Back to Journals » OncoTargets and Therapy » Volume 11
Cisplatin concurrent chemoradiotherapy vs adjuvant radiation in stage IB/IIA cervical cancer with intermediate risk factors, treated with radical surgery: a retrospective study
Authors Sun H, Tang Q, Chen J, Lv X, Tu Y, Yan D
Received 27 November 2017
Accepted for publication 16 January 2018
Published 6 March 2018 Volume 2018:11 Pages 1149—1155
DOI https://doi.org/10.2147/OTT.S158214
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ingrid Espinoza
Hai-Yan Sun, Qiu Tang, Jian-Hong Chen, Xiao-Juan Lv, Ye-Qiang Tu, Ding-Ding Yan
Department of Gynecologic Oncology, Zhejiang Cancer Hospital, Hangzhou, China
Purpose: To determine if postoperative cisplatin concurrent chemoradiotherapy (CCRT) improves the outcome in stage IA/IIB cervical cancer patients with intermediate risk factors, when compared with radiation therapy (RT) alone, and identify the potential eligible populations for this treatment.
Patients and methods: We reviewed medical records of 1,240 patients with stage IA/IIB cervical cancer who underwent radical hysterectomy and pelvic lymphadenectomy in our hospital between January 2008 and December 2011. Of the 1,240 patients, 436 displayed 1 or more intermediate risk factors. Of these, we screened 306 patients who underwent RT only or CCRT. We analyzed the effects of CCRT on survival and prognosis.
Results: The 5-year progress-free survival (PFS) in the CCRT group was superior to that in the RT-only group (96.0% vs 89.0%, respectively; P=0.031). The 5-year overall survivals (OSs) were not different between the 2 groups (P=0.141). Compared with RT-only group, CCRT did not improve PFS or OS in patients with 1 risk factor, large tumor size, or deep stromal invasion (P>0.05). Compared with RT-only group, CCRT improved PFS (97.9% vs 82.8%; P=0.017) but did not increase OS (97.9% vs 89.7%; P=0.109) in patients with lymphovascular space invasion plus deep stromal invasion/large tumor size. OS (92.3% vs 70.6%; P=0.048) and PFS (92.3% vs 64.7%; P=0.020) in the CCRT group were superior to those in the RT-only group with 3 risk factors. Compared with RT-only group, CCRT was an independent prognostic factor for favorable PFS (hazard ratio [HR] =0.238; 95% CI =0.0827–0.697, P=0.009) and OS (HR =0.192; 95% CI =0.069–0.533, P=0.002).
Conclusion: Postoperative CCRT improved survival in stage IA/IIB cervical cancer patients with intermediate risk factors. Patients with 2 or more intermediate risk factors, including lymphovascular space invasion, may benefit from CCRT.
Keywords: cervical cancer, concurrent chemoradiotherapy, intermediate risk factors
Introduction
In developing countries, cervical cancer ranks second among the most common malignant tumors in women.1 Radical hysterectomy with pelvic lymphadenectomy has been the treatment of choice for stage IA/IIB cervical cancer. Some risk factors have been identified that affect the survival of early-stage cervical cancer patients treated with radical surgery.2–6 Therefore, postoperative adjuvant radiotherapy or chemoradiotherapy is recommended, depending on risk factors. Positive pelvic nodes, parametrial invasion, and positive resection margins were considered high-risk factors;2,4 large tumor size (LTS), deep stromal invasion (DSI), and lymphovascular space invasion (LVSI) were recognized as intermediate risk factors.7–9 A randomized clinical trial showed that postoperative chemotherapy plus radiotherapy increased survival in high-risk patients.10 Compared with radiation therapy (RT) alone, concurrent chemoradiotherapy (CCRT) increased the 4-year overall survival (OS) from 71% to 80% and improved the 4-year progress-free survival (PFS) from 63% to 80%. CCRT is the standard treatment recommendation for postoperative treatment for early high-risk cervical cancer. Two other randomized controlled trials have shown that, compared with no further treatment, postoperative adjuvant radiotherapy reduces local recurrence and improves PFS in intermediate-risk cervical cancer patients.7,11 Postoperative radiotherapy is recommended for early cervical cancer with intermediate risk factors that meet the Sedlis criteria (category 1), according