Back to Journals » Clinical Interventions in Aging » Volume 17
Clinical Application Effects of Different Preoperative Blood Management Schemes in Older Patients with Delayed Intertrochanteric Fracture Surgery
Authors Cui Y, Lu Y , Huang Q, Zhang C, Sun L, Ren C, Wang Q, Ma T, Li Z, Zhang K, Wang Z, Xue H
Received 11 February 2022
Accepted for publication 14 May 2022
Published 20 May 2022 Volume 2022:17 Pages 825—835
DOI https://doi.org/10.2147/CIA.S362020
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Yu Cui,* Yao Lu,* Qiang Huang, Congming Zhang, Liang Sun, Cheng Ren, Qian Wang, Teng Ma, Zhong Li, Kun Zhang, Zhimeng Wang, Hanzhong Xue
Department of Orthopedics and Trauma, Hong Hui Hospital, Xi’an Jiaotong University College of Medicine, Xi’an, Shaanxi, 710000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhimeng Wang; Hanzhong Xue, Department of Orthopedics and Trauma, Hong Hui Hospital, Xi’an Jiaotong University College of Medicine, Xi’an, Shaanxi, 710000, People’s Republic of China, Email [email protected]; [email protected]
Introduction: Research on preoperative blood management in older patients with delayed surgery for intertrochanteric fracture is scarce, especially regarding hematopoiesis and hemostasis. We assessed the effectiveness of optimized blood management programs in older patients undergoing delayed surgery for intertrochanteric fractures.
Methods: This retrospective study included 456 patients who underwent delayed surgery for intertrochanteric fractures. According to the optimized blood management plan, the patients were divided into four groups: group A was the control group; group B received 1 g of tranexamic acid (TXA) intravenously at admission; group C underwent sequential TXA treatment after admission until 1 day before surgery (1 g/day); and group D received iron supplements (200 mg/day) in addition to the treatment administered to group C, with or without recombinant human erythropoietin (rHuEPO; 40,000 IU). The primary outcomes were preoperative hidden blood loss (HBL), preoperative allogeneic blood transfusion (ABT) rate, hemoglobin (Hb) change, and actual Hb drop.
Results: The Hb reduction, calculated HBL, and hospitalization duration in groups C and D were significantly lower than those in groups A and B. The preoperative ABT rates in groups C and D were significantly lower than those in groups A and B, with no significant difference between groups C and D.
Discussion: The results of this study suggested that iron supplementation (with or without rHuEPO) combined with the sequential IV TXA scheme did not show a better clinical effect than the sequential IV TXA scheme in the management of patients undergoing delayed surgery for intertrochanteric fractures. Therefore, further evaluation is needed before recommending iron supplements and rHuEPO in older patients.
Keywords: blood management, iron supplements, surgical delay, intertrochanteric fractures, tranexamic acid
Introduction
Owing to its large and rapidly aging population, China has the largest number of older people worldwide. Hip fractures have become a public health concern owing to their poor prognosis; thus, China is currently facing great challenges due to an increasing number of patients with hip fractures.1,2 A systematic analysis reported 1-year mortality rates after hip fracture and intertrochanteric fracture (IF) in China of 13.96% and 17.47%,3 respectively. Perioperative anemia is an important factor for mortality after hip fracture surgery and is closely related to the fracture type, such as intracapsular or extracapsular.4,5
Acute post-traumatic anemia and the need for transfusion in older patients with IFs are the major concerns for orthopedic surgeons. Pre-anemia increases the severity and incidence of postoperative anemia and increases the need for blood transfusion.6 Therefore, an ideal blood management program should include an attempt to minimize preoperative blood loss and to correct preoperative anemia.7 Post-traumatic hyperfibrinolysis is one of the most important causes of preoperative blood loss, and the administration of anti-fibrinolytic drugs is an effective treatment to reduce hidden blood loss (HBL).8 Previous studies have focused on tranexamic acid (TXA) to reduce intraoperative and postoperative hemorrhage in IFs;9–11 however, studies on occult hemorrhage before the operation are limited.12 Intravenous (IV) iron supplementation, with or without recombinant human erythropoietin (rHuEPO) therapy, has been proposed as an intervention to correct preoperative anemia.13 However, the actual clinical effects remain controversial.14,15 Strong evidence is lacking to support the preoperative clinical benefit of iron supplements and rHuEPO in older patients with IFs.
