Back to Journals » International Journal of Nanomedicine » Volume 12
Chitosan-coated diacerein nanosuspensions as a platform for enhancing bioavailability and lowering side effects: preparation, characterization, and ex vivo/in vivo evaluation
Authors Allam AN , Hamdallah SI , Abdallah OY
Received 15 April 2017
Accepted for publication 9 June 2017
Published 4 July 2017 Volume 2017:12 Pages 4733—4745
DOI https://doi.org/10.2147/IJN.S139706
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Israel (Rudi) Rubinstein
Ahmed N Allam, Sherif I Hamdallah, Ossama Y Abdallah
Department of Pharmaceutics, Faculty of Pharmacy, Alexandria University, Alexandria, Egypt
Abstract: Nanodrug delivery systems have been widely reviewed for their use in several drug formulations to improve bioavailability, sustain effect, and decrease side effects of many candidate drugs. The objective of this study was to evaluate the potential of chitosan (CS)-coated nanosuspensions to enhance bioavailability and reduce the diarrheal side effect of diacerein (DCN) after oral administration. DCN nanosuspensions (DNS) were prepared by sonoprecipitation technique using different stabilizers at three different concentrations. The selected DNS with optimum particle size (PS), polydispersity index (PDI), and Zeta potential (ZP) was coated with three different concentrations of CS-coated DNS (CS-DNS) and screened. In vitro dissolution was performed for the selected lyophilized formulae and compared with DCN powder in addition to the assessment of drug crystallinity via scanning electron microscopy, X-ray powder diffraction, and differential scanning calorimetry. Ex vivo drug permeability using noneverted rat intestine, intraluminal content, and mucoadhesion evaluation was studied for nominated formulae in comparison to DCN suspension. Moreover, in vivo study, pharmacokinetic parameters, and evaluation of diarrheal potential were conducted after oral administration of selected formulae. Polyvinyl pyrrolidone (PVP)-stabilized DNS showed a significant increase (P≤0.05) in PS and PDI as the stabilizer concentration increased. PVP-stabilized DNS with the lowest CS concentration was protected from aggregation by lyophilization with mannitol. A remarked enhancement in dissolution parameters was observed in the nanocrystals’ formulae. Morphological examination and X-ray diffraction confirmed drug crystallinity. The intermediate permeation parameters of CS-DNS-F10, lowest rhein-to-DCN ratio in intraluminal content along with the highest percentage of mucoadhesive, could serve as a sustaining profile of coated formula. CS-DNS-F10 showed a significantly higher Cmax of 0.74±0.15 µg/mL at a delayed Tmax of 3.60±0.55 hours with a relative bioavailability of 172.1% compared to DCN suspension. CS-coated nanosuspensions could serve as promising revenue to enhance bioavailability and reduce the diarrheal side effect of DCN after oral administration.
Keywords: diacerein, nanosuspension, permeability, pharmacokinetics, chitosan, side effects
Introduction
Withdrawal of post-approval drugs because of their side effects can be triggered by data obtained from various sources such as clinical studies, systematic reviews, and animal data. The removal of such products from the market can result in loss of confidence in medications by the public and loss of effective compounds and loss of profit for drug manufacturers.1 According to the US Food and Drug Administration (FDA), a drug is usually withdrawn from the market because of safety concerns that cannot be corrected or when its risks overshadow its benefits.
Diacerein (DCN) is a drug used for the treatment of osteoarthritis (OA) at a dosage of 50–100 mg daily in two divided doses; it inhibits the synthesis and activity of interleukin 1-β (inflammatory mediator in OA). Being classified as a class II drug with low solubility and high permeability, poor dissolution rate and low oral bioavailability were reported.2,3 Consequently, a large portion of unabsorbed DCN remains in the intestine and reaches colon where it is hydrolyzed and converted into rhein (active metabolite of DCN) that possesses local stimulatory effect on the intestinal motility.3,4
On November 7, 2013, the European Medicines Agency (EMA) restricted the use of DCN-containing medicines because of major concerns about the frequency and severity of diarrhea in OA patients. Furthermore, the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) questioned the inadequate clinical benefits of DCN (due to its low bioavailability), which did not offset its risks. This report has vastly affected the market share of all DCN-containing medicines. On March 7, 2014, EMA had re-examined DCN-containing medicines and recommended that they remain available but with some limitations to manage the severity of diarrhea. Owing to the risks associated with severe diarrhea, DCN is no longer advised to patients aged ≥65 years. It is also recommended that patients start treatment on half the normal dose and should stop taking DCN if severe diarrhea occurs.5
Improving the bioavailability of DCN by enhancing its aqueous solubility and dissolution velocity could have a valuable effect on its clinical effectiveness and may lower its reported side effects. In this concern, many attempts have been reported to enhance DCN solubility, such as formulation as cyclodextrin complex,6 solid dispersions,7,8 microcrystals,9 noisomes,10 solid lipid nanoparticles,11–13 and nanocrystals.14 To the best of our knowledge, only Singh et al13 investigated the effect of formulation of DCN as solid lipid nanoparticles to enhance its lymphatic uptake and to reduce its diarrheal side effect.
Surface coating of nanodrug delivery system (NDDS) has been used as a mean for drug targeting in cancer and autoimmune diseases.15,16 Surface of NDDS may be modified with antibodies, tumor markers, fluorescent dyes, magnetic materials, carbohydrates, or mucoadhesive materials.17 It was reported that surface coating of NDDS with mucoadhesive could provide additional advantages to NDDS such as protection against degradation,18 localization of drug at the absorption window,19 and sustaining drug effect.20
Chitosan (CS) is a well-known cationic biodegradable polymer that was reported to enhance small intestine permeability.21 Nanoparticles coated with the polysaccharide CS have attracted a special interest for mucoadhesive applications, mainly, because of its ability to interact with the negatively charged mucosal surface and to increase the absorption of drugs by reorganizing tight junctions (TJ) between mucosal cells.22 Recently, the use of CS as surface coating for nanoparticle-medicated drug delivery in cancer was reported in many studies.23,24
The objective of this study is to evaluate the potential of nanoformulation and surface coating with mucoadhesive CS to enhance bioavailability and reduce the possible systemic and local diarrheal side effect of DCN after oral administration.