to the National Comprehensive Cancer Network guidelines. However, the advantage of postoperative CCRT is not clear. Currently, there are no prospective randomized controlled clinical trials investigating the impact of CCRT for intermediate-risk patients. We were able to identify 6 retrospective studies that gave inconsistent findings. Mabuchi et al found that CCRT prolonged PFS and OS.12 Similarly, Song et al13 observed that CCRT prolonged recurrence-free survival (RFS) and OS for intermediate-risk patients. However, another retrospective study reported that nedaplatin CCRT improved PFS but did not increase OS compared with the RT group in patents with 2 or more risk factors. Conversely, Nakamura et al14 reported that CCRT after radical hysterectomy did not confer benefit to intermediate-risk patients. In addition, the group who may benefit from CCRT was not clear. No standard criteria define who benefits from CCRT in cervical cancer patients with intermediate risk factors. Most previous studies analyzed the effect of CCRT on patients with various numbers of intermediate risk factors, but the relationship between the various combinations of risk factors and the efficacy of CCRT has not been analyzed.
To address these issues, we retrospectively studied the outcomes for intermediate-risk patients in our hospital to evaluate the impact of CCRT and identify the groups that might benefit from this treatment.
Patients and methods
Ethics statement
This study was approved by the institutional ethical review board of the Zhejiang Cancer Hospital. According to the Helsinki declaration, written informed consent was obtained from all patients.
Patients
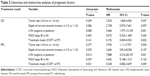
We obtained medical records of patients with stage IA/IIB cervical cancer who underwent radical hysterectomy and pelvic lymphadenectomy in our hospital between January 2008 and December 2011 (n=1,240). A total of 436 patients displayed at least one of the following intermediate risk factors: LVSI, depth of cervical stromal invasion >1/2, and tumor size >4 cm. Patients with high- or low-risk factors were excluded. Of the 436 intermediate-risk patients, the following patients were excluded: 49 patients had received neoadjuvant chemotherapy or adjuvant chemotherapy, 34 had fluorouracil plus cisplatin regimen CCRT, and 39 had paclitaxel plus cisplatin regimen CCRT. Of the remaining 306 patients, 182 received RT alone and 124 received cisplatin CCRT. A flowchart of the study population is shown in Figure 1. No difference was found in the pathological type and radiotherapy mode between RT-only group and the CCRT group (P>0.05). Compared with the RT-only group, the proportion of patients with a single risk factor in the CCRT group was lower, while those with 2 or 3 risk factors was higher (P<0.05). General patient characteristics are displayed in Table 1.
  | Figure 1 Flowchart of the study population. |
Radiotherapy
All patients received postoperative whole pelvic irradiation within 4–6 weeks after surgery. Pelvic radiotherapy was performed by the 4-field technique prior to 2010 and by 3-dimensional conformal radiotherapy or intensity-modulated radiotherapy after 2010. All eligible patients completed external RT, uniformly to the pelvis. The entire pelvis was irradiated with 4,500–5,400 cGy for a total of 25–28 fractions, 5 days per week.
Chemotherapy
Cis-diamminedichloroplatinum was given intravenously once a week during pelvic irradiation for 5 weeks. Chemotherapy was administered in 4–5 cycles, at a dose of 40 mg/m2.
Follow-up
OS was defined as the time from the beginning of radiotherapy to the patient’s death or the end of the final follow-up. PFS was defined as the time from the beginning of radiotherapy to metastasis or local recurrence of disease. After treatment, the patients were regularly reviewed as outpatients every 3 months in the first 2 years, every 6 months from the third to the fifth year, and every 12 months thereafter. CT with contrast of the chest and abdomen and contrast-enhanced MRI of the pelvis were performed every 6 months in the first 2 years and then yearly thereafter. Adverse effects, progression, and death were recorded.
