Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Categorical improvements in disease severity in patients with major depressive disorder treated with vilazodone: post hoc analysis of four randomized, placebo-controlled trials
Authors Durgam S, Chen C, Gommoll CP, Edwards J, Citrome L
Received 19 July 2016
Accepted for publication 14 September 2016
Published 2 December 2016 Volume 2016:12 Pages 3073—3081
DOI https://doi.org/10.2147/NDT.S117581
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Video abstract presented by Durgam et al.
Views: 1916
Suresh Durgam,1 Changzheng Chen,1 Carl P Gommoll,1 John Edwards,1 Leslie Citrome2
1Allergan, Jersey City, NJ, USA; 2Department of Psychiatry and Behavioral Sciences, New York Medical College, Valhalla, NY, USA
Background: In three 8-week studies of vilazodone 40 mg/d (NCT00285376, NCT00683592, and NCT01473394) and a 10-week study of vilazodone 20 or 40 mg/d (NCT01473381), adults with major depressive disorder (MDD) showed significantly greater improvement with vilazodone versus placebo in global disease severity as measured by mean change from baseline in Clinical Global Impression of Severity (CGI-S) score. To assess the proportion of patients achieving clinically meaningful improvement, a post hoc pooled analysis was conducted using categorical shifts in disease severity based on CGI-S scores at baseline and end of treatment (EOT).
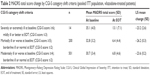
Methods: Analyses were conducted in the pooled intent-to-treat population (N=2,218). Definitions of categorical shifts included CGI-S ≥4 (moderately ill or worse) at baseline to CGI-S ≤2 (normal or borderline ill) at EOT; CGI-S ≥5 (markedly ill or worse) at baseline to CGI-S ≤2 at EOT; and CGI-S ≥6 (severely ill or worse) at baseline to CGI-S ≤3 (mildly ill or better) at EOT.
Results: At baseline, 2,217 patients were moderately ill or worse. The percentage who improved to normal or borderline ill was significantly higher with vilazodone than with placebo (40.0% versus 27.8%; odds ratio [OR] =1.7, P<0.001; number needed to treat [NNT] =9). In the 979 patients who were markedly ill or worse at baseline, the percentage who improved to normal or borderline ill was significantly higher with vilazodone than with placebo (36.8% versus 25.5%; OR =1.7, P<0.001; NNT =9). The small number of severely ill patients at baseline (n =43) provided inadequate power to detect statistically significant between-group differences, but an NNT =5 was found for improvement to mildly ill or better.
Conclusion: Categorical shift analyses, defined using baseline and EOT CGI-S scores, showed that significantly higher proportions of patients had clinically meaningful improvements in global disease severity with vilazodone 20–40 mg/d versus placebo. This type of analysis may be useful for evaluating the effects of antidepressant treatment in adults with MDD.
Keywords: depression, antidepressant, global improvement, clinical trial
Introduction
In clinical trials of major depressive disorder (MDD), the primary efficacy end point is usually defined by a mean score change in a validated depression scale such as the Montgomery–Åsberg Depression Rating Scale (MADRS)1 or Hamilton Depression Rating Scale (HAMD).2 Statistical superiority compared to placebo indicates efficacy in these trials, but it can be difficult to interpret the clinical meaningfulness of between-group differences in MADRS or HAMD score changes. For example, a mean improvement can be due to large changes in a few patients or moderate changes in many patients. Moreover, analyses of mean score changes do not always account for baseline symptom severity. Depending on the treatment, patients with worse baseline scores may have larger or smaller score improvements than patients with less severe baseline scores.
The MADRS and HAMD are often used in clinical trials because they comprise multiple items that are related to core depression symptoms and because the scales are sensitive for detecting antidepressant treatment effects.3 In clinical settings, however, it may be cumbersome to administer a multi-item instrument such as the MADRS or the HAMD at every patient visit to ascertain antidepressant effects. In this respect, a single-item measure such as the Clinical Global Impression of Severity (CGI-S)4 may have more utility for practicing clinicians. As an instrument that has demonstrated sensitivity for detecting antidepressant effects in addition to being correlated with both the MADRS and the HAMD,3,4 the CGI-S has been included in many MDD clinical trials as a secondary or additional efficacy end point. Scoring for the CGI-S (range, 1 “normal” to 7 “extremely ill”) offers a face-valid simplicity that may be useful in clinical practice. However, when presented as mean change from baseline, interpretation of CGI-S results in clinical trial reports may remain challenging. For example, an analysis of CGI-S score mean change from baseline could result in a between-group difference of <1 point with a P-value <0.05. This result would indicate statistical superiority of an active drug over placebo, but it would be difficult to ascertain whether the magnitude of treatment effect was meaningful in day-to-day clinical practice.