Materials and methods
Materials
DCN was supplied by Medizine Pharmaceutical Co. (Alexandria, Egypt); rhein was purchased from Nutragreenlife Biotechnology Co. (Shanxi, China). Poloxamer 188 (PLX188) was purchased from BASF (Ludwigshafen, Germany). CS (MW 100,000–300,000 Da) was purchased from Alpha Aeser (Ward Hill, MA, USA). Polyvinyl pyrrolidone (PVP) K25, sodium dodecyl sulfate (SDS), methylcellulose (MC), and dimethylsulfoxide (DMSO) were supplied by Al Amryia Pharmaceutical Co. (Alexandria, Egypt). All other reagents and chemicals used were of analytical grade.
Methods
Preparation of DCN nanosuspensions (DNS)
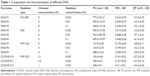
Nanosuspension formulae were prepared using sonoprecipitation method with slight modifications.25 Briefly, 50 mg of DCN was dissolved in DMSO, poured into an aqueous surfactant solution (50 mL) of PVP K25, PLX188, or SDS; each in a concentration of 0.025%, 0.05%, or 0.1% under stirring (IKA Labortechnik, Staufen im Breisgau, Germany) at 1,200 rpm in an ice bath for 30 seconds, and then a probe sonicator is immersed in the dispersion for 5 minutes at 40 kHz (Sonoplus HD 3100; BANDELIN, Berlin, Germany). The obtained nanosuspensions were centrifuged (Model 3K30; Sigma Laborzentrifugen GmbH, Osterode, Germany) at 16,000 rpm for 30 minutes at 4°C. Nine different DNS formulae were prepared, and all are listed in Table 1.
Particle size (PS), polydispersity index (PDI), and zeta potential (ZP)
The PS, PDI, and ZP of the prepared DNS were measured using dynamic light scattering technique (Zetasizer; Malvern Instruments, Malvern, UK) after suitable dilution (1:25) with Millipore-filtered deionized water. An aliquot of the nanosuspension was diluted before the measurement. Measurements were performed in triplicate and the results are presented as average value ±standard deviation (SD).
CS-coated DNS (CS-DNS)
For the preparation of CS-DNS, a method developed by Ramalingam et al26 was adapted. CS solution (5 mL) was added to freshly prepared selected DNS with continuous stirring (IKA Labortechnik) at 1,200 rpm for 60 minutes, and then the nanosuspension was centrifuged at 16,000 rpm for 30 minutes at 4°C. Three different CS-DNS formulae were prepared at different CS concentrations and were analyzed for PS, PDI, and ZP (Table 1).
Lyophilization of prepared nanosuspensions
Selected DNS and CS-DNS were lyophilized after preparation. The nanosuspensions were prefrozen using an ultracold freezer (Thermo Fisher Scientific, Waltham, MA, USA) at −80°C for 12 hours; then, the samples were freeze-dried using lyophilizer (Cryodos-50; Telstar, S.A., Terrassa, Spain) at −55°C and 90 mBar of pressure for 48 hours to yield dry powder. Moreover, mannitol (5%, w/v) was added into the dispersions prior to freezing as a cryoprotectant agent. PS, PDI, and ZP were examined for the lyophilized formulae after reconstitution, and the results were compared to those without cryoprotectant.
In vitro dissolution study
In vitro dissolution was performed for the selected lyophilized formulae (DNS-F7 and CS-DNS-F10) using an amount of drug equivalent to 5 mg in comparison to DCN powder. Dialysis bag diffusion technique was used.27 Dialysis membrane (Visking®, MWCO 12,000–14,000; SERVA, Heidelberg, Germany) was soaked in distilled water for 24 hours before the experiment. Samples were dispersed in 1 mL phosphate buffer in a dialysis bag of 5 cm length sealed hermetically and immersed in vials containing 15 mL sodium orthophosphate buffer 6.8 and were kept in a shaking water bath (Wisebath®, London, UK) at 37°C at 100 rpm. Samples were withdrawn at different time intervals up to 2 hours and replaced with an equal volume of dissolution medium. Samples were filtered and analyzed spectrophotometrically at the wavelength of 258 nm. Dissolution profile was expressed by the percentage diffused at 120 minutes (PD120), mean dissolution time (MDT), in addition to diffusion efficiency (DE).
Crystallinity assessment of nanocrystals
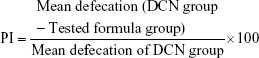
Differential scanning calorimetry (DSC)
Thermal behavior of DCN powder, PVP K25, CS, physical mixture (PM), DNS-F7, and CS-DNS-F10 was assessed using the DSC analysis (PerkinElmer Inc., Waltham, MA, USA). Samples were sealed in an aluminum crimp cell and heated at a speed of 10°C/minute from 30°C to 300°C under nitrogen atmosphere (60 mL/minute). A control empty pan was subjected to the same conditions.
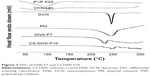
Powder X-ray diffraction (PXRD)
PXRD studies were investigated using an X-ray diffractometer. A copper radiation source was used as anode material. The diffraction pattern was performed in a step scan model with a voltage of 40 kV and a current of 40 mA in the range of 10°<2θ<40°, with a step size of 0.02°. The samples of DCN powder, PVP K25, CS, PM, DNS-F7, and CS-DNS-F10 were investigated.
Scanning electron microscopy (SEM)
Morphological structure of the freeze-dried DNS-F7 and CS-DNS-F10 was studied by SEM (100 CX; JEOL, Tokyo, Japan). Samples were fixed on supports and coated with gold-palladium under an argon atmosphere using a gold sputter. The morphology of different formulae was examined.