Over the past 8 years, we have been committed to perioperative blood management for older patients with hip fractures. Within this patient population, this study focuses on the management of patients undergoing delayed surgery for IFs. We have adopted a variety of intervention programs, including the administration of TXA, iron, and rHuEPO; however, the clinical effects of different application programs have not been effectively summarized. Therefore, we summarized the original data to evaluate (1) whether the optimized blood management plan was effective and safe; (2) compared with an early IV single injection of TXA, whether sequential TXA effectively reduced post-traumatic blood loss and allogeneic blood transfusion (ABT) rate; and (3) whether adding iron supplements, with or without rHuEPO, can further maintain hemoglobin (Hb) levels.
Materials and Methods
Patients
We conducted this retrospective large-scale self-censorship study at the Department of Orthopedics and Trauma, Hong Hui Hospital (level-1 trauma center) among older patients diagnosed with an IF and with an operative delay >72 h, between January 2013 and October 2020. All the data in this study were derived from two randomized controlled studies conducted in our department, which have been registered in the Chinese Clinical Trial Registry (ChiCTR-TRC-1800017754 and ChiCTR-INR-16008134). This study was approved by the hospital ethics committee (No. 201606008) and was conducted in accordance with the principles of the Declaration of Helsinki. All participating patients provided written informed consent.
The inclusion criteria were older patients with IF, age ≥65 years, injury time ≤12 h, and Hb level ≥110 g/L on PTA. The exclusion criteria were (1) polytrauma; (2) open fractures or continuous bleeding from other parts of the body, such as spleen rupture or gastrointestinal bleeding; (3) recent or continuous thromboembolic events and long-term consumption of oral anticoagulants before injury; (4) known allergies to TXA, rHuEPO, or iron supplements; (5) coagulation dysfunction caused by diffuse intravascular coagulation or liver and kidney dysfunction; (6) severe brain, heart, liver, or kidney dysfunction and patients who could not tolerate surgery; (7) patients with pathological fractures or tumors; (8) waiting time for post-traumatic to surgery >5 days; (9) American Society of Anesthesiologists (ASA) score of V; and (10) administration of any drugs, other than TXA, iron, and rHuEPO, that are conducive to hemostasis and hematopoiesis.
Study Design and Blood Management
The patients were divided into four groups according to the actual optimized blood management plan that they received at post-trauma admission (Table 1). The details of each strategy are described below.
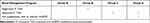 |
Table 1 Optimized Blood Management Program of the Four Groups |
Single-dose intravenous (IV) TXA: Patients were administered IV TXA (0.5 g; Tiancheng Pharmaceutical Co., Ltd., Changchun, China) 1 g (200 mL) immediately at PTA.
Sequential IV TXA: sequential TXA treatment after admission until 1 day before surgery (1 g/day).
Iron supplements, with or without rHuEPO: patients received additional IV iron supplements (200 mg/day, Hengsheng Pharmaceutical Co., Ltd., Nanjing, China), with or without rHuEPO (first dose: 40,000 IU, following doses: 10,000 IU; Shenyang 3SBio Inc., Shenyang, China). The indications for the discontinuation of iron supplementation and rHuEPO were: Hb level >130 g/L for male individuals and Hb level >120 g/L for female individuals.
Preoperative Management and Discharge Criteria
All patients were managed according to the standardized IF pathway protocol after admission, including blood pressure control, blood glucose monitoring, and standardized fluid and blood transfusion procedures.36 The only difference was in the above three main preoperative blood optimization management programs. In addition, according to the recommendations of the China Orthopedic Major Surgery Venous Thromboembolism Prevention Guidelines, all patients were treated with anticoagulants (enoxaparin, intrahepatic [IH] 20 mg qd) and intermittent compression boots as a preventive treatment for lower extremity venous thrombosis during hospitalization. If a positive result was observed on lower extremity vein ultrasound, the enoxaparin (IH) regimen was changed to bid. According to the agreement signed upon admission, the patients underwent IV ultrasound examinations of both lower extremities at the bedside every day during hospitalization and were examined at the outpatient clinic 14 and 30 days after discharge. Patients were discharged according to the following criteria: surgical incision without bleeding, an Hb level of >100 g/L, an albumin level of >30 g/L, and stable vital signs.
