Back to Journals » Clinical Interventions in Aging » Volume 16
Cardiac Delirium Index for Predicting the Occurrence of Postoperative Delirium in Adult Patients After Coronary Artery Bypass Grafting
Authors Lechowicz K , Szylińska A , Listewnik M , Drożdżal S, Tomska N , Rotter I , Kotfis K
Received 18 January 2021
Accepted for publication 26 February 2021
Published 17 March 2021 Volume 2021:16 Pages 487—495
DOI https://doi.org/10.2147/CIA.S302526
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Kacper Lechowicz,1 Aleksandra Szylińska,2 Mariusz Listewnik,3 Sylwester Drożdżal,4 Natalia Tomska,2 Iwona Rotter,2 Katarzyna Kotfis1
1Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, Szczecin, 70-111, Poland; 2Department of Medical Rehabilitation and Clinical Physiotherapy, Pomeranian Medical University in Szczecin, Szczecin, 71-210, Poland; 3Department of Cardiac Surgery, Pomeranian Medical University in Szczecin, Szczecin, 70-111, Poland; 4Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, Szczecin, 70-111, Poland
Correspondence: Katarzyna Kotfis
Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, Al. Powstańców Wielkopolskich 72, Szczecin, 70-111, Poland
Tel +48 91-466-11-44
Email [email protected]
Background: Postoperative delirium (POD) is a serious complication of cardiac surgery. It is an acute neuropsychiatric syndrome. The aim of this study was to analyze the CARDEL Index, composed of advancing age, preoperative glycated hemoglobin and the platelet-to-WBC ratio (PWR) previously described and calculated, using a different patient database, to assess its usefulness as a marker for predicting postoperative delirium after coronary artery by-pass grafting (CABG).
Methods: A retrospective analysis of 1098 patients who underwent, isolated CABG procedures between 2017 and 2019 was performed.
Results: Within the study group, 164/1098 (14.93%) patients were diagnosed with delirium. Preoperative inflammatory parameters were elevated in patients with delirium: White Blood Cell count (p=0.003), Neutrophil count (p=0.016) and C-reactive protein (p< 0.001). A decrease in preoperative PWR was shown in patients with delirium (p=0.008). Delirious patients spent more time mechanically ventilated (p< 0.001) and had longer hospitalization times (p=0.002). Mortality at 1 year was significantly higher in patients with POD (p< 0.001). The CARDEL Index in this study group for POD detection has the largest area under the curve (AUC) of 0.664 (p< 0.001) and a cut-off value of 8.08.
Conclusion: CARDEL Index may be treated as a potentially valuable tool for delirium prediction in patients after CABG.
Keywords: delirium, POD, CAM-ICU, cardiac surgery, CABG, coronary artery bypass grafting
Introduction
Cardiosurgical operations are complicated medical procedures, which may lead to significant complications. The most common postoperative complications include: surgical (operative mortality, reoperation, deep sternal wound infection), associated with organ dysfunction (cardiovascular failure, renal failure, prolonged intubation) and neurological disorders (perioperative stroke, postoperative delirium).1,2 According to the data reported by the Society of Thoracic Surgeons (STS), in year 2018, coronary artery bypass grafting (CABG) which is particularly common surgical procedures in heart surgery, accounted for 55% of all operations, which translates into 157,704 isolated operations in the United States.3
Postoperative delirium (POD) is a serious postoperative complication. It is an acute neuropsychiatric syndrome defined in The Diagnostic and Statistical Manual of Mental Disorders (DSM–5) as a disturbance of consciousness, along with reduced clarity of awareness of self and the environment with reduced ability to focus or sustain attention.4 The incidence of delirium is estimated at 26% to even 85% in patients who are mechanically ventilated in the intensive care units (ICU).5,6 Postoperative delirium in cardiac surgery occurs in 3 to 52% of patients.7,8 The complications of delirium include prolonged mechanical ventilation (MV), prolonged duration of ICU and hospital stay, higher mortality, postoperative cognitive dysfunction and loss of independence. Bilotta et al reported that the risk factors of POD fall into 4 categories: demographic (ie age > 70, male sex, presence of substance abuse, malnutrition), comorbidities (ie dementia, psychiatric disorders, physical impairment, hypertension, diabetes mellitus, heart failure, chronic atrial fibrillation, cerebral vascular disease), surgery-related (ie cardiac surgery, increased EuroScore) and anesthesia-related (ie use of benzodiazepines, grade 3 and of the American Society of Anesthesiologists (ASA), fluid fasting time longer than 6 hours, transfusion of more than 800 mL of blood).9