Ex vivo permeation
Experimental animal protocol
The animal experimental protocols for ex vivo study and diarrhea score test were performed in accordance with the European Community guidelines for the use of experimental animals and were approved by the Animal Care and Use Committee, Faculty of Pharmacy, Alexandria University. Healthy male rats, weighing ~200–250 g, were housed in polypropylene cages with free access to standard laboratory diet and water. They were kept at 25°C±1°C and 45%–55% relative humidity with a 12-hour light–dark cycle. The animals were fasted overnight before the experiment with free access to water.
The noneverted sac experiments were performed based on the method described by Ruan et al,28 and the rats were anesthetized by ether inhalation. A midline abdominal incision of 4–5 cm was made, and the small intestine was separated and washed with an oxygenated Krebs–Ringer solution using a syringe equipped with blunt end. The upper end of the duodenum and lower end of the ileum were separated into 12±0.5 cm long sacs having a diameter of 0.4 cm. Each sac was tied at one end, filled with 1 mL of 1 mg/mL of the tested formulae (DNS-F7 and CS-DNS-F10 in ringer at 6.8 and DCN in 0.3% carboxymethyl cellulose (CMC) in ringer at 6.8) via a 1 mL micropipette, and was sealed by tying the other end keeping effective sac length 10 cm for permeation.
Each noneverted rat intestinal sac was placed in a 25 mL glass beaker containing 10 mL permeation medium (mixture of Krebs–Ringer phosphate buffer saline pH 7.4 and isopropyl alcohol in the ratio of 7:3, v/v) at 37°C in a shaking water bath (Wisebath®) operating at 100 rpm and constantly aerated with oxygen (10–15 bubbles/minute) using laboratory aerator. At predetermined intervals (20, 40, 60, 90, and 120 minutes), samples of 0.5 mL were collected from outside of the sac and replaced with fresh medium. After filtration of samples through 0.22 μm Millipore syringe filter, an aliquot of 20 μL was injected into the high-performance liquid chromatography (HPLC) system. All formulae were tested in triplicates. Apparent permeability (Papp), lag time (LT), and diffusion coefficient (D) were the parameters used for the quantification of amount of drug permeated through the intestinal mucous membrane, which were calculated according to Bothiraja et al.29
Intraluminal perfusate and mucoadhesion
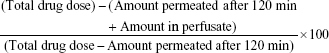
To measure the remaining amount of drug at the end of permeation study for the tested formulae compared to DCN suspension, the intestinal sacs were cut from one end and the intraluminal content was emptied by injecting air then perfused by injecting 5 mL of ringer solution, washed with 10 mL of DMSO, and sonicated in water bath for 5 minutes. The perfusates were filtered, and an aliquot of 20 μL was injected into the HPLC system. The percentage of mucoadhesion was calculated using the following equation:30
|
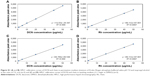
HPLC of DCN and rhein
A validated stability-indicting HPLC method31 was used for the quantification of amounts of DCN permeated as rhein through the noneverted gut sac and amounts of DCN/rhein in the perfusate of the intestinal lumen after predetermined intervals. Calibration curves of DCN and rhein in the permeation medium (mixture of Krebs–Ringer phosphate buffer saline, pH 7.4, and isopropyl alcohol in the ratio of 7:3, v/v) and in the intestinal lumen washing medium (1:1 ringer to DMSO) over the concentration range of 1–50 μg/mL (Figure S1) were obtained.
In vivo study
Experimental animal protocol
The animal experimental protocols for in vivo study and diarrhea score test were performed in accordance with the European Community guidelines for the use of experimental animals and were approved by the Animal Care and Use Committee, Faculty of Pharmacy, Alexandria University.
The study was done using male Wister albino rats (200±20 g). The study protocol followed institutional guidelines for the use of laboratory animals. Before initiation of the experiment, the animals were fasted for 10 hours with free access to water. Eighteen male rats were randomly divided into three groups (n=6), each group received a single oral dose of DNS-F7, CS-DNS-F10, or DCN with equivalent amount to 15 mg/kg body weight of animals.12,32 Blood samples (0.5 mL) were obtained from the retro-orbital plexus of rats and were drawn into EDTA tubes at intervals of 0.33, 0.66, 1, 1.5, 2, 3, 4, 6, 8, and 24 hours. The animals were sacrificed by an overdose of diethyl ether at the end of the experiment.
Preparation of plasma samples
Blood samples were centrifuged at 5,000 rpm for 10 minutes, 200 μL of plasma was mixed with 20 μL of 10% acetic acid for converting rhein into a nondissociating form.33 Then, 200 μL of acetonitrile was added, and the samples were vortexed (Vortex Mixer VM-300; Gemmy Industrial Corporation, Taipei, Taiwan) for 1 minute and sonicated in water bath for 5 minutes for the extraction of rhein. Samples were then centrifuged in a cooling centrifuge (Model 3K-30; Sigma Laboratory; Germany) at 10,000 rpm for 10 minutes at −20°C, and the supernatant was separated, filtered with 0.22 μm syringe filter, and injected in the HPLC system.
A validated stability-indicating HPLC methodology developed by Hamrapurkar et al31 for the determination of rhein was utilized with slight modification. The HPLC instrument (Agilent 1260 Series high-performance liquid chromatography; Agilent Technologies, Santa Clara, CA, USA) with a reversed-phase C18 column (150 cm × 4.6 mm; PS =3.5 μm) was equipped with a security guard ULTRA cartridges HPLC C18 (4.6 mm) (Phenomenex, Torrance, CA, USA). The best separation was achieved by the mobile phase of 50:50 (v/v) of water (pH adjusted to 2.9 with orthophosphoric acid):acetonitrile, at a flow rate of 1.0 mL/minute. The detection wavelength was set at 258 nm. A loop of 100 μL volume was used, and the samples were manually injected. Calibration curve of C concentration in plasma was plotted for quantification purpose. The linearity range of the method was 0.25–10 μg/mL, with a correlation coefficient (R2) of 0.9995. Intra- and interday precisions were represented by percentage of relative SD, which ranged from 1.2% to 3.85% and from 1.1% to 4.53%, respectively, and accuracy of the method, demonstrated by percentage of recovery, ranged from 98.25% to 101.54% and from 98.68% to 102.07%, respectively.
