Back to Journals » Clinical Ophthalmology » Volume 10
Clinical characteristics and selection of treatment modality for patients with vitreomacular traction: real-world implementation of NICE guidance (TA297)
Authors Pritchard E, Shams-Ulislam I, Amar S, Yang Y, Narendran N
Received 10 June 2015
Accepted for publication 3 September 2015
Published 12 January 2016 Volume 2016:10 Pages 79—85
DOI https://doi.org/10.2147/OPTH.S90257
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Edward William James Pritchard,1 Shams-Ulislam Ilyas,1 Soha Khaled Amar,2 Yit Chuin Yang,3 Nirodhini Narendran1
1Ophthalmology Department, Wolverhampton Eye Infirmary, New Cross Hospital, Royal Wolverhampton Hospitals NHS Trust, Wolverhampton, 2College of Medical and Dental Sciences, University of Birmingham, 3Optometry Department, Faculty of Life and Health Sciences, Aston University, Birmingham, UK
Aim: To investigate the qualitative aspects in patient selection and the quantitative impact of disease burden in real world treatment of vitreomacular traction (VMT) and implementation of the National Institute for Health and Care Excellence (NICE) guidance (TA297).
Methods: A monocentric, retrospective review of consecutive patients undergoing optical coherence tomography (OCT) imaging over a 3 month period. Patients with VMT in at least one eye were identified for further data collection on laterality, visual acuity, symptoms, presence of epiretinal membrane, macular hole and treatment selection.
Results: A total of 3472 patients underwent OCT imaging with a total of 6878 eyes scanned. Out of 87 patients, 74 patients had unilateral VMT (38 right, 36 left) and 13 patients had bilateral VMT. Eighteen patients with unilateral VMT satisfied NICE criteria of severe sight problems in the affected eye. Eight were managed for a coexisting pathology, one refused treatment, one patient did not attend, two closed spontaneously, and one received ocriplasmin prior to the study start date. Only two patients with unilateral VMT received ocriplasmin and three underwent vitrectomy. Those failing to meet NICE criteria for unilateral VMT were predominantly asymptomatic (n=49) or had coexisting ERM (n=5) or both (n=2).
Conclusion: Ocriplasmin provides an alternative treatment for patients with symptomatic VMT. Our data shows that the majority of patients with VMT do not meet NICE TA297 primarily due to lack of symptoms. Those meeting NICE criteria, but not treated, tended to have coexisting macular pathology. Variation in patient selection due to subjective factors not outlined in NICE guidance suggests that real world outcomes of ocriplasmin therapy should be interpreted with caution.
Keywords: vitreomacular traction, posterior vitreous detachment, pharmacologic vitreolysis, ocriplasmin
Introduction
Vitreomacular traction (VMT), first described by Reese et al 1970,1 is a disorder widely accepted to be the result of traction at the vitreoretinal interface. This is due to vitreomacular adhesion (VMA) causing incomplete or anomalous detachment of the posterior hyaloid face from the internal limiting membrane during the physiological process of posterior vitreous detachment (PVD).1–6 VMA and VMT can lead to reduced visual acuity from distortion, displacement, or disruption of the normal foveal and retinal anatomy, resulting in clinically recognized lesions, such as macular pucker, focal cysts, foveal eversion, and macular hole (MH) formation.7–12 Until recently, observation or pars plana vitrectomy (PPV) were the only treatment modalities available. More recently, landmark clinical trials have reported that ocriplasmin, a recombinant truncated form of human plasmin, which acts by cleaving fibronectin and laminin, to be effective in resolution of VMT.13–16 Furthermore, recent analysis of the trial data shows improved patient-reported visual outcome following ocriplasmin compared to placebo.17 Real-world data has shown that VMT resolution following ocriplasmin varies between 42% and 50% and MH closure in 27%–50% of cases.18–22 Quezada-Ruiz et al have also recently reported favorable visual outcome in eleven of 23 patients treated for VMT with and without MHs, and observed that VMT release occurred more frequently in those with outer reflectivity changes that resolved following VMT release.23
The National Institute for Health and Care Excellence (NICE) has published guidance (TA297) on patient-selection criteria for ocriplasmin therapy. NICE guidance indicates that patients with VMT – in the absence of epiretinal membrane (ERM) – with a stage II full-thickness MH (FTMH) less than 400 μm and/or severe symptoms should be offered ocriplasmin treatment. In the costing tool provided with TA297, the number of patients requiring ocriplasmin therapy per year in England was estimated at 745 (with MH) and 209 (without MH) for a population of 55 million, and 120 patients who would still require vitrectomy due to persistent VMT following ocriplasmin.24 This would equate to approximately 17 patients requiring ocriplasmin therapy and two requiring additional vitrectomy for persistent VMT per year in a population of one million.
