Back to Journals » Journal of Asthma and Allergy » Volume 15
Clinical Features and Outcomes Associated with Bronchial Asthma Among COVID-19 Hospitalized Patients
Authors Diaz MA, Catalan-Caceres N , Beauperthuy TC , Domingo C, Ibañez E, Morata C, De Diego A
Received 26 December 2021
Accepted for publication 29 April 2022
Published 8 June 2022 Volume 2022:15 Pages 775—781
DOI https://doi.org/10.2147/JAA.S354082
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Amrita Dosanjh
Miguel Angel Diaz,1 Nelly Catalan-Caceres,1 Thais C Beauperthuy,2 Carlos Domingo,1 Ethel Ibañez,1 Carmen Morata,3 Alfredo De Diego2
1Allergy Department, Hospital Universitari I Politècnic La Fe, Valencia, Spain; 2Respiratory Department, Hospital Universitari I Politècnic La Fe, Valencia, Spain; 3Internal Medicine Department, Hospital Universitari I Politècnic La Fe, Valencia, Spain
Correspondence: Miguel Angel Diaz, Allergy Department, Hospital Universitari I Politècnic La Fe, Avinguda de Fernando Abril Martorell, 106, Valencia, 46026, Spain, Tel +34 961244084, Email [email protected]
Background: The impact of diagnosis treatment and bronchial asthma on coronavirus disease 2019 (COVID-19) associated outcomes remains unclear.
Objective: To identify the prevalence and outcomes associated with asthma among hospitalized patients with COVID-19.
Methods: Electronic health records of 130 patients with asthma among hospitalized patients with COVID-19 were reviewed. Two subgroups of asthmatic patients were compared according to clinical outcomes during hospitalization. Patients with death results, intubation, and/or need of intensive care unit (ICU) stay were grouped as asthmatic patients with severe COVID-19 outcomes, and the rest were grouped as asthmatic patients with non-severe COVID-19 outcomes. Multivariable analyses were conducted with logistic regression to identify independent risk factors for severe outcomes.
Results: The prevalence of asthma in COVID-19 hospitalized patients was 5%. The mean age was 59.4 years and 54% were women. 17% received treatment in GINA step 4– 5 asthma at the time of admission. An allergic asthma phenotype was determined in 38%. There was no significant difference in hospital length of stay or need for intubation between asthmatic patients and global COVID-19 admitted patients. 17% of asthmatic patients developed a severe outcome, and 5% had a death result. Elevated Lactate Dehydrogenase (LDH) level, low transcutaneous pulse oximetry (SpO2), the coexistence of atrial fibrillation (AF), and need for moderate or high ICS at admission were independent risk factors for a worse outcome in asthmatics COVID-19 hospitalized patients.
Conclusion: The prevalence of asthma in COVID-19 hospitalized patients was 5%, consistent with the asthma prevalence in the general population. The asthmatic patients with the previous prescription of moderate or high doses of ICS and/or coexistence of atrial fibrillation at admission had a higher risk of the severe outcome.
Keywords: bronchial asthma, COVID-19, risk factors, outcomes
Introduction
There is no clear evidence so far that patients with asthma are more likely to be infected with COVID-19 or to become severely ill. Most of the prevalence studies agree in pointing out an underrepresentation of asthma as a risk factor for admission and/or morbi-mortality due to COVID-19,1–4 and this risk would be even lower in patients with asthma with allergic phenotype when compared to patients with non-allergic phenotype.5 Nevertheless, some studies contradict this general trend, reporting in asthmatic patients a higher risk of hospitalization6 or intubation,7 particularly in severe asthma or non-allergic asthma cases.8
Different hypotheses have been proposed to explain the low representation of asthma in COVID-19 complicated outcomes: better compliance of the social isolation measures in asthmatic patient population compared to other groups, a protective effect of T2 response in asthmatic patients9, or a protective effect of inhaled and/or systemic corticosteroids.10,11
Our study aimed to analyze the clinical features of asthmatic patients and SARS-CoV-2 pneumonia who required admission to a tertiary referral hospital in Valencia, Spain, and to identify the risk predictor factors of worse outcomes at admission.