Pharmacokinetic study
Pharmacokinetic analysis of the data was performed using PKSolver, an add-in program for Microsoft excel.34 The area under the plasma concentration–time profile (AUC0–t and AUC0–inf) was calculated using the linear trapezoidal method. The elimination half-life (t1/2) was computed from the slope of the elimination phase of the log plasma concentration-time points plotted using the least square method. The maximum plasma concentration (Cmax) and the time to reach Cmax (Tmax) were determined. Data were expressed as the mean ± SD.
Diarrhea score test
Twenty-five male Wister albino rats weighing 200±20 g were randomly divided into five groups (n=5) and housed in the experiment household for a week before the experiment, and rats showing any diarrheal signs were excluded. All the animals were placed individually in separate cages along with standard diet pellets and water ad libitum for a week before starting the experiment for adaptation. Then, white sheets of paper were placed under the bottom of each cage for the observation of number, consistency, and collection of fecal droppings. Observations were done every 24 hours for five successive days. The five groups were treated orally with normal saline (negative control), DNS-F7, CS-DNS-F10, DCN, or rhein dispersed in 0.3% CMC (as positive control) with an equivalent amount to 50 mg/kg once daily for five successive days. The parameters observed include diarrhea score and percent inhibition (PI) in diarrhea. A numerical score from 1 to 3 based on stool consistency was assigned for normal, semisolid, and watery stools, respectively.35 PI was calculated as follows:36
|
Statistical analysis
Analysis of variance was conducted using the SPSS version 20.0 software (IBM Corporation, Armonk, NY, USA). A P-value of ≤0.05 was considered to be statistically significant.
Results and discussion
Sonoprecipitation technique was chosen for the preparation of nanosuspension due to the impact of ultrasonic waves on the mixing process and the nucleation rate; it provided sufficient micromixing at molecular level of mixture, which results in a rapid uniform distribution of solvents through the antisolvent beside the mesomixing provided by simple stirring for 30 seconds before sonication.25
Many preliminary trials were carried out to select optimum formulation and processing parameters influencing PS and PDI. These parameters include effect of antisolvent temperature, rate of the addition of solvent and antisolvent, order of addition, sonication time, and amplitude. Based on these preliminary trials, the formulation process has been tailored.
Measurement of PS, PDI, and ZP
Although several articles have discussed nanosuspensions, they lack a systematic understanding of stabilizer selection and nanosuspension stability; there are no systematic empirical or theoretical guidelines for stabilizer selection and optimization.37
The most common approaches of stabilization are steric and/or electrostatic techniques. Steric stabilization is achieved by adsorbing polymers onto the drug particle surface, whereas electrostatic stabilization is obtained by adsorbing charged molecules, both ionic surfactants and charged polymers, onto the particle surface. Based on that rationale, three stabilizers of different natures were used at three different concentrations (0.025%, 0.05%, and 0.1%) for formula optimization and characterization, such as a steric polymeric stabilizer (PVP K25), a nonionic surfactant stabilizer (PLX188), and an anionic surfactant stabilizer (SDS).
Results of the PS analysis are listed in Table 1. For PLX188- and SDS-stabilized formulae, a significant decrease in PS and PDI (P≤0.05) was observed as the stabilizer concentration increased, which can be explained based on their surface activity. As concentration increases, their influence on surface tension increases and energetic conditions are favorable with a maximum contact between the organic and aqueous phase,38 which could be translated into a decreased PS. Moreover, micelle formation at high PLX188 and SDS concentrations hinders their use, since they may solubilize the drug particles rather than stabilizing them.
For PVP K25-stabilized particles, a significant increase (P≤0.05) in PS and PDI was observed as the stabilizer concentration increased, which could be attributed to high affinity of PVP K25 to the hydrophobic surface of DCN particles that increase crystal growth reflected into large PS.39 Another possible factor is PVP K25’s viscosity-imparting property, where an increase in the aqueous phase viscosity decreases the impact of shear stress applied to the system; this may decrease the extent of size reduction.40
The values of ZP ranged from −22.1±3.65 to −37.1±4.41, which may be related to the intrinsic charge due to the ionization of DCN at pH of the dispersion medium (pH =4.88, whereas the pKa of DCN is 2.98). High ZP values indicate the physical stability of the prepared nanosuspensions with the low probability of aggregation and crystal growth.41
Based on the results of PS, PDI, and ZP, DNS-F7 was selected to be coated with different concentrations of CS and was screened for PS, PDI, and ZP to optimize the best formula for further studies.
CS-DNS
As listed in Table 1, an increase in PS and PDI of DNS-F7 was observed with increasing CS concentration, which may be ascribed to the accumulation of CS multilayers in the anchoring pattern of DCN nanoparticles that consequently increase the stagnant hydrated layer formed around the nanoparticles.42 This can also be confirmed by monitoring ZP of different coated formulae. ZP at the negatively charged surface of uncoated DNS-F7 was −28.8±6.11 mV, and after deposition of positively charged CS molecules, it ranged from +32.3±5.20 to +34.4±6.02 mV. This plateau in ZP values suggested a complete saturation of CS-DNS surface with the adsorbed positively charged CS.43 CS-DNS-F10 was selected as our nominated coated formula along with uncoated DNS-F7 for further studies.
Lyophilization of prepared nanosuspensions
Lyophilization was done to stabilize the prepared nanosuspensions and to prevent their crystal growth. The selected lyophilized formulae (DNS-F7 and CS-DNS-F10) were tested for their PS and PDI, after reconstitution, in the absence and presence of 5% mannitol as a cryoprotectant.
Without mannitol, it was obvious from Figure 1 that there was a significant increase in both PS and PDI values for the two examined formulae (P<0.05). Instead, mannitol protected the nanoparticles of DNS-F7 and CS-DNS-F10 from aggregation as the PS and PDI values were not significantly different from those before lyophilization (P>0.05). The lyophilized formulae using mannitol as cryoprotectant were used for other study experiments.
