Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
Catastrophic Cutaneous Polyarteritis Nodosa Exacerbated by Emotional Stress
Authors Bawany F, Lee G, Nousari Y, Ritchlin C, Singh P, Tausk F
Received 7 November 2022
Accepted for publication 23 December 2022
Published 30 December 2022 Volume 2022:15 Pages 2943—2947
DOI https://doi.org/10.2147/CCID.S396539
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Fatima Bawany,1 Gayin Lee,2 Yasmine Nousari,3 Christopher Ritchlin,2 Partik Singh,4 Francisco Tausk2,4
1Department of Dermatology, New York University, New York, NY, USA; 2Department of Medicine, University of Rochester Medical Center, Rochester, NY, USA; 3Mongan Institute, Massachusetts General Hospital, Boston, MA, USA; 4Department of Dermatology, University of Rochester Medical Center, Rochester, NY, USA
Correspondence: Francisco Tausk, Department of Dermatology, University of Rochester Medical Center, 601 Elmwood Ave, Box 697, Rochester, NY, 14642, USA, Email [email protected]
Abstract: We present the first case of a patient with indolent polyarteritis nodosa who suffered severe exacerbations following significant emotional stressors. This report highlights the close relationship between emotions and autoimmune diseases mediated by the deleterious effects of stressors presumptively by skewing immunity from Type 1 to Type 2.
Keywords: psychology, autoimmunity, vasculitis, stressors
Introduction
Polyarteritis nodosa (PAN) is a systemic necrotizing vasculitis that affects medium-sized and small muscular arteries, which most authors consider an autoimmune disorder. Cutaneous PAN (CPAN) is a variant that targets mainly the skin.1,2 A large body of evidence supports the relationship between stress and autoimmunity, suggesting that stressors may trigger or exacerbate autoimmune diseases.3–5
Throughout evolution, animals, including humans, have developed a critical survival mechanism that allows them to deal with short-lived external stressors such as the presence of predators; this acute stress response is adaptive and immunologically protective with a duration of minutes to hours. In contrast, exposure to a stressor for a more extended period, depending on the individual makeup of the subject,6 may lead to a non-adaptive response, significant disruption of the immune system, dysregulation of the circadian cortisol rhythm, and downregulation of the glucocorticoid receptors.6–10
This report highlights a case of smoldering CPAN in which emotional stress appears to have triggered a devastating disease exacerbation.
Case Description
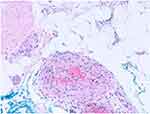
A 54-year-old woman with a long-standing history of well-controlled psoriatic arthritis on adalimumab and methotrexate presented with a five-month duration of a slowly progressive blanching livedo reticularis that started on bilateral dorsal feet and toes and extended to the calves (Figure 1). Her blood pressure was normal, like the rest of her physical examination. She denied paresthesia, pain, constitutional or other symptoms. Aside from a slightly elevated sedimentation rate (32mm/h), additional pertinent laboratory evaluations, including complete blood cell, comprehensive metabolic panel, LDH, β-2 microglobulin, rheumatoid factor, C3, C4, CH50, anti-CCP, ANCA, ANA, anti-SSA, anti-SSB, anti-SM, anti-RNP, anti-dsDNA, anti-cardiolipins, anti-β-2 glycoprotein1, lupus anticoagulant, ANCA, anti-MPO, anti-PR3, hepatitis B, hepatitis C, HIV, serum and urine light chain, urine protein immunofixation and complete urinalysis, were negative or within normal limits. The echocardiogram and CT angiography of the chest, abdomen, and pelvis were unremarkable. An incisional full-thickness skin biopsy of the right calf that included an unaffected center and adjacent reticulated area revealed a leukocytoclastic and necrotizing medium and small muscular artery vasculitis (Figure 2). The results were relayed to the patient, who immediately began researching PAN on the internet, becoming intensely distressed. Over the next two days, she developed excruciating pain and dysesthesia of her legs and feet, prompting her admission to the hospital, where her physical examination was notable for purple, cool, and numbed second to fifth digits of the right foot as well as livedo racemosa throughout the bilateral lower extremities and pinnae. Blood pressure remained normal, and there was no evidence of renal or systemic involvement. She was initiated on 3-day intravenous (IV) pulses of methylprednisolone followed by oral prednisone, pentoxifylline, nifedipine, aspirin, topical nitroglycerin, and enoxaparin. During her 28-day hospital course, the lesions on her ears resolved. Still, she developed worsening necrosis of the affected toes of her right foot (Figure 3) and marked improvement in pain and dysesthesia. She was initiated on six bi-weekly IV pulses of cyclophosphamide, IV rituximab every six months, and oral prednisone tapering, which continued upon discharge. Over the next several months, her mummified digits autoamputated. Her PAN remained otherwise well controlled on rituximab, daily low-dose azathioprine, and weekly oral methotrexate with no evidence of systemic disease.
