Back to Journals » Infection and Drug Resistance » Volume 12
Changing antibiotic susceptibility pattern in uropathogenic Escherichia coli over a period of 5 years in a tertiary care center
Authors Prasada S, Bhat A , Bhat S , Shenoy Mulki S , Tulasidas S
Received 16 January 2019
Accepted for publication 16 April 2019
Published 29 May 2019 Volume 2019:12 Pages 1439—1443
DOI https://doi.org/10.2147/IDR.S201849
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Shobha Prasada,1,2 Archana Bhat,1,2 Sevitha Bhat,1,2 Shalini Shenoy Mulki,1,2 Sanyuktha Tulasidas1,2
1Department of Microbiology, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India; 2Manipal McGill Center for Infectious Diseases, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal, Karnataka, India
Objective: To assess the changing antibiotic sensitivity pattern in Uropathogenic E. coli over a period of time (2013–2017) with a special emphasis on ESBL-producing E. coli.
Methods: This retrospective study was carried out in the Department of Microbiology, Kasturba Medical College, Ambedkar Circle, Mangalore. A retrospective time bound analysis of 500 samples/year was performed. The urine samples received from the suspected cases of urinary tract infection (UTI) were processed. Wet mount examinations of urine samples were done. The urine culture was done by a semi-quantitative method on Mac Conkey’s agar, Cysteine Lactose Electrolyte Deficient (CLED) medium, and UTI Chrome agar. Culture plates were incubated for 18–24 hours at 37°C. Urine samples with a colony count of ≥105, CFU/ml were considered significant. The uropathogens were identified by their biochemical reactions. The antibiotic susceptibility testing (AST) was carried out using a Vitek Compact 2 system and Modified Kirby Bauer disc diffusion method.
Results: Antibiotic resistance of Uropathogenic E.coli to cephalosporins increased from 51 to 58%, Cotrimoxazole: 52 to 59%, Piperacillin tazobactam 9.4 to 23%, Carbapenems 0 to 5.9%. Antibiotic resistance to netilmicin has reduced from 8 to 6.5%, and norfloxacin 59 to 48%. The rates of ESBL production have increased from 45.2 to 59.6% in the 5 years.
Conclusion: The increasing antibiotic resistance trends in UTI patients indicate that it is vitally important to use them conservatively. Proper guidelines, management of antibiotic usage, and constant information to the clinicians regarding the sensitivity pattern can help to prevent drug resistance.
Keywords: uropathogenic E.coli, antibiotic resistance, UTI, trends
Introduction
Urinary tract infections (UTIs) are currently placed among the most widespread infectious diseases worldwide, with chronic and recurrent infections being troublesome.1 Uropathogenic Escherichia coli (E. coli) (UPEC) are the primary etiologic agents, and the most common cause of urinary tract infections (UTIs) worldwide.1,2 Infections are gradually becoming hard to treat, and may lead to therapeutic dead ends.3
The treatment regimen of UTIs differs according to the age of the patient, sex, underlying disease, infecting agent, and whether there is lower or upper urinary tract involvement.4
Escherichia coli express multi-drug resistance. In the treatment of Uncomplicated cystitis, the preferable antibiotics for empiric treatment include Nitrofurantoin, Trimethoprim/sulphamethoxazole, or Ciprofloxacin. The alternate choices include Cefuroxime and Cefixime. For complicated and upper UTI cases in hospitalized patients, the antibiotics used are Piperacillin tazobactam and Carbapenems.4
The antibiotic resistance patterns have shown large inter-regional differentiation. The appropriate choice of antibiotic needs to be tailored based on the local susceptibility pattern.
Usually empirical antimicrobial treatment is initiated in almost all the cases of UTI before the laboratory results of urine culture are obtained and, thus, antibiotic resistance might increase in uropathogens due to repeated inappropriate antibiotic choice. This study will help us to assess the changing antibiotic sensitivity pattern in the E. coli over a period of time (2013–2017), with a special emphasis on ESBL producing E. coli.
Materials and methods
Study setting
The retrospective study was conducted in Kasturba Medical College Hospital, Mangalore, a tertiary care hospital. This is a 1,000 bedded hospital that provides healthcare and other specialist services including exclusive cardiothoracic, respiratory, and urology units. The hospital includes an emergency department and intensive care unit, and offers a wide range of inpatient and outpatient services. The Microbiology laboratory receives around 10,000 urine samples/year from inpatients and outpatients.
Study sample
Inclusion criteria
- Urine samples sent for culture from patients presenting with at least three of the following symptoms: dysuria, urgency, frequency, or suprapubic tenderness.
- Urine samples with significant growth of E. coli (>105 CFU/ml) in the months of March–May. In the first year, 2013, we received 500 urine samples with significant growth of E. coli in the peak summer months . Hence, we continued to analyse 500 samples during the same period subsequently for the next 4 years, to maintain uniformity.
Exclusion criteria
Urine samples with negative culture, no significant growth, or growth other than E. coli.