In vitro dissolution study
Since the process of transportation of drug molecules from formulae inside the dialysis bag to the recipient compartment through the dialysis membrane represents two processes such as drug dissolution and drug molecules diffusion; hence, the dialysis membrane method can be used to compare the dissolution of different DCN formulae. Sodium orthophosphate buffer (pH =6.8) was selected so that sink condition is guaranteed.
DCN dispersion showed a relatively slow diffusion rate (61.64% only was diffused after 120 minutes, PD120), as shown in Figure 2. In contrast, a remarked enhancement in dissolution was observed in the nanocrystals’ formulae (DNS-F7 and CS-DNS-F10); they exhibited 98.63% and 78.45% diffusion rates at the same time, respectively. The intermediate profile of CS-DNS-F10 along with expected mucoadhesive CS effect could serve as a sustaining effect of the coated nanocrystal formula.
MDT was 62.71 minutes in the case of DCN powder. Formula CS-DNS-F10 showed an insignificant decrease in the MDT of 57.47 minutes (P>0.05); further decrease was also observed in the case of DNS-F7 (36.19 minutes), which was significantly different from both the drug powder and CS-DNS-F10 (P<0.001). It was reported that the dissolution rate of a drug crystal is proportional to the available surface area for dissolution and PS reduction in addition to the thickness of the diffusion layer.44
DE is another parameter used to express dissolution profile between different formulae; it is the area under the diffusion curve up to certain time, t, expressed as a percentage of the area of the rectangle described by 100% diffusion in the same time.45
DNS-F7 and CS-DNS-F10 showed 1.6- and 1.2-fold increase in DE than that in DCN dispersion, respectively, which ensure the enhancement of the dissolution efficiency of DCN-NS and CS-DCN-NS over crude DCN powder due to size reduction.
Crystallinity assessment of nanocrystals
DSC
As shown in Figure 3, DCN has a sharp endothermic peak at 256°C, indicating its crystallinity. Such a finding agrees with that obtained by previous studies on DCN.8,13 Moreover, no endothermic peak was detected in the thermograms of CS and PVP K25. The drug characteristic peak was slightly shifted at lower intensity in the thermograms of PM and both formulae confirming the drug crystallinity. This might be attributed to the dilution effect of the drug with the excipients as previously reported.14 Finally, DSC was not a discriminative tool for explaining the changes that occurred in drug crystals during preparation, and further study using XRD is needed.
PXRD
X-ray diffraction was carried out to analyze the internal crystalline structure of DCN powder, DNS-F7, and CS-DNS-F10 and investigate the effect of formulation and surface coating on original crystalline structure. As shown in Figure 4, DCN powder had characteristic diffraction peaks at 10.51, 17.43, and 27.92°. Instead, PVP K25 and CS do not have any overlapping peaks with DCN diffractogram.
It was remarkable that the drug characteristic peaks were reserved but with weakened intensities in PM, DNS-F7, and CS-DNS-F10, which may be attributed to the dilution effect of excipients used rather than decreased or lack of crystallinity of the drug.14 This result confirmed that the sonoprecipitation had no effect on the DCN crystalline state, and the improved dissolution rate was due to size reduction rather than the formation of the amorphous form.
SEM
SEM of lyophilized DNS-F7 and CS-DNS-F10 is shown in Figure 4. The investigated formulae possessed crystalline particles in the nanorange of almost uniformly distributed PS, which led to the rapid penetration of water with dissolution enhancement.
Ex vivo permeation
Calibration curves of both DCN and rhein were obtained in both permeation medium (mixture of Krebs–Ringer phosphate buffer saline, pH 7.4, and isopropyl alcohol in the ratio of 7:3, v/v) and washing medium used in intestine rinsing (1:1 ringer in DMSO). A linear relationship over the concentration range of 1–50 μg/mL was observed with the correlation coefficient of 0.9998 and 0.999 in Krebs–Ringer phosphate buffer and 0.9997 and 0.9998 in 1:1 ringer to DMSO for DCN and rhein, respectively.
Ex vivo intestinal permeation by noneverted rat gut sacs can be used to determine the transport of various compounds from intestine, such as sugars, amino acids, and drugs, and evaluate the performance of novel drug delivery systems with high reliability and reproducibility.46
To provide a sink condition for permeation and taking into consideration the effect of solvent on the intestine viability, a mixture of Krebs–Ringer phosphate buffer saline, pH 7.4, and isopropyl alcohol in the ratio of 7:3 (v/v) was chosen in accordance with previous reports.47
It was noticed that all permeated drug was measured as rhein, which agreed with previous reports that DCN is completely converted into rhein before reaching the circulation.48
As shown in Figure 5, the cumulative amounts permeated after 120 minutes were 450.48±10.51, 108.28±1.06, and 97.83±6.53 μg for DNS-F7, CS-DNS-F10, and DCN suspension, respectively. Although there are too many reports suggesting that CS has a permeation enhancement effect21 either due to its effect on the TJ of the epithelial cells of intestine or by its mucoadhesive effect that keeps the drug molecules in intimate contact with the epithelial cells at the absorption site, Cs-DCN-NS did not show additional enhancement in DCN permeation through the intestinal wall. It was obvious that there is no significant difference (P>0.05) in amount permeated between coated nanocrystals (CS-DNS-F10) and DCN dispersion, which could be referred to the shielding effect of CS coat around the formed nanoparticle in the permeation medium.
Table 2 shows different permeation parameters used for the quantification of amount of drug permeated through the intestinal mucous membrane. DNS-F7 has the highest Papp and diffusion coefficient (D) with the shortest LT compared to other tested formulae. The intermediate permeation parameters of CS-DNS-F10 along with expected mucoadhesive CS effect could serve as a sustaining profile of coated nanocrystal formula.
  | Table 2 Permeation parameters of DCN suspension, DNS-F7, and CS-DNS-F10 |
Intraluminal perfusate and mucoadhesion
The perfusion medium used to wash the intestinal lumen at the end of experiment was analyzed. It was quite valuable to find that the nonpermeated DCN was not totally converted to its active metabolite rhein, and the total amount found in the analyzed perfusate was 257±35.6, 268.4±15.6, and 746.03±45.2 μg for DNS-F7, CS-DNS-F10, and DCN suspension, respectively, as shown in Figure 5.