The clinical characteristics that influence the clinical decision-making process in selecting patients for watchful waiting, ocriplasmin therapy, or vitrectomy in the real world have not been previously studied. Variable estimates of the frequency and prevalence of VMT have been published, but the resultant actual frequency of ocriplasmin use in the real world and the reasons for noncompliance are not known either.25–27 Such quantitative and qualitative data could be valuable to clinicians in designing their local pathways for patient selection and for planning future resources to implement NICE guidance. In this study, we used a case-by-case tracking design to investigate the qualitative aspects in patient selection and the quantitative impact of disease burden in a real-world VMT treatment-service scenario.
Materials and methods
The setting for the study was our hospital’s retinal imaging department, which provides on-demand multimodal imaging for patients referred from primary care services from a catchment population of around 850,000 to our general ophthalmology services, in addition to patients referred into our secondary and tertiary macular referral service.
In order to investigate patient-selection criteria for ocriplasmin therapy, a period of 3 consecutive months (May, June, and July 2014) was chosen to allow 6 complete months after publication of the NICE TA297 guidance. The complete electronic imaging database was used to identify consecutive patients undergoing optical coherence tomography (OCT) imaging on at least one occasion over this period. Individual imaging episodes were easily located on a common server, which contained all images archived from four networked OCT machines (Spectralis; Heidelberg Engineering GmbH, Heidelberg, Germany). In cases where patients attended more than once during the study period, the earliest imaging episode was selected. The individual scans were viewed using the proprietary software (Eye Explorer, Heidelberg Engineering).
Three observers (EWJP, SKA, and ISU) screened all scans to exclude all episodes where the posterior hyaloid line was not visible. All scan episodes where the posterior hyaloid line was distinctly visible as a line anterior to the retina and adhering to the macula were subsequently viewed by a senior retinal specialist (YCY and NN) to confirm the diagnoses of VMT or VMA with or without ERM and with or without an MH. For the patients confirmed to have VMT by the senior retinal specialist, case notes were then reviewed retrospectively. Data collected from case notes included visual acuity, symptoms, primary diagnosis, and subsequent management documented at the time of the hospital visit. Patients found to meet the NICE guidance were individually tracked for up to 6 months to determine the treatment they received and rationale for this treatment option. A flowchart was created to illustrate quantitatively the disposition in terms of management approach depending on eligibility according to NICE criteria and qualitatively the disposition in terms of factors attributed to patient eligibility or ineligibility (Figure 1). In line with Royal Wolverhampton Hospitals policy, ethics committee approval for retrospective data collection studies was not required. Patient consent is not necessary for clinical evaluation of local practice against current recommended guidelines.
Results
During the 3-month study period, a total of 3,472 patients had OCT scans, with a total of 6,878 eyes scanned. Of 87 patients (54 females, 33 males) with an average age of 76.2 years (range 51–96 years), 74 patients had unilateral VMT (38 right, 36 left) and 13 patients had bilateral VMT. Representative spectral domain OCT images for VMT are shown in Figure 1. The quantitative and qualitative dispositions of these patients are shown in Figure 2.
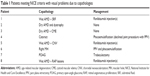
Of 74 patients with unilateral VMT, 18 patients met NICE criteria for ocriplasmin and 56 did not. Of the 18 patients that met NICE criteria for ocriplasmin, only two patients actually received ocriplasmin. Three patients had PPV, and 13 patients had no intervention. The reasons given for not using ocriplasmin included 1) opted for PPV (n=3), 2) patient refused treatment (n=1), 3) watchful waiting recommended due to improving OCT appearances (n=2), 4) prior ocriplasmin without success (n=1), 5) lost to follow-up (n=1), and 6) presence of coexisting pathology (n=8). Of these eight patients, three had wet age-related macular degeneration (AMD) and were being treated with ranibizumab, two were diagnosed with dry AMD with no follow-up, one had severe primary open-angle glaucoma that required trabeculectomy, one opted for cataract surgery only without any VMT treatment, and another was awaiting phacoemulsification and MH repair (Table 1). The 56 patients failing to meet NICE criteria with unilateral VMT were predominantly asymptomatic (n=49) or had coexisting ERM (n=5) or both (n=2).