Sample processing
Wet mount examination of uncentrifuged urine was performed. Urine culture was done by a semi-quantitative method on Mac Conkey’s agar, CLED medium, and UTI Chrom agar. Culture plates were incubated for 18–24 hours at 37°C. The uropathogens were identified by standard biochemical reactions. The urine specimen with a growth of ≥105 CFU/mL of a single microorganism or mixed flora with a predominant species was considered significant and defined as positive urine culture. Negative urine culture was defined as no growth, insufficient growth, or a mixed microbial flora with no predominant organism.5
The uropathogens were identified by the standard biochemical reactions
The antibiotic susceptibility testing (AST) was carried out using the Vitek Compact 2 system and Modified Kirby Bauer disc diffusion method. The antibiotic discs (Himedia) used for coliforms included Ampicillin (10 µg), Amoxicillin/Clavulanic Acid (30 µg), Cefuroxime (30 µg), Ceftriaxone (30 µg), Cefepime (30 µg), Cefoperazone/Sulbactam (75/30 µg), Amikacin (30 µg), Gentamicin (10 µg), Ciprofloxacin (5 µg), Imipenem (10 µg), Meropenem (10 µg), and Piperacillin/Tazobactam (100/10 µg). The interpretation of results was based on the recommendations of the Clinical Laboratory Standards Institute (CLSI). ESBL production in E. coli will be detected by the screening and confirmatory tests recommended by CLSI guidelines.6
The study obtained clearance from the Institutional Ethics committee. IEC KMC MLR 01–17/05.
Results
The antibiotic resistance rates to the first line antimicrobials to treat UTI in our setup were Nitrofurantoin: 13.3%, cotrimoxazole: 0.6%, norfloxacin: 48%. The resistance rates to the second line drugs were Piperacillin tazobactam: 23%, Carbapenems: 5.9%. The trend of antibiotic resistance over the period of 5 years was analyzed using the chi-square test and Cochrane Armitage test. A statistically significant trend in the rates of antibiotic resistance over the period of 5 years was seen for the following antibiotics: Norfloxacin, Ciprofloxacin, Piperaciilin and Tazobactam (p>0.001).
The analysis of the trend is depicted in Table 1 (chi-square test) and Figure 1 (Cochrane Armitage test).
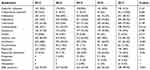 | Table 1 Trend of antibiotic resistance in E. coli isolates |
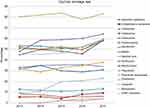 | Figure 1 The 5-year trend of antibiotic susceptibility to uropathogenic E. coli. |
Discussion
A recurrent unreasonable use of antibiotics changes the intestinal flora, leading to bacterial resistance. The extensiveness of antibiotic resistance is a serious public health concern.
In this study, we focused on the uropathogenic E. coli strains and their sensitivity patterns to different groups of antibiotics commonly administered to treat the infections over the period of 5 years.
Resistance to TMP-SXT has increased over the period of time (2013–2017). TMP-SXT has been the first-line empirical treatment for more than 30 years. It is the antibiotic prescribed routinely for uncomplicated UTIs in many developed and developing countries. Increasing resistance to TMP-SXT is a matter of concern. The TMP-SXT resistance rate in 2013 in the present study was 52%, increasing up to 59.6% in 2017. The rise in resistance rate is not statistically significant for this drug. This phenomenon could be due to restricted use of this antibiotic in our setup, owing to its associated side-effects. A study conducted by Nalini et al7 in 2013 in, Tamil Nadu, India, identified an increasing trend in trimethoprim resistance up to 68.69%.
In settings with a >10–20% resistance to cotrimoxazole, the alternative regimen could be fluoroquinolone, nitrofurantoin, or fosfomycin. The data from the present study reveals the high rate of fluoroquinolone resistance in E. coli (>60%). The rise in resistance to Norfloxacin was statistically significant in the 5 years. The fact can be explained as it is one of the commonly prescribed drugs on an outpatient basis. It is of great concern that E. coli has developed a high rate of resistance against them as well, which is in line with other studies.8,9 It reflects that this useful antibiotic is instantaneously losing its efficacy in the treatment of UTI.
Nitrofurantoin resistance is comparatively lower in our study (12.8–13.3%). The lower resistance to nitrofurantoin may be attributed to the sparse use of this drug in the treatment of uncomplicated lower urinary tract infections in outpatients. The findings are in par with the study quoting a resistance rate of 13%.10
In our tertiary care center, cephalosporins are the drug of choice in the treatment of complicated UTI in hospitalized patients. Unfortunately, the increasing use of third generation cephalosporins has contributed to high level resistance amounting up to 58%. Cephalosporins need to definitely be used with caution as an empiric choice in hospitalized patients owing to the high resistance rates. A similar study from North-East India by Mukherjee et al11 reported a considerable rate of resistance to Cefotaxime (67.5%), Ceftriaxone (62.5%), Ceftazidime (55%), and 45% of the uropathogenic E. coli were ESBL producers. Our study showed a statistically significant rise in ESBL prevalence, ie, from 45.2% to 59.6% over a period of 5 years. A varying rate of prevalence (19–60%) of ESBL producing gram-negative bacteria has been reported from different studies across India.12 The increasing levels of ESBLs may be attributed to the increased empirical administration of third generation cephalosporins. This reduces the clinical utility of cephalosporins. In order to preserve these effective antimicrobials, physicians must rely on routine urine culture and sensitivity tests, and treat the patients accordingly. ESBL producers are usually known to be multidrug resistant organisms (MDR).