In general, DCN dispersion showed statistically (P<0.05) significant higher rhein amounts (468.63 μg out of 746.03 μg) over all other formulae; similarly, DNS-F7 also showed high rhein-to-DCN ratio (199.26 μg out of 257 μg), which can be attributed to large surface area of the nanoparticulate DCN formula that facilitates the degradation process, but the absolute amount of rhein remained is still lower than that of DCN dispersion due to the enhanced permeation of DNS-F7 over DCN suspension. Regarding CS-DNS-F10, it showed the lowest rhein-to-DCN ratio (123.31 μg out of 268.4 μg), which may be ascribed to the shielding effect of CS in the permeation medium around the unabsorbed DCN particles that may have a potential effect in lowering the diarrheal side effect of DCN.
Cumulative amounts retained in tissue were calculated by subtracting the summation of amount permeated and perfusate from initial drug added; CS-DNS-F10 showed the highest amount retained (623.44 μg) followed by DNS-F7 (293.26 μg) and DCN suspension (156.14 μg).
To examine the mucoadhesive properties of nanoparticles and CS-coated nanoparticles compared to DCN suspension, the equation adapted by Goto et al30 was used. Both DNS-F7 and CS-DNS-F10 showed a statistically significant (P<0.05) difference compared to DCN suspension. The percentage of mucoadhesion was 53.2, 69.89, and 17.31 for DNS-F7, CS-DNS-F10, and DCN suspension, respectively.
The oral administration of nanoparticle suspensions leads to mucoadhesion of a significant fraction of the particles; clearly, part of the particles is captured by the mucus gel layer, while the remaining particles undergo unmodified transit.49 It is expected that CS-DNS-F10 would show additional mucoadhesive properties in the acidic medium in the stomach and the upper part of intestine due to the deposition of positive charge of CS in acidic medium, which in turn may affect the total drug bioavailability; at the same time, the particles that would not adhere will go through the alkaline medium of intestine, where CS will precipitate on the surface of particles providing a shield preventing unabsorbed DCN from hydrolysis into rhein that is responsible for the diarrheal side effect.32
In vivo study
Under chromatographical conditions applied, rhein showed a sharp and symmetrical peak with minimum tailing. No interfering peaks from endogenous substances present in plasma were detected in the chromatogram. The standard curve was linear over the calibration range of 0.2–10 μg/mL with correlation coefficient =0.999.
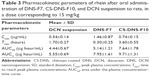
The rhein mean plasma concentration–time curve after oral administration of DNS-F7, CS-DNS-F10, and DCN suspension to rats in a dose corresponding to 15 mg/kg are shown in Figure 6, and the corresponding pharmacokinetics parameters are listed in Table 3.
After oral administration, DCN metabolized into rhein before entering the systemic circulation; DNS-F7 reached a significantly (P<0.05) higher Cmax of 1.46±0.87 μg/mL at the Tmax of 0.3±0.27 hours, while DCN suspension reached a Cmax of 0.537±0.14 μg/mL at the Tmax of 1.7±0.27 hours, and the mean AUC values of DNS-F7 showed significantly (P<0.05) higher values compared to DCN suspension of 5.14±1.2 and 4.44±0.67 μg hour/mL, respectively, which resulted in a relative bioavailability of 115.8%. Concerning CS-DNS-F10, it showed a significant higher Cmax of 0.74±0.15 μg/mL at a delayed Tmax of 3.60±0.55 hours with a relative bioavailability of 172.1% compared to DCN suspension. The slight increase in Cmax along with the delayed Tmax could serve as promising revenue to avoid the high peaking level of rhein in plasma that may be responsible for the systemic diarrheal side effect of DCN after oral administration.
Diarrhea score test
Since DCN has a property to cause diarrhea as a side effect that is attributed to the hydrolysis of the unabsorbed portion of DCN into rhein.50 Therefore, diarrhea score test was carried out to investigate the effect of the prepared formulae in minimizing diarrhea.
As shown in Figure 7, high diarrhea scores were recorded for both DCN and rhein with no significant difference (P>0.05). Nanosizing of DCN in DNS-F7 also showed a high diarrheal score comparable to that of DCN, but at lower extent, this may be explained by the large surface area of nanoparticles due to the enhanced absorption due to the improvement in dissolution and permeation of the formula which agreed with dissolution and ex vivo permeation studies. In contrast, CS-DNS-F10 did not show any statistically significant difference (P>0.05) with the control group that received saline solution, which reinforces our hypothesis that CS coating of DCN nanosuspension could be advantageous in minimizing the diarrheal side effect of our candidate drug by preventing unabsorbed DCN from converting into rhein that is responsible for the diarrheal side effect.
  | Figure 7 Diarrheal score for different formulae with a dose of 50 mg/kg for 5 successive days. |
To measure the extent of diarrhea inhibition by the tested formulae compared to the side effect of DCN dispersion expressed as diarrhea score, PI was calculated. DNS-F7 showed a PI range from 5.78% to 18.79%, whereas CS-DNS-F10 showed a higher PI range from 23.23% to 57.01%, which is another evidence for the above suggestion.
Conclusion
In the current study, nanocrystallization was developed to enhance bioavailability and decrease the side effects of DCN after oral administration. Formulations were successfully achieved through simple sonoprecipitation technique and further coated with mucoadhesive CS polymer. PVP-stabilized DNS with the lowest CS concentration provided optimum PS, PDI with modulated release of DCN, and intermediate permeation along with reasonable pharmacokinetic parameters, and diarrheal score percent could serve as a promising strategy to enhance bioavailability and reduce the diarrheal side effect of DCN after oral administration. Improvement of bioavailability through NDDSs could support the recommendations of EMA’s PRAC in starting DCN treatment with half the normal dose, which subsequently decrease the systemic side effect of absorbed rhein in plasma. Furthermore, the local GIT irritation due to the degradation of unabsorbed DCN could be minimized by surface coating of DCN nanosuspension, which could be advantageous in decreasing the diarrheal side effect of DCN by preventing unabsorbed DCN from converting into rhein that is responsible for the diarrheal side effect.
