide data about clinical nurses’ knowledge, attitudes, and practice of CRT in Hunan province. Besides, the survey instrument developed in the present study could be used to evaluate nurses’ KAP of CRT in hospitals in other regions of China, it also could be used in other countries and territorial dimensions like those in China if it is translated and validated. However, some limitations of the present study are worth reviewing. First, although the quality control procedure was used throughout the data collection and entry, potential information bias may have occurred because the survey was based on self-reported data. Besides, although nurses’ attitude toward CRT was extremely positive, it might be affected by social desirability factors and cannot represent their actual attitude. Thus, a qualitative study on the nurse’s CRT attitude needs to be conducted in the future to verify the results of this study. Finally, this was a cross-sectional study in Hunan province, China. Even though the sample size was large enough (549) to ensure the statistical power to support the conclusions and the response rate of the survey was excellent (93.53%), the generalization of the results to nurses in hospitals in other areas of China is unclear, and similar studies should be conducted in other regions.
Conclusion and Future Recommendations
Central venous catheterization has become one of the indispensable technologies of modern medical technology. CRT is one of its serious complications, which may lead to pulmonary embolism and endanger patients’ lives. The knowledge awareness rate of clinical nurses about CRT is insufficient, and the attitude toward CRT is relatively positive. Still, the practice of CRT is inadequate. The knowledge, attitude, and practice (KAP) model show that any practice is determined by a person’s attitude and knowledge of these practices.43 Based on the present study’s findings, we suggest that hospital managers should improve clinical nurses’ cognition of CRT, strengthen nurses’ training and assessment of CRT knowledge, optimize the training process and content, improve nurses’ comprehension of CRT, and enhance nurses’ attention. Nursing managers should urge nurses to combine cognition with practice so that nurses’ nursing of CRT presents self-awareness, initiative, and predictability, understands the psychological characteristics of patients, carries out the evaluation and health education of venous indwelling periductal thrombus before, during, and after catheterization, and achieves targeted publicity and education in place in time, to provide high-quality nursing services in clinical practice and reduce the pain of patients.15 We can also set up a special central venous catheter quality control team to collect the data of patients with the clinical central venous catheter, monitor the incidence of CRT in the hospital, and provide evidence for clinical CRT control. At the same time, hospitals can further formulate detailed CRT processing processes and systems to standardize CRT processing flow and reduce the rate of CRT.
Acknowledgments
First, we thank Xiangya Hospital of Central South University for approving and supporting this study. Second, we would like to thank all directors of the nursing department in the 2 selected hospitals for their support and help during data collection and the participating nurses’ time. Third, we would also like to thank 20 experts in nursing management for their help in developing the survey instrument used in this study.
Funding
This study was funded by the National Natural Science Foundation of China (Grant No: 72174210). It was also supported by the 2021 Xiangya Nursing Discipline High-Level Scientific Research Project Cultivation Plan (Grant No: 2021xyhlpyjh004) and Clinical Research Fund of National Clinical Research Center for Geriatric Disorders, Xiangya Hospital, Central South University (Grant No: 2021LNJJ09).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Citla Sridhar D, Abou-ismail MY, Ahuja SP. Central venous catheter-related thrombosis in children and adults. Thromb Res. 2020;187:103–112. doi:10.1016/j.thromres.2020.01.017
2. Liu B, Xie J, Sun X, et al. Development and validation of a new clinical prediction model of catheter-related thrombosis based on vascular ultrasound diagnosis in cancer patients. Front Cardiovasc Med. 2020;7:571227. doi:10.3389/fcvm.2020.571227
3. Gorski LA. a look at 2021 infusion therapy standards of practice. Home Healthcare Now. 2021;39(2):62–71. doi:10.1097/NHH.0000000000000972
4. Bleeker SM, Van ESN, Van Gils L, et al. Clinical course of upper extremity deep vein thrombosis in patients with or without cancer: a systematic review. Thromb Res. 2016;140(Suppl 1):S81–S8. doi:10.1016/S0049-3848(16)30104-9
5. Hou J, Zhang J, Ma M, et al. Thrombotic risk factors in patients with superior vena cava syndrome undergoing chemotherapy via femoral inserted central catheter. Thromb Res. 2019;184:38–43. doi:10.1016/j.thromres.2019.10.030
6. Baumann Kreuziger L, Jaffray J, Carrier M. Epidemiology, diagnosis, prevention and treatment of catheter-related thrombosis in children and adults. Thromb Res. 2017;157:64–71. doi:10.1016/j.thromres.2017.07.002
7. Xu B, Zhang J, Hou J, Ma M. The current status of PICC maintenance knowledge and its influencing factors among nurses of primary hospitals in Hunan province. Chin Nurs Manag. 2018;18(10):1357–1361.