Materials and Methods
Electronic medical records of patients admitted to COVID-19 Units of our hospital were reviewed (1st March 2020–28th February 2021). Asthmatic patients were determined based on ICD-10 coding in the discharge report. Asthma cases were only included when the diagnosis was confirmed in electronic clinical history and the patient required ongoing asthma medication at admission. Two groups of patients were compared according to clinical outcomes during hospitalization. Patients with death results, and/or need for intubation, and/or need of intensive care unit (ICU) stay were grouped as asthmatic patients with severe COVID-19 outcomes, and patients discharged without requiring invasive procedures were grouped as asthmatic patients with non-severe COVID-19 outcomes. The previous history of sensitization to aeroallergens detected by prick test and/or specific IgE were considered as an allergic asthma phenotype. Atopic dermatitis and/or food allergy were considered atopic comorbidity. Asthmatic exacerbation was considered if the patient had required at least a short course of oral or parental corticosteroids during the previous year to admission. Spirometry values were collected if an examination was available in electronic medical records within 2 years prior to admission.
Statistical Analysis
Continuous variables are presented as mean ± SD and compared using the Student’s t-test. Discrete variables are presented as percentages (proportions), and compared with the Chi-square test, using Fisher correction when needed. Statistical analysis was done using the SPSS statistical package (Chicago, Illinois). Associations were considered statistically significant when p < 0.05, although all p values are presented. Multivariable analyses were conducted with logistic regression to identify independent risk factors for severe outcomes. Variables with p<0.1 in the univariate analysis were included in multivariable analysis.
Results
130 patients with asthma were identified, representing 5.03% of the global population admitted for COVID-19 (n=2585) during the period of the study. Table 1 shows comparative data of asthmatics admitted patients and global admitted patients with COVID-19 in our hospital. There was no significant difference in mean age, hospital length of stay, or need for intubation between asthmatic patients and global COVID −19 admitted patients. Of note, patients with asthma and COVID-19 had a mortality rate of 5% vs 14% in the global admitted COVID-19 patients (p<0.001). Table 2 summarizes the demographic and clinical characteristics of the study population. The mean age of asthma patients was 59.4±17.5 years. Women were 54%. An allergic asthma phenotype was determined in 38% of the patients. At admission, 17% of asthmatic patients received treatment in GINA step 4 or 5, 46% in GINA step 2 or 3, and 37% were not treated with regular ICS (GINA step 1). Previous FEV1% and FEV1/FVC were 90.3±24 (1/m) and 75±14 respectively (n= 52). Table 3 shows laboratory findings on admission, COVID19- therapy, and length of hospital stay.
 |
Table 1 Comparative Data of Asthmatic Admitted Patients and Global Admitted Patients with COVID-19 |
 |
Table 2 Demographics and Clinical Features of Asthmatic COVID-19 Admitted Patients |
 |
Table 3 Laboratory Findings on Admission, COVID-19 Therapy, and Length of the Hospital Stay |
Out of the asthmatic patients, 17% presented a severe outcome. Considering all data examined, significant differences for a poor prognosis were detected in comorbidities (bronchiectasis, AF), prescribed treatments (GINA step 4 or 5, moderate or high ICS doses), and laboratory findings (LDH, CRP, SpO2).
In the multivariable regression analysis, 4 predictive independent factors were identified: AF comorbidity, need for moderate or high ICS doses, lower SpO2, and higher LDH (Table 4). In laboratory findings, the best cut-off values for predicting severe outcome were LDH >300 U/L (p<0.001), CRP >90 mgrs./L(p=0.003) and SpO2≤94% (p=0.013).
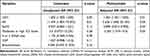 |
Table 4 Clinical Factors Independently Associated with Severe Outcomes Among Asthmatic Patients Hospitalized with COVID-19 |
Discussion
Previous research reveals significant differences in the prevalence of asthma among patients with COVID-19 according to geographical origin. Multiple factors possibly determine this variability: social and political customs, health system organization, genetic factors, or assessment period (an earlier or more advanced phase of the pandemic), among others.
The overall prevalence of asthmatic COVID-19 admitted patients in our study (5.03%) is similar to previous ones conducted in our geographical zone.12,13 These data are in line with 6.4% of asthmatic patients admitted for COVID-19 in European studies, with an intermediate prevalence between 2.2% in Asia and 10.2% in North America.14
Allergic asthma phenotype was determined in 38% of admitted patients, consistent with the prevalence rates of 26–39% reported among asthmatics adults over 50 years.15,16
The mean spirometric values prior to admission were within normal limits, without significant differences between severe and non-severe outcomes, although the sample analyzed was small.