Disclosure
The authors report no conflicts of interest in this work.
References
Onakpoya IJ, Heneghan CJ, Aronson JK. Post-marketing withdrawal of 462 medicinal products because of adverse drug reactions: a systematic review of the world literature. BMC Med. 2016;14:10. | ||
Mahajan A, Singh K, Tandon VR, Kumar S, Kumar H. Diacerein: a new symptomatic slow acting drug for osteoarthritis. J Med Educ Res. 2006;8:173–175. | ||
Kongtharvonskul J, Anothaisintawee T, McEvoy M, Attia J, Woratanarat P, Thakkinstian A. Efficacy and safety of glucosamine, diacerein, and NSAIDs in osteoarthritis knee: a systematic review and network meta-analysis. Eur J Med Res. 2015;20:24. | ||
Panova E, Jones G. Benefit and risk assessment of diacerein in the treatment of osteoarthritis. Drug Saf. 2015;38(3):245–252. | ||
Pavelka K, Bruyere O, Cooper C, Kanis J, Leeb B, Maheu E. Diacerein: benefits, risks and place in the management of osteoarthritis. An opinion-based report from the ESCEO. Drugs Aging. 2016;33(2):75–85. | ||
Maski N, Girhepunje K, Ghode P, Pal R. Studies on the preparation, characterization and solubility of B-cyclodextrin – diacerein inclusion complexes. Int J Pharm Pharm Sci. 2009;1:121–135. | ||
Deshmukh DB, Gaikwad PD, Bankar VH, Pawar SP. Dissolution enhancement of poorly water soluble diacerein by solid dispersion technique. J Pharm Sci Res. 2010;2:734–739. | ||
Patil SB, Shete DK, Narade SB, et al. Improvement in the dissolution profile of diacerein using a surfactant-based solid dispersion technique. Drug Discov Ther. 2010;4(6):435–441. | ||
Yadav DS, Yadav AA, Karekar PS, Pore YV, Gajare PS. Preparation and characterization of Diacerein microcrystals. Der Pharm Lett. 2012;4:428–435. | ||
Zaki RM, Ali AA, El Menshawe SF, Bary AA. Formulation and in vitro evalution of diacerein loaded niosomes. Int J Pharm Pharm Sci. 2014;6:515–521. | ||
Rehman M, Madni A, Ihsan A, et al. Solid and liquid lipid-based binary solid lipid nanoparticles of diacerein: in vitro evaluation of sustained release, simultaneous loading of gold nanoparticles, and potential thermoresponsive behavior. Int J Nanomedicine. 2015;10:2805–2814. | ||
Jain A, Mishra SK, Vuddanda PR, Singh SK, Singh R, Singh S. Targeting of diacerein loaded lipid nanoparticles to intra-articular cartilage using chondroitin sulfate as homing carrier for treatment of osteoarthritis in rats. Nanomedicine. 2014;10(5):1031–1040. | ||
Singh S, Jain A, Singh SK, Singh Y. Development of lipid nanoparticles of diacerein, an antiosteoarthritic drug for enhancement in bioavailability and reduction in its side effects. J Biomed Nanotechnol. 2013;9(5):891–900. | ||
Elsayed I, Abdelbary AA, Elshafeey AH. Nanosizing of a poorly soluble drug: technique optimization, factorial analysis, and pharmacokinetic study in healthy human volunteers. Int J Nanomedicine. 2014;9:2943–2953. | ||
Win KY, Feng SS. Effects of particle size and surface coating on cellular uptake of polymeric nanoparticles for oral delivery of anticancer drugs. Biomaterials. 2005;26(15):2713–2722. | ||
Qie Y, Yuan H, von Roemeling CA, et al. Surface modification of nanoparticles enables selective evasion of phagocytic clearance by distinct macrophage phenotypes. Sci Rep. 2016;6:26269. | ||
Van Rijt SH, Bein T, Meiners S. Medical nanoparticles for next generation drug delivery to the lungs. Eur Respir J. 2014;44(3):765–774. | ||
Patel DJ, Patel JK. Mucoadhesive effect of polyethyleneoxide on famotidine nanosuspension prepared by solvent evaporation method. Int J Pharm Pharm Sci. 2010;2:122–127. | ||
Mazzarino L, Borsali R, Lemos-Senna E. Mucoadhesive films containing chitosan-coated nanoparticles: a new strategy for buccal curcumin release. J Pharm Sci Res. 2014;103(11):3764–3771. | ||
Sosnik A, Das Neves J, Sarmento B. Mucoadhesive polymers in the design of nano-drug delivery systems for administration by non-parenteral routes: a review. Prog Polym Sci. 2014;39:2030–2075. | ||
Thanou M, Verhoef JC, Junginger HE. Chitosan and its derivatives as intestinal absorption enhancers. Adv Drug Deliv Rev. 2001;50(suppl 1):91–101. | ||
Nagarajan E, Shanmugasundaram P, Ravichandiran V, Vijayalakshmi A, Senthilnathan B, Masilamani K. Development and evaluation of chitosan based polymeric nanoparticles of an antiulcer drug lansoprazole. J Appl Pharm Sci. 2015;5:20–25. | ||
Wang H, Wu J, Xu L, Xie K, Chenb C, Dong Y. Albumin nanoparticle encapsulation of potent cytotoxic therapeutics shows sustained drug release and alleviates cancer drug toxicity. Chem Commun. 2017;53(17):2618–2621. | ||
Jiang C, Wang H, Zhang X, et al. Deoxycholic acid-modified chitooligosaccharide/mPEG-PDLLA mixed micelles loaded with paclitaxel for enhanced antitumor efficacy. Int J Pharm. 2014;475(1–2):60–68. | ||
Dhumal RS, Biradar SV, Yamamura S, Paradkar AR, York P. Preparation of amorphous cefuroxime axetil nanoparticles by sonoprecipitation for enhancement of bioavailability. Eur J Pharm Biopharm. 2008;70(1):109–115. | ||