Statistical analysis
SPSS 19 statistical software was used for data processing. The Kaplan–Meier method was used to calculate OS and PFS rates. The associations between OS and PFS and CCRT were determined by multivariate Cox proportional hazard models.
Results
Follow-up
The last follow-up was on December 31, 2011. Follow-up time was 6–94 months (median 61 months). A total of 18 patients were lost to follow-up, including 12 in the RT-only group and 6 in the CCRT group. The overall follow-up rate was 94.1%. In the second and the fifth year, 10 and 16 patients were lost to follow-up, respectively. These follow-up rates were 96.7% and 94.7%, respectively.
Treatment effect
At the end of the final follow-up period, a total of 20 patients died, including 15 in the RT-only group and 5 in the CCRT group. There were 22 patients with recurrence. Sites of recurrence in RT-only group were 7 local and 10 distant. Sites of recurrence in the CCRT group were 1 local and 4 distant. Table 2 displays the sites of the first recurrence and treatment regimen. Ten patients recurred in the first year, 8 in the second year, 1 in the third year, and 1 in the fourth year. Both local and distant recurrences were less frequent in patients receiving CCRT, but no statistically significant difference was found in terms of sites of recurrence between the 2 groups (P=0.160).
  | Table 2 Site of the first recurrence and treatment regimen |
The 5-year OS and PFS rates of the entire cohort were 91.8% and 93.5%, respectively. The 5-year PFS in the cisplatin CCRT group was superior to that in the RT-only group (96.0% vs 89.0%, respectively; P=0.031). However, no significant difference was found in the 5-year OS between the CCRT and RT-only groups (96.0% vs 91.8%, respectively; P=0.141).
To determine the effect of CCRT on patients with different intermediate risk factors, we tested all possible combinations of intermediate risk factors. Compared with RT-only group, CCRT did not improve OS and PFS in patients with 1 risk factor (P>0.05). Similarly, OS and PFS did not increase in patients with LTS and DSI (P>0.05). Compared with RT-only group, CCRT improved PFS (97.9% vs 82.8%; P=0.017) but did not increase OS (97.9% vs 89.7%; P=0.109) in patients with LVSI+DSI/LTS. OS (92.3% vs 70.6%; P=0.048) and PFS (92.3% vs 64.7%; P=0.020) in the CCRT group were superior to those in the RT-only group with 3 risk factors. Figure 2 shows the PFS and OS survival curves for the CCRT and RT-only groups with different intermediate risk factors.
Prognostic ability
Table 3 displays the results of analyses of OS and PFS by clinicopathological factors, including tumor size, depth of cervical stromal invasion, LVSI, stage, and treatment mode. Risks of recurrence and death were significantly higher in patients with positive LVSI, DSI, and LTS. However, addition of concurrent chemotherapy significantly reduced recurrence and prolonged survival. Compared with RT-only group, CCRT was an independent prognostic factor for favorable PFS (HR =0.238; 95% CI =0.0827–0.697, P=0.009) and OS (HR =0.192; 95% CI =0.069–0.533, P=0.002).