To explore whether CGI-S data can be analyzed in a more clinically meaningful way by using shifts from higher to lower degrees of severity, data were pooled from 4 clinical trials of vilazodone,5–8 a serotonin reuptake inhibitor and 5-HT1A receptor partial agonist that is approved in the United States for the treatment of MDD in adults. Taking into account both baseline and end point CGI-S scores, several different categorical shifts were defined to identify the percentage of patients who met specific thresholds for global improvements. In addition to providing further information regarding response to vilazodone in clinical trials in adult patients with MDD, this analytic approach may offer clinicians a practical method for evaluating antidepressant efficacy in clinical settings.
Methods
Studies
Data were pooled from 4 randomized, double-blind, placebo-controlled Phase 3 clinical trials. Methods for all of these studies have been previously reported.5–8 All studies were approved by the Institutional Review Board of each participating study site (Table S1), and all patients provided informed and written consent prior to study entry. In 3 studies (NCT00285376,5 NCT00683592,6 and NCT014733947), patients were randomized (1:1) to 8 weeks of double-blind treatment with placebo or vilazodone 40 mg/d. In 1 study (NCT014733818), patients were randomized (1:1:1) to 10 weeks of double-blind treatment with placebo, vilazodone 20 mg/d, or vilazodone 40 mg/d. All 4 studies included adult patients, ≥18 years of age, who met the Diagnostic and Statistical Manual of Mental Disorders, fourth edition-text revision (DSM-IV-TR) criteria for MDD.9
Patients were required to have a current major depressive episode (duration of ≥4 weeks to <2 years5,6 or ≥8 weeks to ≤12 months7,8); 17-item HAMD total score ≥22 and item 1 (depressed mood) score ≥2;5,6 and/or MADRS total score ≥26.7,8 CGI-S score was not used to determine eligibility in any of the studies. Key exclusion criteria included primary DSM-IV-TR Axis I disorder other than MDD; history of bipolar or psychotic disorders; history of nonresponse to ≥2 antidepressants after adequate treatment; and risk of suicide based on investigator judgment and/or formal assessment (eg, Columbia-Suicide Severity Rating Scale score; MADRS item 10 [suicidal thoughts] score ≥5).
In all the studies, the primary efficacy end point was defined as MADRS total score change from baseline to end of treatment (EOT). All studies also included CGI-S score change from baseline to EOT as a secondary or an additional end point.
Post hoc analyses
The objective of the current post hoc analyses was to provide a clinically meaningful approach for assessing the global effects of vilazodone versus placebo in adults with MDD. These analyses were conducted in the pooled intent-to-treat (ITT) population, defined as all patients who received ≥1 dose of double-blind study drug and had an available MADRS total score at baseline and at ≥1 post-baseline study visit. Patients were classified into 3 subgroups based on the distribution of CGI-S scores at baseline: severely or extremely ill (score ≥6), markedly ill (score =5), and moderately ill (score =4).
The distribution of CGI-S scores at baseline and EOT was assessed to ascertain the percentage of patients who had worsening, no change, or improvement in overall disease severity. In all the post hoc analyses, EOT was defined as the last available assessment in the double-blind period. No inferential statistics were conducted for the distribution of CGI-S scores, either at baseline or at EOT.
Three sets of CGI-S category shift criteria were also defined post hoc to evaluate the percentage of patients who had clinically meaningful improvements in overall disease severity. These criteria were as follows: 1) CGI-S score ≥6 (severely or extremely ill) at baseline, score ≤3 at EOT (mildly ill or better); 2) CGI-S score ≥5 at baseline (markedly ill or worse), score ≤2 at EOT (borderline ill or normal); and 3) CGI-S score ≥4 at baseline (moderately ill or worse), score ≤2 at EOT (borderline ill or normal). Relative effect sizes for vilazodone versus placebo were calculated using odds ratios (ORs), P-values, and 95% confidence intervals (CIs) that were based on a logistic regression model that included study, treatment group, and baseline CGI-S score as explanatory variables; patient status for meeting the shift criteria was defined as the dependent variable. P-values were not adjusted for multiple comparisons as the analyses were considered exploratory in nature. Absolute effect sizes for the CGI-S category shifts were calculated using numbers needed to treat (NNTs) and 95% CIs, with NNT =1/(rate difference), rounded up to the next whole number.
