Back to Journals » International Medical Case Reports Journal » Volume 13
Case Report on Giant Pars Plana Cysts Mimicking Retinal Detachment
Authors Braceros KK , Choi D, Gallemore R
Received 5 March 2020
Accepted for publication 27 April 2020
Published 20 May 2020 Volume 2020:13 Pages 191—194
DOI https://doi.org/10.2147/IMCRJ.S252129
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kathryn Kelani Braceros,1 Dale Choi,2 Ron Gallemore1
1Retina Macula Institute, Torrance, CA, USA; 2Hope Vision Care, Torrance, CA, USA
Correspondence: Ron Gallemore Tel +1 310 413 7020
Email [email protected]
Purpose: To report a case of peripheral elevated lesions mimicking retinal detachment which were ultimately ascertained to be giant pars plana cysts through ophthalmoscopy with scleral depression.
Methods: This was a case report documented with ophthalmoscopy and Optos imaging.
Results: Patient initially referred for assessment of bilateral retinal detachment was found by careful ophthalmoscopy with scleral depression to have bilateral giant pars plana cysts with no frank retinal breaks.
Conclusion: Large pars plana cysts may mimic retinal detachment or other peripheral retinal pathology. The lesions in question were found to originate from the pars plana and overhang the retina. No frank retinal breaks or associated rhegmatogenous retinal detachments were noted in either eye. Ophthalmoscopy with a complete scleral depressed exam allowed for the differentiation.
Keywords: peripheral retinal elevation, pars plana, fundus pathology
Introduction
Peripheral retinal pathology picked up on routine exam can be concerning – tumors, retinal detachment, and congenital lesions that have implications for systemic health may be identified. Careful ophthalmoscopy with scleral depression can help differentiate between retinal pathology of concern and more benign retinal changes, such as pars plana cysts (PPC). It is of utmost importance that pars plana cysts are differentiated from retinal detachments (RD), as the latter almost always require prompt treatment. We encountered a very rare case of giant PPC mimicking RD and report the case here to add to your list of unusual peripheral retina disorders.
Case Report
A 32-year-old Caucasian male presented with a history of abnormal retinal findings. Upon routine optometric exam, the patient was noted to have temporal elevated retinal tissue suspicious for rhegmatogenous RD in both eyes and was subsequently referred to a retina specialist for further evaluation. The patient was asymptomatic, denying any flashes, floaters, loss of peripheral vision, or distortion. Best corrected visual acuity was 20/20 in the right eye and 20/20 -1 in the left eye. The patient presented with full confrontational visual fields in both eyes. His intraocular pressures were 16 mmHg and 17 mmHg, respectively. He denies any family history of RD. Upon exam with scleral depression, there were irregularly elevated mass-like lesions in both eyes that were localized to the pars plana. The cyst extended from the clock hours of 8:30ʹ to 9:30ʹ in the right eye and 2:30ʹ to 3:30ʹ in the left eye with no associated rhegmatogenous RD in either eye. There were some pigmentary changes noted posterior to the ora serrata but the lesions themselves originated in the pars plana/pars plicata region and overhung the ora serrata. The left eye had an apparent area of schisis within the cyst but the lesion was indeed overhanging, and not a part of, the retina. Their location, elevation, and fluid-filled appearance were consistent with PPC and not RD. Furthermore, the lesion had a somewhat irregular border whereas schisis typically has a smooth border. Given the presence of pigmentation that was noted on the posterior side of the ora serrata traction was suspected as a possible factor for causing these large, cystic changes as well as the pigmentation. Indeed, the patient was referred with a diagnosis of rhegmatogenous RD. The diagnostic key was a complete scleral depressed exam. Wide field fundus photography was performed in both eyes to document the cysts (Figures 1 and 2), however, we were unable to image the entire lesions or even the pars plana clearly with our imaging systems. No frank retinal breaks were appreciated and no treatment was required. The fluid did not extend across the ora serrata in either eye so only observation was advised.
 |
Figure 1 Fundus image of the right eye showing pars plana cyst temporally from 8:30ʹ to 9:30ʹ. |
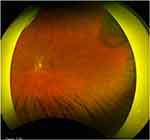 |
Figure 2 Fundus image of the left eye showing pars plana cyst temporally from 2:30ʹ to 3:30ʹ. |
Discussion
Pars plana cysts form when epithelial cell layers separate either between the non-pigmented ciliary epithelium and pigmented epithelium, or within the non-pigmented epithelium itself. These bullous elevations are localized to the pars plana and are clear and smooth, typically presenting in the shape of oblong cysts. PPC have been found most commonly to conform to a single oral bay, ranging from 0.25 to 2.5 disc diameters in size.1 Larger cysts have been noted to extend from the ora serrata to the ciliary processes, with some noted to span across several oral bays,2 often the result of multiple neighboring cysts becoming confluent. Per a study conducted by Allen et al,2 PPC have a tendency to be smaller and more numerous when located posteriorly versus larger and scanty when located anteriorly.
One of the first reported cases of PPC was by Kuhnt in 1881, where he describes such cysts as being found typically in senile eyes and accompanied by other common changes in the aging eye.2,3 In a study by Okun et al4 of 494 autopsy eyes from 250 autopsies, PPC were one of the more common retinal pathologies, being observed in 16% of autopsies. Further studies have shown that PPC are found in up to 18% of the normal population.5 No patients under the age of 40 were found to have PPC, concurring with Kuhnt’s observation that cysts of this type were an age-related change.