Discussion
In most previous studies, risk factors such as LTS, LVSI, or DSI were regarded as “intermediate-risk factors” when 2 or more of them were present. However, in our institution, from 2008 to 2012, the indications for postoperative radiotherapy included 1 or more risk factors (ie, LVSI, depth of cervical stromal invasion >1/2, and tumor size >4 cm). Studies found that adenosquamous carcinoma histology was an intermediate-risk factor predicting recurrence.15,16 In our study, adenocarcinoma accounted for a higher proportion in low- or high-risk patients, and most intermediate-risk adenocarcinoma patients underwent concurrent chemotherapy with fluorouracil plus cisplatin or paclitaxel plus cisplatin regimen. Therefore, only 3 adenocarcinoma patients were eligible for this study. We did not consider the effects of pathological type on prognosis. The proportion of LTS, LVSI, and DSI in the CCRT group was significantly higher than that in RT-only group. In other words, patients in the CCRT group had worse prognostic factors. Nevertheless, survival in the CCRT group was better compared with the RT-only group. Compared with the RT-only group, CCRT reduced local and distant recurrence and improved OS and PFS. CCRT was an independent prognostic factor for favorable PFS and OS. These results suggest that CCRT significantly improves survival in some patients with poor prognosis. Our results are consistent with those of previous studies.13,17
No standard criteria are available to define who benefits from CCRT in cervical cancer patients with intermediate risk factors. Most previous studies examined the impact of CCRT on survival with various numbers of intermediate risk factors.9,12–14,18 Kim et al found that chemoradiation improved RFS in cervical cancer patients with 1 or more intermediate risk factors.17 CCRT increased 3-year RFS in patients with 2 or more intermediate risk factors.13 Japanese investigators studied nedaplatin-based CCRT for efficacy in early cervical cancer patients with 1 or more risk factors.12,18 Their initial findings showed that nedaplatin-based CCRT improved 3-year PFS and OS in patients with 1 or more risk factors.12 However, with an increase in the total number of cases (from 57 to 129) and prolonged follow-up time (from 3 to 5 years), it turned out that CCRT only improved PFS in patients with 2 or 3 risk factors and showed no survival benefit in patients with only 1 risk factor.18 Taken together, these studies indicated that the benefits of chemotherapy can be predicted to some extent, according to the number of risk factors.
The classic criteria defined intermediate-risk group as 2 or more of the following: tumor size >2 cm, LVSI, and depth of cervical stromal invasion >1/3.2,8,9,19 But the Gynecologic Oncology Group (GOG), namely, the Sedlis criteria, defined the intermediate-risk group using various combinations of 3 factors (LVSI, DSI, and tumor size).3,7,19 Compared with the classic criteria, the Sedlis criteria have a more specific relationship with prognosis. The effect of CCRT on early-stage intermediate-risk cervical cancer patients is related to the number of risk factors, but it remains unclear as to the effect of CCRT in the context of combinations of risk factors. Our further subgroup analysis revealed that CCRT gave no substantial improvement of 5-year OS and PFS in patients with any 1 intermediate risk factor or 2 intermediate risk factors, including LTS and DSI. CCRT improved PFS but did not increase OS in patients with LVSI+DSI/LTS. PFS and OS in the CCRT group were superior to those in the RT-only group with 3 risk factors. Therefore, we speculate that patients with 2 or 3 intermediate risk factors, including LVSI, may potentially benefit from CCRT. In previous studies, subgroup analysis according to the number of risk factors may have hidden the effectiveness of chemotherapy because some relatively low-risk patients do not benefit from CCRT.9,18
In conclusion, we showed that postoperative CCRT improved survival in stage IA/IIB cervical cancer patients with intermediate risk factors. Patients with 2 or more intermediate risk factors, including LVSI, may benefit from CCRT. Previous studies have had the following shortcomings: small sample size,18 differences in the number of intermediate risk factors,12–14,18 inconsistent chemotherapy protocols,13,18 and short follow-up time.9,12 The shortcomings of these retrospective studies may have impacted the determination of the efficacy of CCRT in intermediate-risk patients. Compared with previous studies, our study has the advantages of large sample size, identical chemotherapy regimen, and >5 years of follow-up for living patients. Nevertheless, our study suffers from the same limitations as other retrospective studies. We expect that the GOG0263 Phase III clinical findings may identify the survival benefit of CCRT for early-stage cervical cancer patients, and the groups who may benefit from CCRT.
Disclosure
The authors report no conflicts of interest in this work.
