Back to Journals » Clinical Optometry » Volume 13
CHARGE Syndrome Associated with Ocular Abnormalities: A Case Report with Treatment of Amblyopia and Refractive Correction
Authors Aldakhil S
Received 24 August 2021
Accepted for publication 18 October 2021
Published 25 October 2021 Volume 2021:13 Pages 303—307
DOI https://doi.org/10.2147/OPTO.S335805
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Sulaiman Aldakhil
Department of Optometry, College of Applied Medical Sciences, Qassim University, Buraydah, Saudi Arabia
Correspondence: Sulaiman Aldakhil
Department of Optometry, College of Applied Medical Sciences, Qassim University, P.O. Box 6699, Buraydah, 51452, Saudi Arabia
Tel +966163015501
Email [email protected]
Abstract: CHARGE syndrome is a rare genetic disorder associated with many ocular anomalies including amblyopia, strabismus and high refractive errors. It has been found that the visual acuity of patients with CHARGE syndrome is typically lower than 20/60. After reviewing the literature, there has been a lack of detailed information about the assessments of visual function. Thus, this case report illustrates the strategy plan to treat amblyopia and refractive correction for a young girl with CHARGE syndrome.
Keywords: CHARGE syndrome, amblyopia, visual function, mixed astigmatism, refractive correction
Introduction
CHARGE syndrome (CS) is caused by rare genetic disorder with incidence rate of approximately 1:10,000–15,000 live births.1–3 The term “CHARGE” is an acronym summarizing six clinical features of the syndrome: involving coloboma, heart defects, atresia of the choanae, restriction in growth and/or development, genital anomalies and ear anomalies.4 It has been reported that 70% of patients with CS had a mutation in the CHD7 (chromodomain helicase DNA‑binding protein) gene.5 The visual function is commonly affected, with coloboma representing a major feature and being present in 72% to 95% of patients.6–8 Coloboma is generally chorioretinal, and it may affect the eyelid, iris and optic disc. The macula can also be affected and this would cause substantial reductions in central visual acuity.9 There are other ocular anomalies associated with CS including microcornea, microphthalmos, nystagmus, ptosis, amblyopia, strabismus and high refractive errors.6,10 Studies have found that the mean value of visual acuity (VA) was less than 20/60 in subjects with CS.6,7,9,10 However, there is lack of detailed information in other aspects of visual function due to some difficulties in participation of CS patients.11 Among these studies, there were no assessments of refractive error corrections and/or details about the treatment of amblyopia. Thus, the aim of this case report is to examine in details the visual function of a young girl with CS having bilateral amblyopia and provide her with the refractive correction including a treatment plan of amblyopia.
Case Report
The study was approved by the Ethics Committee in Qassim University and the patient’s parents have given a written informed consent for the publication of the case. The study was carried out according to the tenets of the Helsinki Declaration for the conduct of medical research with human subjects.
A 7-year-old female with CS presented to our pediatric optometry clinic to assess her visual function. She was born premature at 29 weeks and diagnosed with congenital heart defect when she was 3 years old. The patient exhibited hearing loss, restriction in growth (height, 105 cm; weight, 20.5 kg) and a characteristic facial appearance. Her mental age was that of a 5-year-old based on the evaluation of the scientific committee in the ministry of education which is responsible for classifying students with disabilities. The girl complained of gradual decrease in distance vision for both eyes during the last two years. There was no history of wearing glasses and her parents reported that she did not undergo any ocular examination in the past three years.
Clinical Findings
First Visit
In the first visit, the ocular examinations of our patient involved the assessment of anterior segment. The fundus examination by direct ophthalmoscopy revealed a very mild bilateral chorioretinal/optic disc coloboma. Intraocular pressure (IOP) measured 15 mmHg in the right eye and 16 mmHg in the left eye.