Aminoglycoside resistance also depicted an increase over the last few years. Gentamicin is used as an antibiotic prophylaxis of choice for invasive urological procedures in many countries. Of the isolates, 16.25% showed resistance to gentamicin in the previous studies.13 In our study the aminoglycoside resistance rate was 34%. The use of aminoglycosides has decreased in the last few years.
In the present study, we observed a change in the resistance pattern to Carbapenems, which is used as the last choice for the management of multidrug-resistant E. coli. These results were similar to the study conducted by Ramalingam Sekar et al 201614 Cefaperazone/sulbactum, piperacillin/tazobactum, and nitrofurantoin showed good sensitivity rates.
Conclusion
Urinary tract infection is one of the most frequent conditions in medical practice affecting people of all ages. The high rates of antibiotic resistance among the UPEC has left the clinicians with fewer options for choosing the proper antibiotics for the treatment of UTI caused by these multi-drug resistant organisms. The worrisome fact of emergence of ESBL producing organisms necessitates the clinical microbiology laboratories to detect ESBL production. Judicious use of antibiotics and proper implementation of Antibiotic policy in hospitals is the need of the hour. The study highlights the need for restricted use of quinolones and third generation cephalosporins in our setup. This will help, to a certain extent, in preventing the emergence and spread of antibiotic resistance among the Gram negative bacilli. Carbapenem resistance is an issue of concern. Proper guidelines, management of antibiotic usage, and constant information to the clinicians regarding the sensitivity pattern can help to prevent drug resistance.
Acknowledgments
The authors are grateful to Manipal Academy of Higher Education for all the support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Matthew GB, Matthew AM. Persistence of uropathogenic Escherichia coli in the face of multiple antibiotics. Antimicrob Agents Chemother. 2010;54(5):1855–1863. doi:10.1128/AAC.00014-10
2. Ihsan A, Zara R, Safia A, Sajid M, Javid ID. Prevalence of multi-drug resistant uropathogenic Escherichia coli in Potohar region of Pakistan. Asian Pac J Trop Biomed. 2016;6(1):60–66. doi:10.1016/j.apjtb.2015.09.022
3. Moroh JLA, Fleury Y, Tia H, et al. Diversity and antibiotic resistance of uropathogenic bacteria from Abidjan. Afr J Urol. 2014;20:18–24. doi:10.1016/j.afju.2013.11.005
4. Jharna M, Srinivas AN, Buddhapriya D, Subhash CP. Antibiotic resistance pattern among common bacterial uropathogens with a special reference to ciprofloxacin resistant Escherichia coli. Indian J Med Res. 2012;136:842–849.
5. Cheesebrough M
6.
7. Nalini R, Ramya JE, Meenaksh B, et al. Recent sensitivity pattern of Escherichia Coli in urinary tract infection. Rrjmb. 2014;3(3):31–35.
8. Neetu S, Anita G, Geeta W, Rupinder B. Pattern of antimicrobial resistance of Escherichia coli isolates from urinary tract infection patients: a three year retrospective study. JAPS. 2016;6(1):62–65.
9. Waseem A, Fareeda J, Wajeeha A. Frequency of Escherichia Coli in patients with community acquired urinary tract infection and their resistance pattern against some commonly used antibacterials. JAMC. 2015;27(2):333–337.
10. Shakya P, Shrestha D, Maharjan E, Sharma VK, Paudyal R, Production Among ESBL. E. coli and Klebsiella spp. Causing urinary tract infection: a hospital based study. Open Microbiol J. 2017;11:23–30. doi:10.2174/1874285801711010023
11. Mukherjee M, Basu S, Mukherjee SK, Majumder M. Multidrug-resistance and extended spectrum beta-lactamase production in uropathogenic E. Coli which were isolated from hospitalized patients in Kolkata, India. J Clin Diagno Res. 2017;7(3):449–453.
12. Narayan P, Pooja M, Hridaya P, Govardhan J. High rates of multidrug resistance among uropathogenic Escherichia coli in children and analyses of ESBL producers from Nepal. Antimicrob Resist Infect Control. 2017;6(9):3–7. doi:10.1186/s13756-016-0165-9
13. Gordon KA, Jones RN. Susceptibility patterns of orally administered antimicrobials among urinary tract infection pathogens from hospitalized patients in North America: comparison report to Europe and LatinAmerica: results from the SENTRY antimicrobial surveillance program. Diagn Microbiol Infect Dis. 2000;45:295–301. doi:10.1016/S0732-8893(02)00467-4
14. Mahtab H, Yalda M, Hamid H, Hadi SE. Antimicrobial resistance pattern in Escherichia coli isolates obtained from a specialized women and children hospital in Shiraz, Iran: a prevalence study. J Health Sci Surveillance Sys. 2016;4(4):194–197.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