References
Bermudez A, Bhatla N, Leung E. Cancer of the cervix uteri. Int J Gynaecol Obstet. 2015;131(Suppl 2):S88–S95. | ||
Samlal RA, van der Velden J, Schilthuis MS, et al. Identification of high-risk groups among node-positive patients with stage IB and IIA cervical carcinoma. Gynecol Oncol. 1997;64(3):463–467. | ||
Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol. 1990;38(3):352–357. | ||
Inoue T, Okumura M. Prognostic significance of parametrial extension in patients with cervical carcinoma Stages IB, IIA, and IIB. A study of 628 cases treated by radical hysterectomy and lymphadenectomy with or without postoperative irradiation. Cancer. 1984;54(8):1714–1719. | ||
Kamura T, Tsukamoto N, Tsuruchi N, et al. Multivariate analysis of the histopathologic prognostic factors of cervical cancer in patients undergoing radical hysterectomy. Cancer. 1992;69(1):181–186. | ||
Sevin BU, Lu Y, Bloch DA, Nadji M, Koechli OR, Averette HE. Surgically defined prognostic parameters in patients with early cervical carcinoma. A multivariate survival tree analysis. Cancer. 1996;78(7):1438–1446. | ||
Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: a Gynecologic Oncology Group Study. Gynecol Oncol. 1999;73(2):177–183. | ||
Van de Putte G, Lie AK, Vach W, Baekelandt M, Kristensen GB. Risk grouping in stage IB squamous cell cervical carcinoma. Gynecol Oncol. 2005;99(1):106–112. | ||
Ryu SY, Park SI, Nam BH, et al. Is adjuvant chemoradiotherapy overtreatment in cervical cancer patients with intermediate risk factors? Int J Radiat Oncol Biol Phys. 2011;79(3):794–799. | ||
Peters WA 3rd, Liu PY, Barrett RJ 2nd, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000;18(8):1606–1613. | ||
Rotman M, Sedlis A, Piedmonte MR, et al. A phase III randomized trial of postoperative pelvic irradiation in Stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006;65(1):169–176. | ||
Mabuchi S, Morishige K, Isohashi F, et al. Postoperative concurrent nedaplatin-based chemoradiotherapy improves survival in early-stage cervical cancer patients with adverse risk factors. Gynecol Oncol. 2009;115(3):482–487. | ||
Song S, Song C, Kim HJ, et al. 20 year experience of postoperative radiotherapy in IB-IIA cervical cancer patients with intermediate risk factors: impact of treatment period and concurrent chemotherapy. Gynecol Oncol. 2012;124(1):63–67. | ||
Nakamura K, Kitahara Y, Satoh T, et al. Analysis of the effect of adjuvant radiotherapy on outcomes and complications after radical hysterectomy in FIGO stage IB1 cervical cancer patients with intermediate risk factors (GOTIC Study). World J Surg Oncol. 2016;14(1):173. | ||
Ryu SY, Kim MH, Nam BH, et al. Intermediate-risk grouping of cervical cancer patients treated with radical hysterectomy: a Korean Gynecologic Oncology Group study. Br J Cancer. 2014;110(2):278–285. | ||
Noh JM, Park W, Kim YS, et al. Comparison of clinical outcomes of adenocarcinoma and adenosquamous carcinoma in uterine cervical cancer patients receiving surgical resection followed by radiotherapy: a multicenter retrospective study (KROG 13-10). Gynecol Oncol. 2014;132(3):618–623. | ||
Kim K, Kang SB, Chung HH, Kim JW, Park NH, Song YS. Comparison of chemoradiation with radiation as postoperative adjuvant therapy in cervical cancer patients with intermediate-risk factors. Eur J Surg Oncol. 2009;35(2):192–196. | ||
Okazawa M, Mabuchi S, Isohashi F, et al. Impact of the addition of concurrent chemotherapy to pelvic radiotherapy in surgically treated stage IB1-IIB cervical cancer patients with intermediate-risk or high-risk factors: a 13-year experience. Int J Gynecol Cancer. 2013;23(3):567–575. | ||
Delgado G, Bundy BN, Fowler WC Jr, et al. A prospective surgical pathological study of stage I squamous carcinoma of the cervix: a Gynecologic Oncology Group Study. Gynecol Oncol. 1989;35(3):314–320. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.