Data Collection
The hospital records contained data on age, sex, body mass index, preoperative blood volume, injury side, time from injury to operation, duration of operation, ASA classification, and AO fracture classification (A1/A2/A3). We noted the Hb and hematocrit (Hct) levels at PTA, day 2 of PTA, preoperatively, and on POD 1.
Outcome Measurements
Primary Outcomes
The primary outcomes in the present study were preoperative HBL, preoperative ABT rate, Hb change, and actual Hb drop. HBL was calculated using the Gross formula, as follows:37
HBL = PBV × (Hct1 - Hct2) + Hbtrans
Hct1= initial Hct level upon admission
Hct2 = lowest Hct level detected before surgery
The PBV was calculated using Nadler’s equation, as follows:38
PBV = K1×h3+K2×w+K3, [h: height (m), w: weight (kg)]
For male patients, K1 = 0.3669, K2 = 0.03219, and K3 = 0.6041
For female patients, K1 = 0.3561, K2 = 0.03308, and K3 = 0.1833
The ABT indications, formulated according to the guidelines of the Chinese Ministry of Health, were: (1) Hb level <70 g/L; (2) 70 g/L <Hb level <100 g/L; and (2) in patients with symptoms of dizziness, tachycardia, asthma, and fatigue. Because most older people are in a frail state before injury, our department and the anesthesiology department jointly developed a new blood transfusion strategy in which patients with Hb levels of <90 g/L received ABT preoperatively.11
Secondary Outcomes
The secondary outcomes included intraoperative and POD 1 blood transfusion rates and hospitalization duration. Complications, such as intramuscular venous thrombosis, DVT, and symptomatic PE, were recorded preoperatively. In addition, the incidence of 30-day mortality and 30-day all-cause re-admission were recorded through a review of existing medical data of the department. Clinically suspected PE was diagnosed based on clinical symptoms and findings from enhanced chest computed tomography scans.
Statistical Analyses
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 22.0, and GraphPad Prism, version 8.0. One-way analysis of variance and Tukey’s post-hoc tests were performed to analyze parametric data, while Kruskal–Wallis H and Mann–Whitney U-tests were applied to nonparametric data. Chi-square or Fisher’s tests were used for the analysis of qualitative variables. Statistical significance was set at P <0.05.
Results
Patient Demographics
A total of 833 consecutive patients with IFs were screened between January 2013 and October 2020, and their eligibility for participation in this study was assessed. Among these, 377 patients were excluded according to the exclusion criteria, including 38 aged <65 years, 124 with an injury time of >12 h, 73 with an Hb level of <110 g/L upon admission, 11 with polytrauma, 27 with long-term oral anticoagulants before injury, 4 with pathological fractures, 37 with a waiting time post-trauma to surgery of >5 days, 26 who received other hemostatic or hematopoietic medications after trauma, 18 lost to follow-up, and 19 who received non-proximal femoral nail anti-rotation fixation. Finally, this study enrolled a total of 456 patients with IFs (Figure 1). No significant differences in demographic data upon admission were found between the groups, and the baseline characteristics of the four groups were comparable (Table 2).
 |
Table 2 Baseline Characteristics |
 |
Figure 1 Flow diagram of patient selection. |
Primary Outcome
Figure 2A shows the mean Hb concentrations of the four treatment groups from post-trauma admission (PTA) to postoperative day (POD) 1, including the decreasing trends in each group. The comparison between groups showed a significant difference in the mean Hb values preoperatively and POD 1 (P<0.001).