8. Xu B, Zhang J, Hou J, Ma M, Gong Z, Tang S. Nurses’ attitudes and knowledge of peripherally inserted central catheter maintenance in primary hospitals in china: a cross-sectional survey. Risk Manag Healthc Policy. 2020;13:903–913. doi:10.2147/RMHP.S250741
9. Xu B, Zhang J, Hou J, Ma M, Gong Z, Tang S. Nurses’ knowledge of peripherally inserted central catheter maintenance and its influencing factors in Hunan province, China: a cross-sectional survey. BMJ open. 2020;10(5):e033804. doi:10.1136/bmjopen-2019-033804
10. Murray J, Precious E, Alikhan R. Catheter-related thrombosis in cancer patients. Br J Haematol. 2013;162(6):748–757. doi:10.1111/bjh.12474
11. Debourdeau P, Farge D, Beckers M, et al. International clinical practice guidelines for the treatment and prophylaxis of thrombosis associated with central venous catheters in patients with cancer. J Thromb Haemost. 2013;11(1):71–80. doi:10.1111/jth.12071
12. Zheng L-Y, Peng Y, Yuan H, et al. Nurses’ knowledge of the management of drug-induced peripherally inserted central catheter obstruction: a descriptive phenomenological study. J Vasc Access. 2020;21(5):680–686. doi:10.1177/1129729819900864
13. Sadideen H, O’callaghan JM, Navidi M, et al. Educating surgical patients to reduce the risk of venous thromboembolism: an audit of an effective strategy. JRSM Short Rep. 2011;2(12):97. doi:10.1258/shorts.2011.011116
14. Almahmoud RS, Alfarhan MA, Alanazi WM, et al. Assessment knowledge and practices of central line insertion and maintenance in adult intensive care units at a tertiary care hospital in Saudi Arabia. J Infect Public Health. 2020;13(11):1694–1698. doi:10.1016/j.jiph.2020.07.009
15. Mlinar S, Malnarsić RR. Knowledge of nursing students about central venous catheters. Vojnosanit Pregl. 2012;69(4):333–339. doi:10.2298/VSP1204333M
16. Chopra V, Kuhn L, Ratz D, et al. Vascular nursing experience, practice knowledge, and beliefs: results from the Michigan PICC1 survey. J Hosp Med. 2016;11(4):269–275. doi:10.1002/jhm.2523
17. Serpici A, Gürsoy A. Nurse-led patient training improves deep vein thrombosis knowledge and self-care practices. J Vasc Nurs. 2018;36(2):53–63. doi:10.1016/j.jvn.2018.03.002
18. Sun Q, Xu H, Li H, et al. A survey of nurses’ knowledge of PICC related thrombosis prevention and treatment in oncology departments. Chin J Nurs Educ. 2019;16(08):617–620.
19. Zhu J, Lin M, Zhou C. Investigation on the status of cognition, attitude and behavior of nurses on deep vein thrombosis in 6 first class tertiary hospitals in Guangzhou. Contemp Med. 2016;22(29):6–8.
20. Chen X, Gao Y, Zhang W, et al. Influence of nurses’ knowledge, attitude and behavior on the prevention of deep vein thrombosis. J Qilu Nurs. 2019;25(06):67–71.
21. Zhao W, Huang Y, Zhang X. Investigation on the status of knowledge, belief, and practice of venous thromboembolism prevention among geriatric nurses. Chin J Mod Nurs. 2018;24(29):3494–3498.