Previous research has made an association between other abnormalities of the peripheral retina (e.g., retinoschisis, retinal dialysis, and cystoid degeneration) and PPC. PPC tend to be larger and more numerous in areas where retinoschisis is adjacently present.2,6-8 Moreover, studies have shown PPC to be filled with hyaluronic acid, which is the same substance found in the cystoid spaces and schisis of the peripheral retina,8 further suggesting a relation. On exam, PPC can be difficult to differentiate from other peripheral retinal pathology, namely schisis and RD, as they have qualities similar to each other. PPC classically present as translucid bullous elevations localized to the pars plana. Schisis has a distinct, smooth border and appears immobile. Schisis can also have visible blood vessels on the inner retinal layer that may appear white.9 There are also distinct factors which differentiate PPC from RD. On exam, retinal detachments, if not rhegmatogenous, are associated with retinal breaks and can appear to have a wrinkled surface that is mobile and can change shape with or without scleral depression.
Due to their location in the extreme fundus periphery, methods of examination typically include indirect ophthalmoscopy with scleral depression. Through experimentation on both patients and enucleated eyes, Schepens et al10 found that indirect ophthalmoscopy was superior to direct ophthalmoscopy when examining the extreme fundus periphery. Ultrasound biomicroscopy can also be performed for a more detailed study.
Pars plana cysts are not typically considered a precursor for RD, and the literature is currently too limited to define a significant relationship between pars plana cysts and their frequency and severity in eyes with RD. In incidences where RD and PPC are present in the same eye, there are typically significant pathological findings, namely traction, in the region of the ora serrata.6 Schepens et al10 have alluded to PPC as being analogous to RD of the visual retina; however, PPC are distinguishable in that they are not commonly associated with retinal holes, they are commonly seen in groups, and they increase in number and size with age.2
Pars plana cysts are a common peripheral retinal pathology that do not raise much clinical concern. They do not affect the central vision and observation alone is typically recommended.
Conclusion
Pars plana cysts are something to be considered when peripheral retinal elevation is noted on routine exam. They must be distinguished from other peripheral fundus abnormalities such as retinal detachment or retinoschisis, as the treatment plans for each can vary widely. This distinction is most effectively done by careful ophthalmoscopy with scleral depression. In the aforementioned case, scleral depression revealed the origin of the cysts to be from the pars plana with the cysts themselves overhanging the ora serrata as opposed to extending past it. On clinical exam, PPC are translucent, smooth, oval-shaped cysts localized to the pars plana. While schisis also appears translucent and smooth it can present anywhere on the fundus. During scleral depression, schisis remains taut and can be differentiated from retinal detachments, which display more surface wrinkling and mobility with scleral depression. PPC themselves are innocuous and observation alone is often recommended to ensure there is no extension of the fluid into the visual retina.
Ethics
Written informed consent has been obtained from all patients to have case details and any accompanying images published. No institutional approvals were required for the publishing of this case report.
Author Contributions
All authors attest that they meet the current ICMJE criteria for authorship. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zinn KM. Clinical Atlas of Peripheral Retinal Disorders. New York: Springer-Verlag; 1988:18.
2. Allen RA, Miller DH, Straatsma BR. Cysts of the posterior ciliary body (pars plana). Arch Ophthalmol. 1961;66(3):302–313. doi:10.1001/archopht.1961.00960010304003
3. Kuhnt. Atrophie des Uvealtractus, Zehenders Klin. Monatsbl. 1881. cited by Coates, G. Royal London Ophthal. Hosp Rep. 1907;17:43.
4. Okun E. Gross and microscopic pathology in autopsy eyes*: Part IV. Pars plana cysts. Am J Ophthalmol. 1961;51(6):1221–1228. doi:10.1016/0002-9394(61)92461-8
5. Kumar V, Kumar P, Roy S, Padhy SK. Pars plana cysts. Ophthalmic Surg Lasers Imaging Retina. 2018;49(10):e169–e170. doi:10.3928/23258160-20181002-24
6. Grignolo A, Schepens CL, Heath P. Cysts of the pars plana ciliaris: ophthalmoscopic appearance and pathological description. AMA Arch Ophthalmol. 1957;58(4):530–543. doi:10.1001/archopht.1957.00940010548008
7. Ruiz RS. Giant cyst of the pars plana. Am J Ophthalmol. 1971;72:481–482. doi:10.1016/0002-9394(71)91324-9
8. Mannino G, Malagola R, Abdolrahimzadeh S, Villani GM, Recupero SM. Ultrasound biomicroscopy of the peripheral retina and the ciliary body in degenerative retinoschisis associated with pars plana cysts. Br J Ophthalmol. 2001;85(8):976–982. doi:10.1136/bjo.85.8.97
9. Degenerative retinoschisis. Institute de la vision. Available from: http://www.institut-vision.org/en/institute/28-diseases/94-degenerative-retinoschisis.html?showall=1&limitstart=.
10. Schepens CL, Bahn GC. Examination of the ora serrata: its importance in retinal detachment. AMA Arch Ophthalmol. 1950;44(5):677–690. doi:10.1001/archopht.1950.00910020689006
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