The preoperative mean Hb values were 105.06±8.52 g/L, 106.59±9.04 g/L, 111.47±10.01 g/L, and 112.86±8.79 g/L in groups A, B, C, and D, respectively. The Hb values in groups A and B differed significantly from those in groups C and D but did not differ significantly for group A vs group B and group C vs group D (Figure 2B). The mean Hb values on POD 1 were 97.24±8.66, 99.29±9.58, 100.23±10.07, and 102.67±8.89 g/L in groups A, B, C, and D, respectively. The mean Hb values on POD1 differed significantly for groups C and D vs group A (P=0.014 and P<0.001, respectively). The values in group D also differed significantly from those in group B (P=0.008). No significant differences in the mean Hb values were observed between groups B and C (P=0.490) (Figure 2C). The average preoperative drops in Hb values in the four groups (21.48 g/L, 21.02 g/L, 17.36 g/L, and 16.55 g/L, respectively) were significant (P<0.001). Compared with groups A and B, groups C and D showed significant inter-group statistical differences (all P<0.001); however, pairwise comparisons between the groups showed that the differences between groups D and C and between groups B and A were not statistically significant (Figure 2D).
Figure 3 shows that the average preoperative HBL was 526±159 (range: 292–1063) mL in group A, 531±154 (range: 221–955) mL in group B, 466±115 (range 276–997) mL in group C, and 449±117 (range: 242–1168) mL in group D, with significant differences between the groups (P<0.001). Pairwise comparisons between groups showed significant differences for groups C and D compared with groups A and B (P<0.001) but no significant differences between groups A and B and groups C and D (P>0.05). The preoperative transfusion rates in groups B, C, and D were lower than those in group A, although the difference between the groups was not significant (P>0.05).
Secondary Outcomes
Compared with groups A (n=21) and B (n=17), groups C (n=12) and D (n=10) had fewer patients who required intraoperative ABT (P=0.104). The intraoperative blood loss and operation duration of the four groups of patients were similar, with no significant differences between the groups (all P>0.05). Similarly, fewer patients in groups C and D required ABT on POD 1 compared with those in groups A and B; however, the difference was not significant (P=0.353). Intermuscular vein thrombosis was the most common condition preoperatively, with 22 cases (17.40%) in group A, 15 (15.63%) in group B, 19 (16.37%) in group C, and 20 (16.95%) in group D. The incidence rates were similar among groups (P=0.986). No patients in any group experienced symptomatic pulmonary embolism (PE). Compared with patients in groups A and B, those in groups C and D showed a good effect regarding a shortened hospitalization duration (P<0.001). No difference was detected between groups C and D (P>0.05). According to the existing medical data of our department, 16 patients had been hospitalized within 30 days. Among them, four were admitted to the hospital due to poor blood sugar control, four with hypoproteinemia, two with redness and swelling, four with deep venous thrombosis (DVT), and two with stroke (Table 3).
 |
Table 3 Comparison of the Primary and Secondary Outcomes Among the Groups |
Discussion
The most important findings of the current study are as follows. First, post-traumatic administration of sequential IV TXA reduced the preoperative waiting period of HBL and maintained Hb levels without increasing the incidence of preoperative DVT. It also showed some benefits in reducing transfusion rates. Second, the patients did not receive additional benefits from the combined supplementary treatment plan (iron supplementation with or without rHuEPO). Finally, the early blood management intervention of patients should follow the conclusions of the CRASH-2 trial, in which the first IV single-dose TXA should be administered within 8 h post-trauma.
IFs cause substantial blood loss in older and frail patients, exposing them to preoperative anemia, which negatively impacts clinical outcomes and mortality.16,17 Wu et al18 reported that blood loss occurring between the time of fracture and operation is the main reason underlying decreased Hb levels, with significantly higher Hb decreases before the operation compared with after the operation. In their prospective analysis of perioperative hidden blood loss in 123 older patients with femoral IFs, Li et al19 observed an HBL in the preoperative waiting period of approximately 375.6 mL, which was 62.4% of the total HBL on POD 1 (602 mL) and 48.6% (772 mL) of the total HBL on POD 3. Therefore, blood management during the preoperative waiting period for older patients with delayed surgery is particularly important.