According to multivariate regression analysis, concomitant AF, elevated LDH level, lower SpO2 saturation, and previous treatment with moderate or high dose inhaled corticosteroids at admission were independent risk factors for severe outcomes, in line with reported published research.17–20,27 Other major risk factors for a poor prognosis of COVID-19 (age, obesity, hypertension, diabetes, cancer, etc.) were not detected in our study.
Regarding eosinophils, the mean absolute eosinophil count (AEC) in our COVID-19 asthmatic patients was low (50.4 ± 110.3). Eosinopenia is a common finding in COVID-19 disease1 probably related to worse outcomes in asthmatic patients,21,22 nonetheless, in our cohort of patients with asthma we did not find significant differences in absolute eosinophil count on admission in terms of outcomes, as in previous reports.27
The strengths of our work lie in the enrolled patients being representative of the real-life asthmatic patients hospitalized with COVID-19 as well as in the large set of clinical and biochemical data collected. Nonetheless, it presents some limitations. Data were collected from a single hospital with a retrospective design. Comparative group control and outpatients with asthma were not included in the analysis. Previous spirometry and some laboratory data (IL-6, ferritin) were only disposable in a limited number of patients. Finally, a larger cohort study is needed to verify our conclusions.
Conclusion
Our results suggest that admitted adult patients with asthma did not have a higher risk of severe COVID-19. 5% of asthmatic patients had a result of death vs 14.8% of the global admitted population (p<0.001). The prevalence of asthma in COVID-19 hospitalized patients was consistent with asthma prevalence in the general population. Asthmatic patients with more requirements in their treatments (moderate or high doses of ICS) and coexistence of AF, had a higher risk of the severe outcome. SpO2 ≤ 94% and LDH>300 on admission were other independent factors for a poor prognosis in asthmatics patients hospitalized with COVID-19.
Acknowledgments
We acknowledge Dra. Silvia Marset and Dr. José Castejón from Admissions and Clinical Documentation Department of La Fe University and Polytechnic Hospital, by providing data to this analysis. We are also thankful to all front-line healthcare workers of our hospital and clinical staff of Allergy Service, who made this research possible.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Zhang J, Dong X, Cao Y, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. 2020;75(7):1730–1741. doi:10.1111/all.14238
2. Li X, Xu S, Yu M, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110–118. doi:10.1016/j.jaci.2020.04.006
3. Wang Y, Ao G, Qi X, Xie B. The association between COVID‐19 and asthma: a systematic review and meta‐analysis. Clin Exp Allergy. 2020;50(11):1274–1277. doi:10.1111/cea.13733
4. Mendes NF, Jara CP, Mansour E, Araújo EP, Velloso LA. Asthma and COVID-19: a systematic review. Allergy, Asthma Clin Immunol. 2021;17(1). doi:10.1186/s13223-020-00509-y
5. Eggert LE, He Z, Collins W, et al. Asthma phenotypes, associated comorbidities, and long‐term symptoms in COVID‐19. Allergy. 2021;19(1):173–185.
6. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052. doi:10.1001/jama.2020.6775
7. Rosenthal JA, Awan SF, Fintzi J, Keswani A, Ein D. Asthma is associated with increased risk of intubation but not hospitalization or death in coronavirus disease 2019. Ann Allergy, Asthma Immunol. 2021;126(1):93–95. doi:10.1016/j.anai.2020.10.002
8. Zhu Z, Hasegawa K, Ma B, Fujiogi M, Camargo CA, Liang L. Association of asthma and its genetic predisposition with the risk of severe COVID-19. J Allergy Clin Immunol. 2020;146(2):327–329.e4. doi:10.1016/j.jaci.2020.06.001
9. Kimura H, Francisco D, Conway M, et al. Type 2 inflammation modulates ACE2 and TMPRSS2 in airway epithelial cells. J Allergy Clin Immunol. 2020;146(1):80–88.e8. doi:10.1016/j.jaci.2020.05.004
10. Peters MC, Sajuthi S, Deford P, et al. COVID-19 related genes in sputum cells in asthma: relationship to demographic features and corticosteroids. Am J Respir Crit Care Med. 2020;202(1):83–90. doi:10.1164/rccm.202003-0821OC
11. Jackson DJ, Busse WW, Bacharier LB, et al. Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2. J Allergy Clin Immunol. 2020;146(1):203–206.e3. doi:10.1016/j.jaci.2020.04.009
12. Prieto-Alhambra D, Balló E, Coma E, et al. Hospitalization and 30-day fatality in 121,263 COVID-19 outpatient cases. MedRxiv. 2020;20090050. doi:10.1101/2020.05.04.20090050
13. Borobia A, Carcas A, Arnalich F, et al. A cohort of patients with COVID-19 in a major teaching hospital in Europe. J Clin Med. 2020;9(6):1733. doi:10.3390/jcm9061733
14. Liu S, Cao Y, Du T, Zhi Y. Prevalence of comorbid asthma and related outcomes in COVID-19: a systematic review and meta-analysis. J Allergy Clin Immunol Pract. 2021;9(2):693–701. doi:10.1016/j.jaip.2020.11.054
15. Pallasaho P, Ronmark E, Haahtela T, Sovijarvi ARA, Lundback B. Degree and clinical relevance of sensitization to common allergens among adults: a population study in Helsinki, Finland. Clin Exp Allergy. 2006;36(4):503–509. doi:10.1111/j.1365-2222.2006.02460.x
16. Warm K, Backman H, Lindberg A, Lundbäck B, Rönmark E. Low incidence and high remission of allergic sensitization among adults. J Allergy Clin Immunol. 2012;129(1):136–142. doi:10.1016/j.jaci.2011.08.033
17. Li C, Ye J, Chen Q, et al. Elevated Lactate Dehydrogenase (LDH) level as an independent risk factor for the severity and mortality of COVID-19. Aging. 2020;12(15):15670–15681. doi:10.18632/aging.103770
18. Peltzer B, Manocha KK, Ying X, et al. Outcomes and mortality associated with atrial arrhythmias among patients hospitalized with COVID‐19. J Cardiovasc Electrophysiol. 2020;31(12):3077–3085. doi:10.1111/jce.14770
19. Budweiser S, Ş B, Jörres RA, et al. Patients’ treatment limitations as predictive factor for mortality in COVID-19: results from hospitalized patients of a hotspot region for SARS-CoV-2 infections. Respir Res. 2021;22(1). doi:10.1186/s12931-021-01756-2
20. Caminati M, Vultaggio A, Matucci A, et al. Asthma in a large COVID-19 cohort: prevalence, features, and determinants of COVID-19 disease severity. Respir Med. 2021;176:106261. doi:10.1016/j.rmed.2020.106261
21. Ferastraoaru D, Hudes G, Jerschow E, et al.Eosinophilia in asthma patients is protective against severe COVID-19 illness. J Allergy Clin Immunol Pract. 2021;(3):1152–1162.e3. doi:10.1016/j.jaip.2020.12.045
22. Valverde-Monge M, Cañas JA, Barroso B, et al. Eosinophils and chronic respiratory diseases in hospitalized COVID-19 patients. Front Immunol. 2021;12:668074. doi:10.3389/fimmu.2021.668074
23. Halpin DMG, Singh D, Hadfield RM. Inhaled corticosteroids and COVID-19: a systematic review and clinical perspective. Eur Respir J. 2020;55(5):2001009. doi:10.1183/13993003.01009-2020
24. Yamaya M, Nishimura H, Deng X, et al. Inhibitory effects of glycopyrronium, formoterol, and budesonide on coronavirus HCoV-229E replication and cytokine production by primary cultures of human nasal and tracheal epithelial cells. Respir Investig. 2020;58(3):155–168. doi:10.1016/j.resinv.2019.12.005
25. Matsuyama S, Kawase M, Nao N, et al. The inhaled steroid ciclesonide blocks SARS-CoV-2 RNA replication by targeting the viral replication-transcription complex in cultured cells. J Virol. 2020;95(1). doi:10.1128/JVI.01648-20
26. Jeon S, Ko M, Lee J, et al. Identification of antiviral drug candidates against SARS-CoV-2 from FDA-approved drugs. Antimicrob Agents Chemother. 2020;64(7):e00819–20. doi:10.1128/AAC.00819-20
27. Chen D, Zhang S, Feng Y, et al. Decreased eosinophil counts and elevated lactate dehydrogenase predict severe COVID-19 in patients with underlying chronic airway diseases. Postgrad Med J;2021.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