The uncorrected visual acuity (VA) was measured using an auto chart projector with the Snellen’s chart at 6 m. The uncorrected VA in her right eye was 20/40, improving to 20/30 with pinhole, whereas the UCVA of the left eye was 20/100, improving to 20/50 with pinhole. The dry and cycloplegic refraction were obtained by the use of both standard retinoscopy and autorefractor (NIDEK AR-310), and three static measurements of refractive error were averaged for each eye. Cyclopentolate 1% was instilled 3 times after 5-min intervals, and then cycloplegic refraction was obtained. The findings showed a high mixed astigmatism in both eyes, and the patient was given an appointment after one week for post mydriatic test (PMT) to examine the subjective refraction acceptance (see Table 1).
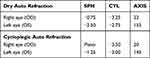 |
Table 1 The Average Measurements of Dry and Cycloplegic Auto Refraction |
The mean corneal curvature, measured using an autorefractor was 7.18 and 7.34 mm, respectively. The binocular vision function was also assessed using a cover–uncover test at both distance (3 m) and near (40 cm). The results of cover test showed alternating esotropia of 15Δ prism diopter at near and 10Δ prism diopter at distance, by using Hirschberg method.
Second Visit
After one week, the patient attended for PMT and subjective refraction was performed to examine the child tolerance of maximum cylindrical power correction. The best subjective refraction was given as shown in Table 2.
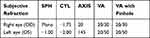 |
Table 2 The Best Subjective Acceptance After Cycloplegic Refraction and VA |
Treatment Plan as a First Intervention Strategy for Treatment of Amblyopia
The visual assessment of child showed a bilateral amblyopia with high mixed astigmatism in both eyes. Thus, a new prescribed spectacles were given to the child and the parents were instructed to ensure a full-time wearing of the glassed accompanied with part-time patching of the right eye (4 to 6 hours per day) for two months period. Although the patient has small ESO deviation, the binocular vision evaluation showed almost good fixation with some limitation in the abduction movement of extraocular muscles.
Third Visit
The patient returned to our clinic after two months and the parents reported that her vision improved with the new prescribed glasses. The parents confirmed that she has been wearing the glasses all the time; however, they were struggling with patching time as the girl refused to complete the assigned hours (only 1 to 2 hours per day). In this visit, re-evaluation of the visual function was obtained including the measurements of refractive error, the corrected VA and the binocular vision function. The dry objective and subjective refraction showed no significant differences compared with the previous visit. The measurements of corrected VA showed one line improvement in both eyes (see Table 3). The assessments of the binocular vision function also revealed no changes in the ESO deviation and the movements of extraocular muscles.
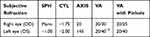 |
Table 3 The Subjective Refection and VA After Two Months of Amblyopia Treatment |
Further appointments are required each 3 months to observe the changes in refraction and evaluate the efficiency of the amblyopia treatment as well as the fundus examination.
Discussion
The ocular abnormalities associated with CS including strabismus and high refractive errors are not well elucidated, as most cases in the literature were not reported with full assessments of amblyopia treatment. However, this rare case report of the CS child provides a detailed evaluation of refractive errors corrections with an appropriate intervention strategy for treating amblyopia.
Our case has a very mild bilateral chorioretinal/optic disc coloboma and the visual functionality was affected due to the involvement of optic disc and retina. The girl also has high astigmatism and ESO deviation and this has led to a significant reduction in distance visual acuity for both eyes. The impact of these ocular abnormalities has impaired her visual function and caused bilateral amblyopia.
The results showed that the child has a difference in the spherical power between the two eyes (more than 1D), with high mixed astigmatism and ESO deviation. Studies have reported that in anisometropic amblyopia, the refractive errors should be corrected first with optical intervention, whereas in strabismic amblyopia the amblyopia needs to be treated initially.12,13 The challenge was in how to prescribe the optimum visual correction without creating visual distortion due to the high astigmatism. Thus, the best subjective refraction acceptance was given to avoid the intolerance of maximum astigmatism power.