Two consecutive global multicenter studies showed that the early application of TXA effectively reduces the incidence of mortality due to traumatic bleeding.8,20 A prospective randomized controlled study by Ma et al12 confirmed that a single-dose IV TXA (1 g, 200 mL) interventional treatment in the early post-traumatic period of older patients with IF effectively reduced HBL. A pharmacokinetic study of TXA showed that its half-life is approximately 3 h. However, the high fibrinolytic state of the body due to trauma is persistent, and patients with severe trauma more often require transfusion support with red blood cells and plasma within 6 h.21 In addition, the use of anticoagulants, such as enoxaparin or rivaroxaban, after trauma, may cause new bleeding. Thus, a single dose of TXA in the early post-traumatic period cannot sufficiently inhibit hyperfibrinolysis; therefore, this finding provides the theoretical basis for multiple doses and sequential administration of IV TXA to inhibit fibrinolysis and to reduce HBL after trauma.
IV iron supplementation, with or without rHuEPO, before surgery, is considered a compelling potential intervention to increase Hb levels and to reduce perioperative transfusion exposure. Yoon et al22 applied a restrictive transfusion strategy combined with IV iron supplementation in 859 patients with hip fracture before surgery, reporting less total blood loss, lower blood transfusion rates, and higher Hb levels at 6 weeks after surgery. Muñoz et al23 conducted a pooled observational analysis of 2547 patients undergoing major orthopedic surgery (lower-limb arthroplasty and hip fracture repair), confirming that very short-term perioperative IV iron supplementation, with or without rHuEPO, was closely related to reduced transfusion rates and length of hospital stay. García-Erce et al24 reported that the preoperative administration of rHuEPO was associated with reduced transfusion requirements in patients with anemia due to hip fracture managed with perioperative IV iron and a restrictive transfusion protocol. However, some scholars remain skeptical about the clinical effects of IV iron supplementation. Jeong et al25 found that, although the serum iron profile of patients with IV iron supplementation improved, it could not increase the Hb level or reduce the transfusion rates among patients who underwent primary staged bilateral total knee arthroplasty during a single hospitalization. All of the abovementioned studies were observational. To date, there is no broad consensus or established clinical practice guideline to support the routine use of preventive IV iron supplementation, with or without rHuEPO, for the treatment of anemia before major elective surgery; furthermore, the best treatment timing, specific doses, and whether patients with anemia require additional nutritional supplements remain unclear.
This study is the first to investigate the effectiveness and safety of different preoperative blood optimization management programs for older patients with delayed IF surgery. The results showed lower HBL volumes for sequential IV TXA (group C) and iron supplementation treatment (with or without rHuEPO, group D) in the preoperative waiting period compared with the administration of single-dose TXA (group B) and the control group (group A); however, the HBL volume did not differ significantly between groups C and D (466.25±114.82 mL vs 448.66±116.83 mL, P=0.247). In the last laboratory results before surgery, the Hb levels of groups C and D were higher than those of groups A and B, with no significant difference between groups C and D. The decreases in Hb levels also showed the same trends. These findings indicated that the extended use of TXA, with or without iron and rHuEPO, reduced the HBL and actual Hb loss after admission. The findings regarding the preoperative transfusion rate also confirmed the advantages of the long-term use of TXA, with rates of 22.22%, 19.79%, 14.66%, and 14.41% for groups A, B, C, and D, respectively. Another important finding was that, theoretically, TXA intervention in the early post-traumatic period can reduce HBL; however, in this study, the HBL and Hb levels did not differ significantly between groups A and B. Our results showed a mean time from trauma to admission in the single-dose group of 8.77 h, which was higher than those reported in the CRASH-II trial (8 h)8 and by Ma et al (2 h).12 Therefore, early single-dose intervention should be administered within 8 h after trauma.