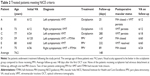
There were 13 patients with bilateral VMT, which are also illustrated in Figure 1. Dispositions are shown in terms of study eyes and the fellow eyes, where the study eye represents the eye with the more significant disease. Among the study eyes, six eyes met NICE criteria and only one received ocriplasmin. For the remaining five eyes, one patient refused treatment, two had dry AMD and were not followed up, one was watched and felt to be stable, and lastly one patient had FTMH that was closing spontaneously. Among seven study eyes that did not meet NICE criteria, four were asymptomatic, one had symptomatic ERM, one had ERM without symptoms, and one had a symptomatic large FTMH with ERM.
Three of 13 fellow eyes met NICE criteria, and none of these received treatment. Two eyes had dry AMD, and one eye was watched and found to be stable. Ten fellow eyes did not meet NICE criteria, and all of these were asymptomatic. Table 2 shows the distribution of treatment modality used for patients meeting NICE criteria. The average age of these patients was 75.6 years. Six patients received treatment, three received ocriplasmin therapy, and three underwent PPV. Those eyes that underwent PPV had worse visual acuities prior to intervention.
Discussion
There has been a paradigm shift in the management of patients with VMT, macular pucker, ERM, and MH. A subset of patients with focal VMT, without ERM formation, with an FTMH (less than 400 μm), and/or severe symptoms can now be treated with ocriplasmin therapy instead of conventional PPV. This new medical vitreolysis approach is supported by high-level evidence from large, well-designed, randomized clinical trials and also by recent guidance issued by NICE. In this study, we set out to investigate the qualitative and quantitative aspects of the selection process involved in identifying suitable patients for ocriplasmin therapy, in order to understand the frequency and numbers of patients that meet the strict NICE guidance criteria for vitreolysis and also the multitude of factors that lead to selection of alternative forms of management, such as PPV or watchful waiting.
The most striking finding was the high frequency of VMT. Within a period of 3 months in a medium-size department, 3,472 patients received at least one OCT scan. Of this number, a total of 74 patients were found to have unilateral VMT and another 13 patients had bilateral VMT. This figure is a reflection of how commonly encountered focal VMT is in everyday practice. Many of these patients have coexisting pathologies, such as AMD, which require monthly visits, and this can lead to a false impression of a higher annual incidence rate of new cases of focal VMT. The true incidence of new cases of focal VMT is not known, as there have been few longitudinal population studies performed to capture the occurrence of new cases over time in a population. At the 20-year follow-up of the Beaver Dam eye study, VMT was present in 28 eyes in 24 individuals (1.6% of the 1,540 participants).26 Although the current study cannot give an accurate figure for incidence of VMT, assuming that each patient in our study represents a new case, we estimate the incidence to be approximately 2.5%. The comparatively high frequency of VMT in our study could be explained by a varying demographic. However, it could also represent the high fallout of patients in the Beaver Dam study (4,926 participants at baseline to 1,540 at 20 years), which reflects survival as opposed to participation. Due to the asymptomatic nature of VMT as reflected in this study, it is likely that any study involving symptomatic patients will underestimate the frequency of disease in the population.
Another finding was that of 87 patients with focal VMT in one or both eyes, 63 patients were not suitable for ocriplasmin therapy, as they were either asymptomatic or had associated ERM. This high proportion is in keeping with previous reports and meta-analyses of the rates of focal VMT in the overall population. This finding may justify the provision of separate guidelines for monitoring of these patients, so that early cases of MH can be detected and treated more promptly with either vitreolysis or surgery. The large proportion of patients in this category may represent a future public health issue or burden on resources.
Of 24 patients who satisfied the NICE criteria for ocriplasmin, only three eyes received this treatment. The reasons for noncompliance with the guidance were quite interesting and varied. Three patients who received vitrectomy typically had worse visual acuity compared to those treated with ocriplasmin, and these patients all opted for this treatment over ocriplasmin. Twelve eyes in ten patients were not treated, due to coexisting eye disease, in particular AMD of varying severity, considered the more likely cause for visual symptoms. The other reasons included partial or full resolution, patient refusal and patient nonattendance.