For descriptive purposes, the least squares mean change from baseline to EOT in MADRS total score was determined in vilazodone-treated patients who met the CGI-S category shift criteria using a mixed model with study and treatment group as fixed effects and baseline MADRS total score as a covariate.
Results
Patients
The pooled ITT population included 2,218 patients (placebo, n=964; vilazodone, n=1,254). One patient was borderline ill at baseline (CGI-S score of 2). The remaining 2,217 patients were moderately ill (CGI-S =4, n=1,238 [55.8%]), markedly ill (CGI-S =5, n=936 [42.2%]), or severely ill (CGI-S =6, n=43 [1.9%]) at baseline. No patient had a CGI-S score of 1 (normal), 3 (mildly ill), or 7 (extremely ill) at baseline.
Within the 2 larger subgroups of patients categorized by global severity (CGI-S =4 or 5), demographics and baseline characteristics were generally similar between treatment groups (Table 1). Across all 3 CGI-S severity subgroups, a higher CGI-S score was not clearly associated with longer MDD duration or current episode duration. However, recurrent episodes were more common in the severely ill subgroup (83.7%) than in markedly ill (73.3%) or moderately ill (74.8%) subgroups. No statistical analyses were conducted to test for differences between treatment groups or between CGI-S severity subgroups.
CGI-S score improvement
In the individual studies, a significantly greater mean improvement in CGI-S score was found with vilazodone versus placebo (Figure 1). A post hoc analysis of data pooled from the 4 individual studies showed that for each of the CGI-S subgroups (severely ill, markedly ill, and moderately ill at baseline), the percentage of patients with CGI-S score improvement was higher with vilazodone than with placebo (Figure 2); no statistical testing between treatment groups was conducted for this analysis. Very few patients receiving either placebo or vilazodone had worsening in CGI-S score.
  | Figure 1 Mean CGI-S score improvements in vilazodone MDD studies. |
Clinically meaningful categorical improvements
In the CGI-S category shift analyses, the percentage of patients who had clinically meaningful improvements in disease severity was higher with vilazodone than with placebo (Figure 3).
The largest magnitude of effect was seen in patients shifted from a score ≥6 at baseline (severely ill or worse) to a score ≤3 (mildly ill or better) at EOT: OR (95% CI) =3.3 (0.7, 16.5); NNT (95% CI) =5 (2 to ∞, −19 to −∞). The difference between treatment groups was not statistically significant, probably due to the small sample size (n=43).
A statistically significant difference between vilazodone and placebo (P<0.001) was observed in patients who shifted from a CGI-S score ≥5 at baseline (markedly ill or worse) to a score ≤2 at EOT (borderline ill or normal): OR (95% CI) =1.7 (1.3, 2.3); NNT (95% CI) =9 (6, 19). Results were also statistically significant for vilazodone versus placebo (P<0.001) in patients who shifted from a CGI-S score ≥4 at baseline (moderately ill or worse) to a score ≤2 at EOT (borderline ill or normal): OR (95% CI) =1.7 (1.4, 2.1); NNT (95% CI) =9 (7, 13). The 3 groups of vilazodone-treated patients who met CGI-S category shift criteria had comparable mean changes from baseline in MADRS total score (Table 2).
Discussion
The efficacy of vilazodone in adults with MDD was established in 4 randomized, double-blind, placebo-controlled trials based on mean changes from baseline in MADRS total score and CGI-S score. Since it can be difficult to apply these types of results to clinical practice, post hoc shift analyses of CGI-S data from the vilazodone studies were conducted.
The single-item CGI-S was selected as the focus of these analyses because of its potential utility in clinical settings. Regular administration of the CGI-S at study visits could help clinicians assess whether patients are improving during acute treatment, and if necessary, whether they are maintaining stability during long-term treatment. The duration of the vilazodone trials (8 or 10 weeks) was not adequate to draw conclusions about the long-term effects of this medication in MDD patients, but analysis of the pooled data indicates that more patients had CGI-S score improvements with vilazodone than with placebo. For example, in patients who were markedly ill at baseline, the percentage experiencing any improvement in CGI-S score was higher with vilazodone (75.1% [386/514]) than with placebo (62.1% [262/422]).