Preoperative sequential IV TXA (12 patients, 10.34%) and supplementation treatment (10 patients, 8.47%) programs also showed benefits in reducing the requirement for intraoperative transfusion compared with single-dose TXA (17 patients, 17.71%) and control programs (21 patients, 16.67%) (P=0.104). In addition, on POD 1, transfusions were required by 11 patients (8.73%) in the control group, 8 (8.33%) in the single-dose group, 8 (6.90%) in the sequential IV TXA group, and 4 (3.39%) in the supplementation treatment group. Groups C and D showed reduced blood transfusion rates during surgery and on POD 1 because good blood preservation before surgery can increase the tolerance of older patients to surgical trauma. A reduction in blood transfusion rate not only reduces the risk of infection in the blood but also contributes to a substantial reduction in healthcare costs and resource utilization for these patients.26 In addition, the length of stay differed significantly between the four groups in this study (P<0.001), with the length for groups C and D being significantly less than that for groups A and B. Therefore, good preoperative blood management can reduce post-trauma HBL and transfusion requirements due to IF in older patients, reduce the incidence of anemia, maintain high Hb levels during hospitalization, and shorten hospitalization duration, which is closely related to postoperative physical function recovery and the concept of enhanced recovery after surgery.27
While some studies have reported that delaying the operation time increases the probability of postoperative complications and mortality in older patients with hip fracture,28 other studies have shown no significant difference in the mortality of patients whose surgery is delayed by up to 3 days.29 The results of this study showed no mortality or serious adverse events within 30 days after the operation among the four groups. Surgeons have focused on the safety of IV TXA. Although many studies have reported administering the routine dose without increasing the risk of venous thromboembolism, there remains no consensus regarding the safety of higher doses or prolonged use.30,31 Conservation of blood products, reduced laboratory costs, and shorter hospital stays are likely the major factors driving the cost savings associated with TXA use.32 Similarly, the use of erythropoiesis agents increases the risk of thrombotic events.33 In this study, the incidence of venous thrombosis in the lower extremities did not differ significantly in the three groups and the incidence of venous thrombosis was comparable to the control group. IV iron supplementation can cause life-threatening hypersensitivity reactions, cardiovascular events, and infections.34 We did not encounter such adverse events in this study. These results are consistent with those of a previous systematic review that included 10,390 patients participating in 103 trials, which concluded that IV iron supplementation was not associated with adverse drug reactions or increased risk of infection.35
Although this was not a prospective randomized controlled study, it still has several strengths. Our study employed strict inclusion criteria; for older patients with an Hb level >110 g/L, it is difficult for doctors to pay attention to preoperative anemia and blood transfusion requirement in the clinic. However, the results of this study confirmed a declining trend in the Hb level of patients with delayed surgery. Furthermore, the time from injury to admission was strictly controlled to reduce potential interference. This study also has some limitations. First, this study only focused on hospitalization and a short follow-up period, which may not be sufficient to evaluate the clinical efficacy and safety of the treatment. Second, as the coagulation index was easily missed by the doctor during the post-trauma admission examination, it was excluded from this study. Third, when the Gross formula was obtained, considering the impact of dehydration on the Hb level upon admission, the Hb level upon admission was corrected to 0.9 to simulate 10% dehydration for all patients; however, rehydration following admission might have interfered with the accuracy of Hb measurements. Finally, a prospective study might better verify the effectiveness and safety of an optimized blood management program with the application of TXA, iron supplement, and rHuEPO in the older population with hip fractures.
Conclusion
Older patients with delayed IF surgery who received sequential IV TXA combined with iron supplementation, with or without rHuEPO, in the preoperative waiting period did not show better effects than those who received sequential IV TXA alone. Therefore, further evaluation is required before recommending iron supplementation to patients. In addition, if the patient undergoes early TXA intervention, the first IV time should be guaranteed within 8 h post-trauma.
Data Sharing Statement
Correspondence and requests for materials should be addressed to X.H.Z and Z.K.
Acknowledgments
This work was supported by the Project of Science and Technology Department of Shaanxi Province (Nos. 2016SF-340, 2017ZDXM-SF-009, and 2019JQ-976).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no competing interests.