Ramalingam P, Yu SW, Ko YT. Nanodelivery systems based on mucoadhesive polymer coated solid lipid nanoparticles to improve the oral intake of food curcumin. Food Res Int. 2016;84:113–119. | ||
Souza SD. A review of in vitro drug release test methods for nano-sized dosage forms. Adv Pharm. 2014;2014:304757, 1–12. | ||
Ruan L, Chen S, Yu BY, Zhu DN, Cordell GA, Qiu SX. Prediction of human absorption of natural compounds by the non-everted rat intestinal sac model. Eur J Med Chem. 2006;41(5):605–610. | ||
Bothiraja C, Pawar AP, Dama GY, Joshi PP, Shaikh KS. Novel solvent-free gelucire extract of Plumbago zeylanica using non-everted rat intestinal sac method for improved therapeutic efficacy of plumbagin. J Pharmacol Toxicol Methods. 2012;66(1):35–42. | ||
Goto T, Morishita M, Kavimandan NJ, Takayama K, Peppas NA. Gastrointestinal transit and mucoadhesive characteristics of complexation hydrogels in rats. J Pharm Sci Res. 2006;95(2):462–469. | ||
Hamrapurkar P, Patil P, Desai M, Phale M, Pawar SP. Stress degradation studies and development of a validated stability-indicating-assay-method for determination of diacerein in presence of degradation products. Pharm Methods. 2011;2(1):30–35. | ||
El-Laithy HM, Basalious EB, El-Hoseiny BM, Adel MM. Novel self-nanoemulsifying self-nanosuspension (SNESNS) for enhancing oral bioavailability of diacerein: simultaneous portal blood absorption and lymphatic delivery. Int J Pharm. 2015;490(1–2):146–154. | ||
Yaroshenko IS, Khaimenov AY, Grigoriev AV, Sidorova AA. Determination of Rhein in blood plasma by HPLC with UV detection and its application to the study of bioequivalence. J Anal Chem. 2014;69:793–799. | ||
Zhang Y, Huo M, Zhou J, Xie S. PKSolver: an add-in program for pharmacokinetic and pharmacodynamic data analysis in Microsoft excel. Comput Methods Programs Biomed. 2010;99(3):306–314. | ||
Yagi T, Miyawaki Y, Nishikawa A, Yamauchi K, Kuwano S. Suppression of the purgative action of rhein anthrone, the active metabolite of sennosides A and B, by indomethacin in rats. J Pharm Pharmacol. 1991;43(5):307–310. | ||
Taufiqul Islam A, Erfan Uddin M, Chowdhury M, Rahman M, Habib M, Rahman A. In vivo antidiarrheal and cytotoxic potential of different fractions of Pandanus foetidus leaves. Am J Biomed Sci. 2013;5:208–216. | ||
Ghosh I, Bose S, Vippagunta R, Harmon F. Nanosuspension for improving the bioavailability of a poorly soluble drug and screening of stabilizing agents to inhibit crystal growth. Int J Pharm Pharm Sci. 2011;409(1–2):260–268. | ||
Rowe RC, Sheskey PJ, Quinn ME. Handbook of Pharmaceutical Excipients. 6th ed. London: Pharmaceutical Press, American Pharmacists Association; 2009. | ||
Choi JY, Yoo JY, Kwak HS, Uk Nam B, Lee J. Role of polymeric stabilizers for drug nanocrystal dispersions. Curr Appl Phys. 2005;5:472–474. | ||
El-Habashy SE, Allam AN, El-Kamel AH. Ethyl cellulose nanoparticles as a platform to decrease ulcerogenic potential of piroxicam: formulation and in vitro/in vivo evaluation. Int J Nanomedicine. 2016;11:2369–2380. | ||
Verma S, Kumar S, Gokhale R, Burgess DJ. Physical stability of nanosuspensions: investigation of the role of stabilizers on Ostwald ripening. Int J Pharm. 2011;406(1–2):145–152. | ||
Guo C, Gemeinhart RA. Understanding the adsorption mechanism of chitosan onto poly(lactide-co-glycolide) particles. Eur J Pharm Biopharm. 2008;70(2):597–604. | ||
Quan P, Shi K, Piao H, et al. A novel surface modified nitrendipine nanocrystals with enhancement of bioavailability and stability. Int J Pharm. 2012;430(1–2):366–371. | ||
Kesisoglou F, Panmai S, Wu Y. Nanosizing – oral formulation development and biopharmaceutical evaluation. Adv Drug Deliv Rev. 2007;59(7):631–644. | ||
Samaha D, Shehayeb R, Kyriacos S. Modeling and comparison of dissolution profiles of diltiazem modified-release formulations. Dissolut Technol. 2009;16:41–46. | ||
Dixit P, Jain DK, Dumbwani J. Standardization of an ex vivo method for determination of intestinal permeability of drugs using everted rat intestine apparatus. J Pharmacol Toxicol Methods. 2012;65(1):13–17. | ||
Bothiraja C, Pawar A, Deshpande G. Ex-vivo absorption study of a nanoparticle based novel drug delivery system of vitamin D3 (Arachitol NanoTM) using everted intestinal sac technique. J Pharm Investig. 2016;46:425–432. | ||
Nicolas P, Tod M, Padoin C, Petitjean O. Clinical pharmacokinetics of diacerein. Clin Pharmacokinet. 1998;35(5):347–359. | ||
Ahmed A, Yadav HK, Lakshmi SV, Namburi BV, Shivakumar HG. Mucoadhesive nanoparticulate system for oral drug delivery: a review. Curr Drug Ther. 2012;7:42–55. | ||
Nijs G, de Witte P, Geboes K, Lemli J. Influence of rhein anthrone and rhein on small intestine transit rate in rats: evidence of prostaglandin mediation. Eur J Pharmacol. 1992;218(2–3):199–203. |
Supplementary material
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.