These results were supported by specific CGI-S category shift analyses, which were designed to reflect clinically meaningful improvements, provide relative and absolute treatment effects (ORs and NNTs), and be tested for statistical significance between treatment groups. All patients in the pooled ITT population (except for 1 patient randomized to vilazodone) were moderately ill or worse at baseline (CGI-S score ≥4). In these 2,217 patients, the odds of shifting to borderline ill or normal at EOT (CGI-S score ≤2) was 1.7 times greater with vilazodone than with placebo (P<0.001). The NNT for this CGI-S category shift was 9, which meets the conventional threshold (NNT <10) for clinically relevant results.10 Thus, for every 9 moderately or severely ill patients randomized to vilazodone versus placebo, 1 additional patient can be expected to achieve normal or near-normal global status by the EOT. Similar effect sizes and statistical significance (OR =1.7, NNT =9, P<0.001) were found for the CGI-S category shift analysis that was based on the 979 patients who were markedly ill or worse at baseline (CGI-S score ≥5).
The results from these 2 shift analyses suggest that with acute vilazodone treatment, ~35%–40% of moderately or markedly ill patients may expect a ≥3-point improvement in CGI-S score, which in our data set corresponded to an ~25-point improvement in MADRS total score. These results were consistent with a published analysis of data from other antidepressant clinical trials, which showed positive and significant correlations between CGI-S and MADRS scores over the course of acute treatment.11 A more complex analysis of the vilazodone trial data, such as a regression model with estimation of fit, would be needed to draw any definitive conclusions about the correlation between CGI-S and MADRS improvements in the vilazodone studies. However, the exploratory analysis that was conducted for this report suggests that in clinical settings, a CGI-S score improvement of ≥3 points could be used as an indicator of good treatment response in moderately or markedly ill patients, with a smaller CGI-S score improvement possibly indicating a need for treatment adjustment. Of course, any change to therapy (eg, longer treatment, dose increase, augmentation, or switch) would require careful consideration of the individual patient’s specific medical history and current situation.
Only 43 patients in the pooled study population were categorized as severely ill at baseline (CGI-S =6). This group had the largest treatment effects (OR =3.3, NNT =5), as well as ~25-point decrease in MADRS total score with vilazodone, but lacked power to show a statistically significant difference between vilazodone and placebo for the shift analysis. Thus, it appears that patients with more severe symptoms of MDD might benefit from treatment with vilazodone, but the data in this group are limited in our analysis.
It should be noted that there are no universally established scoring guidelines for the 7 anchor points of the CGI-S.12 Rather, the instrument was designed to be scored based on the professional judgment of individual clinicians. The post hoc analyses presented in this report were adjusted for study site to help mitigate any potential inter-rater variability in CGI-S scoring. From a research perspective, a more structured approach to the CGI-S may be warranted in future MDD clinical trials.12,13 Within a clinical setting, however, inter-rater variability is much less likely to have a confounding effect on evaluating whether a patient is experiencing categorical improvements in overall disease severity.
Limitations
Due to the inclusion criteria of the vilazodone studies, a limitation of these post hoc analyses is the possible skewing of baseline CGI-S scores toward categories that are more severe than may be found in a general population of MDD patients. However, as indicated by a retrospective analysis of observational studies in which >75% of MDD outpatients were found to be moderately to severely ill prior to treatment,14 it seems likely that a majority of patients in clinical settings would also be moderately ill or worse prior to treatment. Nonetheless, the generalizability of baseline CGI-S scores (and corresponding severity categories) found in the current post hoc analyses may be limited.
Other limitations, as mentioned earlier, are as follows: the criteria for CGI-S category shifts were based on the face validity of the CGI-S scale, but these criteria have not been formally validated in MDD patients; the number of patients who were “severely ill” at baseline was not large enough to draw conclusions in this group; and the study duration (8 or 10 weeks) does not provide any information about the long-term effects of vilazodone on overall disease severity.