In this case, the optimum sphere/cylinder correction was applied to obtain the best corrected visual acuity, while the residual visual deficit was due to amblyopia. Numerous researchers have suggested that refractive correction alone is therapeutic in its own right, by creating a clear foveal image to be received by the retinal signals of the amblyopic eye.14–16 One study also indicated that refractive correction alone improves the VA not only in subjects with anisometropic amblyopia but also in patients with strabismic amblyopia.15
The patching strategy to treat amblyopia is the most popular method that has been used for centuries.17 Randomized clinical trials have shown that 6 hours of patching is a more effective method compared to 1% atropine drop.18,19 Another randomized study has examined 507 amblyopic children aged 7 to 12 years old, with VA ranging from 20/40 to 20/400.20 The results showed that 53% of children improved with patching, optical correction, atropine and near visual activities, while 25% improved with optical correction alone. The findings indicate that the amblyopia treatment is beneficial and effective even for children above the age of 7 years old. Therefore, the treatment plan for this case was to apply 6 to 4 hour patching per day with the best refractive correction. Clearly the data showed that this strategy improved the VA (one line improvement in both eyes) in two months period of time, although the child did not complete the total assigned hours of patching.
The girl has acceptable communication skills and the parents made considerable effort to encourage her to draw and read some words. During the clinical sessions, she was cooperative in visual acuity and subjective refraction tests. However, her general behavior has some issues, as the parents were struggling in convincing her to complete the patching time. It is possible that her visual function could have been improved if she completed the total time of patching, or it could be that only 1 to 2 hours of patching along with the optical correction have achieved the maximum visual improvement.
In humans, many studies have evaluated emmetropization process and the development of refractive errors.21,22 The data have shown a significant reduction in the magnitude of astigmatism and hyperopia over the first few years of life.23 One study examined the visual development in children and reported that emmetropia is achieved at the age of 10 to 12 years old.24 It is well established that uncorrected refractive errors disrupts the normal emmetropization process, and this is thought to be due to the absence of a clear retinal image which is important to send an accurate visual feedback for the development of visual system. Thus, for this CS case, the treatment plan will continue by monitoring the development of the visual system, providing optimum correction of refractive error along with the treatment of amblyopia until she reaches 12 years old.
Conclusion
This rare case demonstrates an appropriate amblyopia treatment for CHARGE syndrome patient. The data showed that part-time patching with refractive correction is an effective treatment in eliminating amblyopia. Eye practitioners should be aware of the other ocular abnormalities associated with CS including high refractive errors, strabismus and amblyopia. Future investigation is needed to examine the long term effect of amblyopia treatment upon a large number of CS patients.
Ethics Approval and Consent to Participate
This research was approved by the human ethics committees of the Qassim University, deanship of scientific research with reference number: 19-07-06, dated 5 March 2020. The patient’s parents have given a written informed consent for the publication of the case details.
Funding
There is no funding to report.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Blake KD, Davenport SLH, Hall BD, et al. CHARGE association: an update and review for the primary pediatrician. Clin Pediatr. 1998;37(3):159–174. doi:10.1177/000992289803700302