Our low numbers of patients treated with ocriplasmin did not agree with predicted figures that have been published. Amoaku et al predicted 10–20 patients would require treatment per 100,000 per year. From our figures, using a catchment population of 850,000, we estimate a frequency of ocriplasmin use at 1.4 per 100,000 per year.28 This discrepancy may well be partly due to the variation in patient selection for treatment and in particular the subjective interpretation of the definition of “symptomatic”, and what constitutes focal VMT on an OCT scan. Another factor may be the lack of guidance on coexisting macular pathology. A large proportion of cases of symptomatic focal VMT also had coexisting pathology. There may be different emphasis on the exclusion of patients with coexisting pathology between studies and between sites. Although NICE guidance does not explicitly exclude focal VMT with coexisting macular pathology to be treated with ocriplasmin, some clinicians (like ours) may still be excluding such patients, as they would not have been eligible for entry into the pivotal MIVI-TRUST (Microplasmin for Intravitreous Injection – Traction Release without Surgical Treatment) trials on which the NICE guidance was based.14 Another potential reason for excluding patients is refractive error. It is well known that eyes that are highly myopic are at increased risk of developing retinal detachment following PVD, and the presence of very early VD in myopic eyes has been recently reported using swept-source OCT.29 Although we did not capture any cases with myopia as copathology in any of the ocriplasmin-excluded cases in the 3-month study period, high myopia with pathological vitreous and retinal changes may be an additional factor that could deter selection of patients for ocriplasmin therapy.
In our study, we could not capture the stage of PVD in those eyes with VMT, as this was not a necessary criterion of selection of therapy for VMT at our site. However, as such imaging techniques as swept-source OCT become more widely available, the stage of PVD may become more reliable, as shown recently by Itakura et al and Uchino et al, and will undoubtedly play a more important role in the decision-making process for VMT therapy.29,30
Ocriplasmin represents a valuable alternative treatment option for patients with symptomatic focal VMT, which has been found by this and many other studies to be a commonly encountered condition. However, the number of cases suitable for ocriplasmin therapy may actually be quite low, and the main reasons for exclusion were lack of sufficient symptoms and the coexistence of another macular pathology. These subjective factors are not covered explicitly under NICE criteria, and future publication of real-world outcomes of ocriplasmin therapy should be interpreted cautiously, as there may be variation in patient selection. Clinicians in other departments with high attrition rates due to their selection process for ocriplasmin therapy may find our results of corroborative value. The large proportion of patients without significant symptoms may warrant the development of strategies to monitor such patients in a cost-effective way.
Acknowledgment
Institutional funding was received by Royal Wolverhampton Hospitals NHS Trust from Alcon and Thrombogenics for sponsored research studies on ocriplasmin.
Disclosure
Travel expenses, speaker fees, and honoraria for advisory boards were received by YCY from Thrombogenics, Alcon, Novartis, Bayer, Allergan, Alimera Sciences, Pfizer, Regeneron, and Genentech. Travel expenses and speaker fees were received by NN from Novartis and Bayer. The other authors report no conflicts of interest in this work.
References
Reese AB, Jones IS, Cooper WC. Vitreomacular traction syndrome confirmed histologically. Am J Ophthalmol. 1970;69(6):975–977. | ||
Sebag J. Age-related differences in the human vitreoretinal interface. Arch Ophthalmol. 1991;109(7):966–971. | ||
Duker JS, Kaiser PK, Binder S, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120(12):2611–2619. | ||
Sebag J. Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol. 2004; 242(8):690–698. | ||
Ezra E. Idiopathic full thickness macular hole: natural history and pathogenesis. Br J Ophthalmol. 2001;85(1):102–108. | ||
Johnson MW. Perifoveal vitreous detachment and its macular complications. Trans Am Ophthalmol Soc. 2005;103:537–567. | ||
Hikichi T, Yoshida A, Trempe CL. Course of vitreomacular traction syndrome. Am J Ophthalmol. 1995;119(1):55–61. | ||