Conclusion
Post hoc analyses of CGI-S data from 4 randomized, double-blind, placebo-controlled trials indicate that overall disease severity improved in adults with MDD who received acute treatment with vilazodone 20–40 mg/d. Results from the CGI-S category shift analyses demonstrated that in moderately to markedly ill patients, the odds of improving to borderline ill or better was significantly greater with vilazodone than with placebo. These category shifts based on changes in CGI-S scores may provide a useful way to identify clinically meaningful improvements in adults with MDD.
Acknowledgment
Writing and editorial assistance was provided by Mildred Bahn at Prescott Medical Communications Group (Chicago, IL, USA), with support from Allergan.
Disclosure
S Durgam, C Chen, C Gommoll, and J Edwards are full-time employees of Allergan, which sponsored the studies and analyses that are presented in this report. L Citrome has engaged in collaborative research with or received consulting or speaking fees from Acadia Pharmaceuticals, Alexza Pharmaceuticals, Alkermes plc, Allergan (Actavis plc, Forest Laboratories, Inc.), AstraZeneca, Avanir Pharmaceuticals, Inc., Boehringer Ingelheim, Bristol-Myers Squibb, Eli Lilly and Company, Forum Pharmaceuticals Inc., Genentech (member of the Roche Group), Intra-Cellular Therapies, Inc., Janssen Pharmaceuticals, Inc., Jazz Pharmaceuticals, H. Lundbeck A/S, Medivation, Inc, Merck & Co., Inc., Mylan N.V., Novartis AG, Noven Pharmaceuticals, Inc., Otsuka Pharmaceutical, Pfizer Inc., Reckitt Benckiser Group plc, Reviva Inc, Shire, Sunovion Pharmaceuticals Inc., Takeda Pharmaceutical Company Limited, Teva Pharmaceutical Industries Ltd, Valeant Pharmaceuticals International, Inc., and Vanda Pharmaceuticals Inc. The authors report no other conflicts of interest in this work.
References
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. | ||
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. | ||
Khan A, Khan SR, Shankles EB, Polissar NL. Relative sensitivity of the Montgomery-Asberg Depression Rating Scale, the Hamilton Depression rating scale and the Clinical Global Impressions rating scale in antidepressant clinical trials. Int Clin Psychopharmacol. 2002;17(6):281–285. | ||
Guy W. The Clinician Global Severity and Impression Scales. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: National Institute of Mental Health; 1976:218–222. DHEW Publication No. 76–338. | ||
Rickels K, Athanasiou M, Robinson DS, Gibertini M, Whalen H, Reed CR. Evidence for efficacy and tolerability of vilazodone in the treatment of major depressive disorder: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2009;70(3):326–333. | ||
Khan A, Cutler AJ, Kajdasz DK, et al. A randomized, double-blind, placebo-controlled, 8-week study of vilazodone, a serotonergic agent for the treatment of major depressive disorder. J Clin Psychiatry. 2011;72(4):441–447. | ||
Croft HA, Pomara N, Gommoll C, Chen D, Nunez R, Mathews M. Efficacy and safety of vilazodone in major depressive disorder: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2014;75(11):e1291–e1298. | ||
Mathews M, Gommoll C, Chen D, Nunez R, Khan A. Efficacy and safety of vilazodone 20 and 40 mg in major depressive disorder: a randomized, double-blind, placebo-controlled trial. Int Clin Psychopharmacol. 2015;30(2):67–74. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. | ||
Citrome L, Ketter TA. When does a difference make a difference? Interpretation of number needed to treat, number needed to harm, and likelihood to be helped or harmed. Int J Clin Pract. 2013;67(5):407–411. | ||
Jiang Q, Ahmed S. An analysis of correlations among four outcome scales employed in clinical trials of patients with major depressive disorder. Ann Gen Psychiatry. 2009;8:4. | ||
Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry. 2007;4(7):28–37. | ||
Targum SD, Houser C, Northcutt J, Little JA, Cutler AJ, Walling DP. A structured interview guide for global impressions: increasing reliability and scoring accuracy for CNS trials. Ann Gen Psychiatry. 2013;12(1):2. | ||
Brnabic A, Lin C, Monkul ES, Duenas H, Raskin J. Major depressive disorder severity and the frequency of painful physical symptoms: a pooled analysis of observational studies. Curr Med Res Opin. 2012;28(12):1891–1897. |
Supplementary material
  | Table S1 Institutional Review Boards |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.