References
1. Zhang C, Feng J, Wang S, et al. Incidence of and trends in hip fracture among adults in urban China: a nationwide retrospective cohort study. PLoS Med. 2020;17:e1003180. doi:10.1371/journal.pmed.1003180
2. Ren Y, Hu J, Lu B, Zhou W, Tan B. Prevalence and risk factors of hip fracture in a middle-aged and older Chinese population. Bone. 2019;122:143–149. doi:10.1016/j.bone.2019.02.020
3. Cui Z, Feng H, Meng X, et al. Age-specific 1-year mortality rates after hip fracture based on the populations in mainland China between the years 2000 and 2018: a systematic analysis. Arch Osteoporos. 2019;14:55. doi:10.1007/s11657-019-0604-3
4. Yombi JC, Putineanu DC, Cornu O, et al. Low haemoglobin at admission is associated with mortality after hip fractures in elderly patients. Bone Joint J. 2019;101-b:1122–1128. doi:10.1302/0301-620x.101b9.bjj-2019-0526.r1
5. Espinosa KA, Gélvez AG, Torres LP, García MF, Peña OR. Pre-operative factors associated with increased mortality in elderly patients with a hip fracture: a cohort study in a developing country. Injury. 2018;49:1162–1168. doi:10.1016/j.injury.2018.04.007
6. Dao P, Massin P. Blood management in enhanced recovery after hip and knee replacement. Orthop Traumatol Surg Res. 2020;106:S1–S5. doi:10.1016/j.otsr.2019.05.022
7. Zhang S, Huang Q, Xu B, et al. Effectiveness and safety of an optimized blood management program in total hip and knee arthroplasty: a large, single-center, retrospective study. Medicine. 2018;97:e9429. doi:10.1097/md.0000000000009429
8. Shakur H, Roberts I, Bautista R, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376:23–32. doi:10.1016/s0140-6736(10)60835-5
9. Farrow LS, Smith TO, Ashcroft GP, Myint PK. A systematic review of tranexamic acid in hip fracture surgery. Br J Clin Pharmacol. 2016;82:1458–1470. doi:10.1111/bcp.13079
10. Tian S, Shen Z, Liu Y, Zhang Y, Peng A. The effect of tranexamic acid on hidden bleeding in older intertrochanteric fracture patients treated with PFNA. Injury. 2018;49:680–684. doi:10.1016/j.injury.2018.01.026
11. Lei J, Zhang B, Cong Y, et al. Tranexamic acid reduces hidden blood loss in the treatment of intertrochanteric fractures with PFNA: a single-center randomized controlled trial. J Orthop Surg Res. 2017;12:124. doi:10.1186/s13018-017-0625-9
12. Ma H, Wang H, Long X, et al. Early intravenous tranexamic acid intervention reduces post-traumatic hidden blood loss in elderly patients with intertrochanteric fracture: a randomized controlled trial. J Orthop Surg Res. 2021;16:106. doi:10.1186/s13018-020-02166-8
13. Mueller MM, Van Remoortel H, Meybohm P, et al. Patient blood management: recommendations from the 2018 Frankfurt consensus conference. JAMA. 2019;321:983–997. doi:10.1001/jama.2019.0554
14. Bernabeu-Wittel M, Romero M, Ollero‐Baturone M, et al. Ferric carboxymaltose with or without erythropoietin in anemic patients with hip fracture: a randomized clinical trial. Transfusion. 2016;56:2199–2211. doi:10.1111/trf.13624
15. Koo CH, Shin HJ, Cho H, Ryu JH. The effect of perioperative intravenous iron on hemoglobin in surgical patients: a meta-analysis. J Surg Res. 2020;246:42–51. doi:10.1016/j.jss.2019.08.023
16. Gregersen M, Borris LC, Damsgaard EM. Postoperative blood transfusion strategy in frail, anemic elderly patients with hip fracture: the TRIFE randomized controlled trial. Acta Orthop. 2015;86:363–372. doi:10.3109/17453674.2015.1006980
17. Smith GH, Tsang J, Molyneux SG, White TO. The hidden blood loss after hip fracture. Injury. 2011;42:133–135. doi:10.1016/j.injury.2010.02.015
18. Wu JZ, Liu PC, Ge W, Cai M. A prospective study about the preoperative total blood loss in older people with hip fracture. Clin Interv Aging. 2016;11:1539–1543. doi:10.2147/cia.s120526
19. Li B, Li J, Wang S, Liu L. Clinical analysis of peri-operative hidden blood loss of elderly patients with intertrochanteric fractures treated by unreamed proximal femoral nail anti-rotation. Sci Rep. 2018;8:3225. doi:10.1038/s41598-018-21703-4