 |
Figure 1 Initial presentation. Slowly progressive blanching livedo reticularis. |
 |
Figure 3 Necrotic toes. |
Nineteen months following her hospital admission, she was presented with a new flare with painful livedo reticularis of the lower extremities. This happened in the context of family issues. As a result, prednisone was restarted, and the methotrexate dose was increased. As her lesions and symptoms persisted, she was readmitted, receiving IV pulses of methylprednisolone and cyclophosphamide and continued oral prednisone tapering. After several weeks of treatment, she eventually achieved remission and was re-transitioned to oral methotrexate and rituximab.
The patient’s disease remained well controlled for about 3.5 years. Around this time, she was involved in a motor vehicle accident resulting in splenic rupture, and her mother contracted COVID-19. She returned to the clinic with painful livedo reticularis and livedo racemosa of the second and third digits of the left foot, the first digit of the right foot (Figure 4), and the joint lines of the digits of the bilateral hands. She again received IV pulses of methylprednisolone, cyclophosphamide, oral tapering prednisone, nifedipine, and pentoxifylline. After two weeks, her symptoms and lesions began to improve, and she was transitioned to oral mycophenolate mofetil for maintenance therapy which she remained on. Twelve months later, her symptoms and lesions show near-complete resolution, with well-healed ulcers on her feet.
 |
Figure 4 Livedo racemosa of the first toe. Note auto-amputated second to fifth toes of the right foot. |
Discussion
The skin lesions of cPAN most often present with tender subcutaneous and deep dermal nodules, livedo reticularis, and much less commonly livedo racemosa, retiform purpura, ulcerations, digital ischemia, and digital infarcts. Virtually all cPAN cases involve the lower extremities, with most patients having relatively indolent yet chronic relapsing and remitting course.1,2
This case’s salient features lie in the severity of the cPAN and the sequence of stressors followed by disease exacerbations. Although this is the first report of stress-exacerbated cPAN, numerous studies have shown the close relationship between stressful life events and the flaring of various autoimmune diseases such as Graves’ Disease, rheumatoid arthritis, Sjogren’s Syndrome, multiple sclerosis, and ANCA vasculitis.4,5 An interesting aspect of our patient lies in the fact that she presented two diseases (psoriasis and cPAN) found at opposite poles of the TH1/TH2 immune response. This can be explained by numerous reports documenting the development of autoimmune diseases, particularly vasculitis, following treatments with anti-TNF agents, as seen in this patient.11–16
Underlying this phenomenon, stressors mediate the switch from Type 1 to Type 2 humoral immune response by activating the HPA-axis and the sympathetic nervous system (SNS). For example, catecholamines were shown to stimulate IL4 and IL-10 production by immune cells and inhibit TNF-α and IL-12 production. Similarly, glucocorticoids promote the Type 2 cytokines IL-4, IL-10, and IL-13 and reduce the production of the Type 1 cytokines IFN-γ and TNF-α.17,18 More importantly, nor-epinephrine (NE) secreted by peripheral nerves of the SNS can reach high tissue concentrations during stress and have profound effects on immune cells carrying β-2 adreno-receptors, resulting in a shift in the ratio of TH1/TH2.19 This favors the secretion of TH2-type cytokines and the dominance of humoral immunity, which triggers the exacerbation of autoimmune diseases20 as presumptively seen in our patient, albeit serum levels of cytokines and stress hormones were not assessed.