2. Janssen N, Bergman JEH, Swertz MA, et al. Mutation update on the CHD7 gene involved in CHARGE syndrome. Hum Mutat. 2012;33(8):1149–1160. doi:10.1002/HUMU.22086
3. Trider C-L, Arra-Robar A, van Ravenswaaij-arts C, Blake K. Developing a CHARGE syndrome checklist: health supervision across the lifespan (from head to toe). Am J Med Genet A. 2017;173(3):684–691. doi:10.1002/AJMG.A.38085
4. Pagon RA, Graham JM, Zonana J, Yong SL. Coloboma, congenital heart disease, and choanal atresia with multiple anomalies: CHARGE association. J Pediatr. 1981;99(2):223–227. doi:10.1016/S0022-3476(81)80454-4
5. Aramaki M, Udaka T, Kosaki R, et al. Phenotypic spectrum of CHARGE syndrome with CHD7 mutations. J Pediatr. 2006;148(3):410–414. doi:10.1016/J.JPEDS.2005.10.044
6. Russell-Eggitt IM, Blake KD, Taylor DS, Wyse RK. The eye in the CHARGE association. Br J Ophthalmol. 1990;74(7):421–426. doi:10.1136/BJO.74.7.421
7. Strömland K, Sjögreen L, Johansson M, et al. CHARGE association in Sweden: malformations and functional deficits. Am J Med Genet A. 2005;133A(3):331–339. doi:10.1002/AJMG.A.30563
8. Legendre M, Abadie V, Attié-Bitach T, et al. Phenotype and genotype analysis of a French cohort of 119 patients with CHARGE syndrome. Am J Med Genet C Semin Med Genet. 2017;175(4):417–430. doi:10.1002/AJMG.C.31591
9. McMain K, Robitaille J, Smith I, et al. Ocular features of CHARGE syndrome. J Am Assoc Pediatr Ophthalmol Strabismus. 2008;12(5):460–465. doi:10.1016/J.JAAPOS.2008.02.009
10. Nishina S, Kosaki R, Yagihashi T, et al. Ophthalmic features of CHARGE syndrome with CHD7 mutations. Am J Med Genet A. 2012;158A(3):514–518. doi:10.1002/AJMG.A.34400
11. Onesimo R, Ricci D, Agazzi C, et al. Visual function and ophthalmological findings in CHARGE syndrome: revision of literature, definition of a new clinical spectrum and genotype phenotype correlation. Genes. 2021;12(7):972. doi:10.3390/GENES12070972
12. Lam GC, Repka MX, Guyton DL. Timing of amblyopia therapy relative to strabismus surgery. Ophthalmology. 1993;100(12):1751–1756. doi:10.1016/S0161-6420(13)31403-1
13. Holmes JM, Clarke MP. Amblyopia. Lancet. 2006;367(9519):1343–1351. doi:10.1016/S0140-6736(06)68581-4
14. Moseley MJ, Neufeld M, McCarry B, et al. Remediation of refractive amblyopia by optical correction alone. Ophthalmic Physiol Opt. 2002;22(4):296–299. doi:10.1046/J.1475-1313.2002.00034.X
15. Stewart CE, Moseley MJ, Fielder AR, Stephens DA. Refractive adaptation in amblyopia: quantification of effect and implications for practice. Br J Ophthalmol. 2004;88(12):1552–1556. doi:10.1136/BJO.2004.044214
16. Clarke MP, Wright CM, Hrisos S, Anderson JD, Henderson J, Richardson SR. Randomised controlled trial of treatment of unilateral visual impairment detected at preschool vision screening. BMJ. 2003;327(7426):1251. doi:10.1136/BMJ.327.7426.1251
17. Loudon SE, Simonsz HJ. The history of the treatment of amblyopia. Strabismus. 2009;13(2):93–106. doi:10.1080/09273970590949818
18. Group TPEDI. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120(3):268–278. doi:10.1001/ARCHOPHT.120.3.268
19. Group* TPEDI. Two-year follow-up of a 6-month randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2005;123(2):149–157. doi:10.1001/ARCHOPHT.123.2.149
20. Scheiman MM, Hertle RW, Beck RW, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123(4):437–447. doi:10.1001/ARCHOPHT.123.4.437
21. Cook RC, Glasscock RE. Refractive and ocular findings in the newborn. Am J Ophthalmol. 1951;34(10):1407–1413. doi:10.1016/0002-9394(51)90481-3
22. Goldschmidt E. Refraction in the newborn. Acta Ophthalmol. 1969;47(3):570–578. doi:10.1111/J.1755-3768.1969.TB08143.X
23. Atkinson J, Braddick O, French J. Infant astigmatism: its disappearance with age. Vision Res. 1980;20(11):891–893. doi:10.1016/0042-6989(80)90070-X
24. Saunders KJ. Early refractive development in humans. Surv Ophthalmol. 1995;40(3):207–216. doi:10.1016/S0039-6257(95)80027-1
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