20. Roberts I, Roberts I, Shakur H, et al. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet. 2011;377:1096–1101. doi:10.1016/S0140-6736(11)60278-X
21. Banerjee A, Silliman CC, Moore EE, et al. Systemic hyperfibrinolysis after trauma: a pilot study of targeted proteomic analysis of superposed mechanisms in patient plasma. J Trauma Acute Care Surg. 2018;84:929–938. doi:10.1097/ta.0000000000001878
22. Yoon BH, Lee BS, Won H, et al. Preoperative iron supplementation and restrictive transfusion strategy in hip fracture surgery. Clin Orthop Surg. 2019;11:265–269. doi:10.4055/cios.2019.11.3.265
23. Muñoz M, Gómez-Ramírez S, Cuenca J, et al. Very-short-term perioperative intravenous iron administration and postoperative outcome in major orthopedic surgery: a pooled analysis of observational data from 2547 patients. Transfusion. 2014;54:289–299. doi:10.1111/trf.12195
24. García-Erce JA, Cuenca J, Haman-Alcober S, et al. Efficacy of preoperative recombinant human erythropoietin administration for reducing transfusion requirements in patients undergoing surgery for hip fracture repair. An observational cohort study. Vox Sanguinis. 2009;97:260–267. doi:10.1111/j.1423-0410.2009.01200.x
25. Jeong JH, Chang MJ, Kang S-B, et al. Postoperative intravenous iron supplementation does not improve hemoglobin level and transfusion rate following staged bilateral total knee arthroplasty. J Arthroplasty. 2020;35:2444–2450. doi:10.1016/j.arth.2020.04.086
26. Gupta PB, DeMario VM, Amin RM, et al. Patient blood management program improves blood use and clinical outcomes in orthopedic surgery. Anesthesiology. 2018;129:1082–1091. doi:10.1097/aln.0000000000002397
27. Kang Y, Liu J, Chen H, et al. Enhanced recovery after surgery (ERAS) in elective intertrochanteric fracture patients result in reduced length of hospital stay (LOS) without compromising functional outcome. J Orthop Surg Res. 2019;14:209. doi:10.1186/s13018-019-1238-2
28. Rosso F, Dettoni F, Bonasia DE, et al. Prognostic factors for mortality after hip fracture: operation within 48 hours is mandatory. Injury. 2016;47:S91–S97. doi:10.1016/j.injury.2016.07.055
29. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87:483–489. doi:10.2106/jbjs.d.01796
30. Raman T, Varlotta C, Vasquez-Montes D, Buckland AJ, Errico TJ. The use of tranexamic acid in adult spinal deformity: is there an optimal dosing strategy? Spine J. 2019;19:1690–1697. doi:10.1016/j.spinee.2019.06.012
31. Xie J, Hu Q, Ma J, Huang Q, Pei F. Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss and the inflammatory response following enhanced-recovery primary total hip arthroplasty: a randomised clinical trial. Bone Joint J. 2017;99-b:1442–1449. doi:10.1302/0301-620x.99b11.bjj-2017-0488.r1
32. Lin ZX, Woolf SK. Safety, efficacy, and cost-effectiveness of tranexamic acid in orthopedic surgery. Orthopedics. 2016;39:119–130. doi:10.3928/01477447-20160301-05
33. Unger EF, Thompson AM, Blank MJ, Temple R. Erythropoiesis-stimulating agents–time for a reevaluation. N Engl J Med. 2010;362:189–192. doi:10.1056/NEJMp0912328
34. Muñoz M, García-Erce JA, Villar I, Thomas D. Blood conservation strategies in major orthopaedic surgery: efficacy, safety and European regulations. Vox Sang. 2009;96:1–13. doi:10.1111/j.1423-0410.2008.01108.x
35. Avni T, Bieber A, Grossman A, et al. The safety of intravenous iron preparations: systematic review and meta-analysis. Mayo Clin Proc. 2015;90:12–23. doi:10.1016/j.mayocp.2014.10.007
36. Greenstein AS, Gorczyca JT. Orthopedic surgery and the geriatric patient. Clin Geriatr Med. 2019;35:65–92. doi:10.1016/j.cger.2018.08.007
37. Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58:277–280. doi:10.1097/00000542-198303000-00016
38. Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224–232.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