22. Al-Mugheed K, Bayraktar N. Patient safety attitudes among critical care nurses: a case study in North Cyprus. Int J Health Plann Manage. 2020;35(4):910–921. doi:10.1002/hpm.2976
23. AL-Mugheed K, Bayraktar N, Al-Bsheish M, et al. Patient safety attitudes among doctors and nurses: associations with workload, adverse events, experience. Healthcare. 2022;10:631. doi:10.3390/healthcare10040631
24. Oh H, Boo S, Lee J-A, et al. Clinical nurses’ knowledge and practice of venous thromboembolism risk assessment and prevention in South Korea: a cross-sectional survey. J Clin Nurs. 2017;26(3–4):427–435. doi:10.1111/jocn.13424
25. Feng S, Li M, Wang K, et al. Knowledge, attitudes, and practices regarding venous thromboembolism prophylaxis: a survey of medical staff at a tertiary hospital in China. Medicine. 2021;100(49):e28016. doi:10.1097/MD.0000000000028016
26. Wang Y, Wu X-J, Ma Y-F, et al. Chinese orthopaedic nurses’ knowledge, attitude and venous thromboembolic prophylactic practices: a multicentric cross-sectional survey. J Clin Nurs. 2021;30(5–6):773–782. doi:10.1111/jocn.15615
27. Ting Y, He W, Hang C, et al. Nurses’ knowledge, attitudes, and behaviors toward venous thromboembolism prophylaxis: how to do better. Vascular. 2021;29(1):78–84. doi:10.1177/1708538120933782
28. Al-Mugheed KA, Bayraktar N. Knowledge and practices of nurses on deep vein thrombosis risks and prophylaxis: a descriptive cross sectional study. J Vasc Nurs. 2018;36(2):71–80. doi:10.1016/j.jvn.2018.02.001
29. Lina L, Huiping Y, Weizhen Z, et al. Survey on cognition condition and present nursing status on catheter-associated thrombosis nurses in Zhoushan District. Nurs Rehabilit J. 2016;15(9):834–837.
30. Geerts W. Central venous catheter-related thrombosis. Hematol Ame Soc Hematol Educ Progr. 2014;2014(1):306–311. doi:10.1182/asheducation-2014.1.306
31. Khan F, Tritschler T, Kahn SR, et al. Venous thromboembolism. Lancet. 2021;398(10294):64–77. doi:10.1016/S0140-6736(20)32658-1
32. Titze M, Gurley J. VTE prevention: development of an institutional protocol and the nurse’s role. Medsurg Nurs. 2014;23(5):331–342.
33. Kim PS, Probeck K, Elitharp D, et al. The staff and patient perspectives on compliance with mechanical prophylaxis for venous thromboembolism. J Vasc Surg. 2018;6(4):441–448. doi:10.1016/j.jvsv.2018.01.008
34. Yohannes S, Abebe T, Endalkachew K, et al. Nurses’ knowledge, perceived practice, and their associated factors regarding Deep Venous Thrombosis (DVT) prevention in Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, 2021: a cross-sectional study. Crit Care Res Pract. 2022;2022(7386597):16. doi:10.1155/2022/7386597
35. Tang X, Sun B, Yang Y, et al. A survey of the knowledge of venous thromboembolism prophylaxis among the medical staff of intensive care units in North China. PLoS One. 2015;10(9):e0139162. doi:10.1371/journal.pone.0139162
36. Laval KA, Costello JF. Assessment of the public’s knowledge of venous thromboembolism. J Vasc Nurs. 2015;33(2):68–71. doi:10.1016/j.jvn.2014.11.001
37. LE SAGE S, Mcgee M, Emed JD. Knowledge of venous thromboembolism (VTE) prevention among hospitalized patients. J Vasc Nurs. 2008;26(4):109–117. doi:10.1016/j.jvn.2008.09.005
38. Grau-Muñoz A. Estrategias ante el uso de Internet por población usuaria en Atención Primaria: una clasificación sociológica [A proposal of sociological classification of Internet use in primary health care]. Gac Sanit. 2021;35(5):420–424. doi:10.1016/j.gaceta.2020.08.008
39. Zhou W-H, He J-Q, Guo S-G, et al. Venous thromboembolism in the emergency department: a survey of current best practice awareness in physicians and nurses in China. World J Emerg Med. 2019;10(1):5. doi:10.5847/wjem.j.1920-8642.2019.01.001
40. Elder S, Hobson DB, Rand CS, et al. Hidden barriers to delivery of pharmacological venous thromboembolism prophylaxis: the role of nursing attitudes and practices. J Patient Saf. 2016;12(2):63–68. doi:10.1097/PTS.0000000000000086
41. Wen Q. Potential safety risks associated with clinical use of PICC and management status. J Nurs Sci. 2013;28(14):6–8.
42. Piechowski KL, Elder S, Efird LE, et al. Prescriber knowledge and attitudes regarding non-administration of prescribed pharmacologic venous thromboembolism prophylaxis. J Thromb Thrombolysis. 2016;42(4):463–470. doi:10.1007/s11239-016-1378-8
43. Alzghoul BI, Abdullah NAC. Pain management practices by nurses: an application of the Knowledge, Attitude and Practices (KAP) Model. Glob J Health Sci. 2015;8(6):154–160. doi:10.5539/gjhs.v8n6p154
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