Interestingly, all the components of the HPA axis are reproduced in the skin; it is the only peripheral organ that mirrors the central HPA axis, leading to the notion that stressors can induce the production of CNS peptides and finally produce cutaneous glucocorticosteroids as well as induce the secretion of immunomodulatory cytokines by keratinocytes.21
Conclusion
Our report suggests that stress and flares of autoimmunity are closely intertwined and call for a biopsychosocial approach to patient care. Just as we prescribe medical therapies to achieve disease remission so should we provide resources to address our patients’ psychological health to ameliorate the stress responses that can trigger a relapse.22
Ethics and Consent Statements
Appropriate informed consent to publish this case report including all the images has been obtained from the patient. The Institutional Review Board of the University of Rochester does not review case reports.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Stone JH, Nousari HC. ”Essential” cutaneous vasculitis: what every rheumatologist should know about vasculitis of the skin. Curr Opin Rheumatol. 2001;13(1):23–34. doi:10.1097/00002281-200101000-00005
2. De Virgilio A, Greco A, Magliulo G, et al. Polyarteritis nodosa: a contemporary overview. Autoimmun Rev. 2016;15(6):564–570. doi:10.1016/j.autrev.2016.02.015
3. Song H, Fang F, Tomasson G, et al. Association of stress-related disorders with subsequent autoimmune disease. JAMA. 2018;319(23):2388–2400. doi:10.1001/jama.2018.7028
4. Sharif K, Watad A, Coplan L, et al. The role of stress in the mosaic of autoimmunity: an overlooked association. Autoimmun Rev. 2018;17(10):967–983. doi:10.1016/j.autrev.2018.04.005
5. Golemati CV, Mavragani CP, Lionaki S, Karaiskos D, Moutsopoulos HM. Stress and disease onset in antineutrophil cytoplasmic antibody-associated vasculitis. Front Psychiatry. 2017;8:286. doi:10.3389/fpsyt.2017.00286
6. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi:10.1056/NEJM199801153380307
7. Dhabhar FS, Malarkey WB, Neri E, McEwen BS. Stress-induced redistribution of immune cells--from barracks to boulevards to battlefields: a tale of three hormones--Curt Richter award winner. Psychoneuroendocrinology. 2012;37(9):1345–1368. doi:10.1016/j.psyneuen.2012.05.008
8. Dhabhar FS. Effects of stress on immune function: the good, the bad, and the beautiful. Immunol Res. 2014;58(2–3):193–210. doi:10.1007/s12026-014-8517-0
9. Dhabhar FS, McEwen BS. Acute stress enhances while chronic stress suppresses cell-mediated immunity in vivo: a potential role for leukocyte trafficking. Brain Behav Immun. 1997;11(4):286–306. doi:10.1006/brbi.1997.0508
10. Antoni MH, Dhabhar FS. The impact of psychosocial stress and stress management on immune responses in patients with cancer. Cancer. 2019;125(9):1417–1431. doi:10.1002/cncr.31943
11. da Silva Cendon Duran C, da Paz AS, Barreto santiago M. Vasculitis induced by biological agents used in rheumatology practice: a systematic review. Arch Rheumatol. 2022;37(2):300–310. doi:10.46497/ArchRheumatol.2022.9049
12. Ramos-Casals M, Brito-Zeron P, Munoz S, et al. Autoimmune diseases induced by TNF-targeted therapies: analysis of 233 cases. Medicine. 2007;86(4):242–251. doi:10.1097/MD.0b013e3181441a68
13. Ramos-Casals M, Brito-Zeron P, Soto MJ, Cuadrado MJ, Khamashta MA. Autoimmune diseases induced by TNF-targeted therapies. Best Pract Res Clin Rheumatol. 2008;22(5):847–861. doi:10.1016/j.berh.2008.09.008
14. Reitblat T, Reitblat O. Appearance of ANCA - associated vasculitis under Tumor necrosis factor-alpha inhibitors treatment. Am J Case Rep. 2013;14:80–82. doi:10.12659/AJCR.883841
15. Sokumbi O, Wetter DA, Makol A, Warrington KJ. Vasculitis associated with tumor necrosis factor-alpha inhibitors. Mayo Clin Proc. 2012;87(8):739–745. doi:10.1016/j.mayocp.2012.04.011
16. Anandacoomarasamy A, Kannangara S, Barnsley L. Cutaneous vasculitis associated with infliximab in the treatment of rheumatoid arthritis. Intern Med J. 2005;35(10):638–640. doi:10.1111/j.1445-5994.2005.00899.x
17. Ramirez F, Fowell DJ, Puklavec M, Simmonds S, Mason D. Glucocorticoids promote a TH2 cytokine response by CD4+ T cells in vitro. J Immunol. 1996;156(7):2406–2412.
18. Kim BJ, Jones HP. Epinephrine-primed murine bone marrow-derived dendritic cells facilitate production of IL-17A and IL-4 but not IFN-gamma by CD4+ T cells. Brain Behav Immun. 2010;24(7):1126–1136. doi:10.1016/j.bbi.2010.05.003
19. Elenkov IJ, Wilder RL, Chrousos GP, Vizi ES. The sympathetic nerve--an integrative interface between two supersystems: the brain and the immune system. Pharmacol Rev. 2000;52(4):595–638.
20. Bellocchi C, Carandina A, Montinaro B, et al. The interplay between autonomic nervous system and inflammation across systemic autoimmune diseases. Int J Mol Sci. 2022;23(5):2449. doi:10.3390/ijms23052449
21. Pondeljak N, Lugovic-Mihic L. Stress-induced interaction of skin immune cells, hormones, and neurotransmitters. Clin Ther. 2020;42(5):757–770. doi:10.1016/j.clinthera.2020.03.008
22. Stress Triggers Disease Flares in Patients With Vasculitis. Study shows psychological health important to controlling wegener’s granulomatosis; 2011. Available from: https://www.hss.edu/newsroom_stress-triggers-vasculitis-flares.asp.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.