Theodossiadis GP, Grigoropoulos VG, Theodoropoulou S, Datseris I, Theodossiadis PG. Spontaneous resolution of vitreomacular traction demonstrated by spectral-domain optical coherence tomography. Am J Ophthalmol. 2014;157(4):842–851.e1. | ||
Simpson AR, Petrarca R, Jackson TL. Vitreomacular adhesion and neovascular age-related macular degeneration. Surv Ophthalmol. 2012; 57(6):498–509. | ||
Johnson MW. Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol. 2010;149(3):371–382.e1. | ||
Spaide RF, Wong D, Fisher Y, Goldbaum M. Correlation of vitreous attachment and foveal deformation in early macular hole states. Am J Ophthalmol. 2002;133(2):226–229. | ||
Koerner F, Garweg J. Vitrectomy for macular pucker and vitreomacular traction syndrome. Doc Ophthalmol. 1999;97(3–4):449–458. | ||
Hermel M, Dailey W, Hartzer MK. Efficacy of plasmin, microplasmin, and streptokinase-plasmin complex for the in vitro degradation of fibronectin and laminin – implications for vitreoretinal surgery. Curr Eye Res. 2010;35(5):419–424. | ||
Stalmans P, Delaey C, de Smet MD, van Dijkman E, Pakola S. Intravitreal injection of microplasmin for treatment of vitreomacular adhesion: results of a prospective, randomized, sham-controlled phase II trial (the MIVI-IIT trial). Retina. 2010;30(7):1122–1127. | ||
Stalmans P, Benz MS, Gandorfer A, et al. Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med. 2012;367(7):606–615. | ||
Benz MS, Packo KH, Gonzalez V, et al. A placebo-controlled trial of microplasmin intravitreous injection to facilitate posterior vitreous detachment before vitrectomy. Ophthalmology. 2010;117(4):791–797. | ||
Varma R, Haller JA, Kaiser PK. Improvement in patient-reported visual function after ocriplasmin for vitreomacular adhesion: results of the Microplasmin for Intravitreous Injection – Traction Release Without Surgical Treatment (MIVI-TRUST) Trials. JAMA Ophthalmol. 2015;133(9):997–1004. | ||
Chatziralli I, Theodossiadis G, Parikakis E, Datseris I, Theodossiadis P. Real-life experience after intravitreal ocriplasmin for vitreomacular traction and macular hole: a spectral-domain optical coherence tomography prospective study. Graefes Arch Clin Exp Ophthalmol. Epub 2015 May 5. | ||
Sharma P, Juhn A, Houston SK, et al. Efficacy of intravitreal ocriplasmin on vitreomacular traction and full-thickness macular holes. Am J Ophthalmol. 2015;159(5):861–867.e2. | ||
Maier M, Abraham S, Frank C, Feucht N, Lohmann CP. [Ocriplasmin as a treatment option for symptomatic vitreomacular traction with and without macular hole: first clinical experiences]. Ophthalmologe. Epub 2015 Jun 11. German. | ||
Singh RP, Li A, Bedi R, et al. Anatomical and visual outcomes following ocriplasmin treatment for symptomatic vitreomacular traction syndrome. Br J Ophthalmol. 2014;98(3):356–360. | ||
Kim BT, Schwartz SG, Smiddy WE, et al. Initial outcomes following intravitreal ocriplasmin for treatment of symptomatic vitreomacular adhesion. Ophthalmic Surg Lasers Imaging Retina. 2013;44(4):334–343. | ||
Quezada-Ruiz C, Pieramici DJ, Nasir M, et al. Outer retina reflectivity changes on SD-OCT after intravitreal ocriplasmin for vitreomacular traction and macular hole. Retina. 2015;35(6):1144–1150. | ||
National Institute for Health and Care Excellence. Ocriplasmin for treating vitreomacular traction: NICE technology appraisal guidance [TA297]. 2013. Available from: https://www.nice.org.uk/guidance/ta297/resources. Accessed October 14, 2015. | ||
Fusi-Rubiano W, Awad M, Manjunath R, Elaraoud I, Narendran N, Yang Y. Spectrum of morphological and visual changes due to vitreomacular interface disorders encountered in a large consecutive cohort of patients. Eye (Lond). 2015;29(3):397–402. | ||
Meuer SM, Myers CE, Klein BE, et al. The epidemiology of vitreoretinal interface abnormalities as detected by spectral-domain optical coherence tomography: the Beaver Dam eye study. Ophthalmology. 2015;122(4):787–795. | ||
Jackson TL, Nicod E, Angelis A, et al. Vitreous attachment in age-related macular degeneration, diabetic macular edema, and retinal vein occlusion: a systematic review and metaanalysis. Retina. 2013;33(6):1099–1108. | ||
Amoaku W, Cackett P, Tyagi A, et al. Redesigning services for the management of vitreomacular traction and macular hole. Eye (Lond). 2014;28(Suppl 1):S1–S10. | ||
Itakura H, Kishi S, Li D, Nitta K, Akiyama H. Vitreous changes in high myopia observed by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2014;55(3):1447–1452. | ||
Uchino E, Uemura A, Ohba N. Initial stages of posterior vitreous detachment in healthy eyes of older persons evaluated by optical coherence tomography. Arch Ophthalmol. 2001;119(10):1475–1479. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.