The same or similar parameters can be observed in patients undergoing cardiac surgery due to many burdens associated with coronary artery diseases, such as: diabetes, hypertension, atrial fibrillation (AF), and obstructive pulmonary disease (COPD).10,11 In the analysis of delirium risk factors, it is worth paying attention to the age of the patients, as studies have shown that the risk of POD increases with advancing age.8
Pain and its treatment is also an important risk factor for delirium. Cardiac surgery causes severe pain that can directly contribute to delirium, and opioid use is also a known risk factor.7 Pain is inherent in cardiac surgery. The influence of opioids and pain on the occurrence of delirium is not entirely clear. It has been proven that the presence of significant pain and high doses of opioids increases the risk of postoperative delirium, especially in the presence of significant preoperative risk.12 In studies where pain was adequately treated, despite the use of opioids, the incidence was less than average.13 The type of opioid used is also of great importance. The highest risk of delirium is the use of meperidine. The use of hydromorphone and fentanyl seems to be relatively safe compared to other opioids, OR = 0.22–0.3. Morphine, used in our center, increases the risk of delirium with OR = 1.2–2.32.14 An additional factor that distinguishes cardiac surgery is the use of cardiopulmonary bypass (CPB) and aortic cross-clamping. As a result, chemokines are released, leading to systemic inflammation and the disruption of the blood–brain barrier (BBB).15
In clinical practice, the majority of patients with delirium remain undiagnosed and the rate of delirium is underreported.16 There are methods for delirium detection, such as ICDSC (Intensive Care Delirium Screening Checklist) and CAM-ICU (Cognitive Assessment Method for ICU),17 however they are rarely used outside of research settings, although this is changing.16,18 For this reason, scientists’ efforts are focused on discovering simple biomarkers or biomarker panels that would allow for proper, timely diagnosis as well as correct prediction of POD. The costs of a biomarker and the ease of its use alongside a simple delirium detection scale, play a significant role when looking for an appropriate test or marker.
The pathogenesis of delirium has not been fully elucidated and understood.19 Some potential mechanisms have been identified, which include the neurotransmitter imbalance (ie acetylcholine deficiency with excess dopamine), decreased cerebral blood flow and metabolism, inadequate response to stress, disturbed sleep-wake cycle and generalized inflammation.20 Inflammation markers are easily measurable, but interpretation remains problematic due to their increase or decrease over time and due to the presence of other risk factors for delirium.21 One of the possible options to aid delirium detection is to use white blood cell derived parameters, which provide information about generalized inflammation in the body and have been associated with delirium.22–24 Markers such as Neutrophil-to-Lymphocyte Ratio (NLR), along with Platelet-to-Lymphocyte Ratio (PLR) and Platelet-to-WBC ratio (PWR) are important in delirium prediction. They are provided by routine laboratory analyses performed in each patient prior to cardiac surgery.24,25 In their previous work, Kotfis et al analyzed the significance of white cell inflammatory biomarkers in predicting POD after cardiac surgery.23 The authors have shown that lower preoperative levels of PWR and PLR were associated with the occurrence of postoperative delirium. Based on the coefficients of logistic regression, the authors suggested that an index composed of age, preoperative level of glycated hemoglobin (HbA1c), and preoperative PWR, called the CARDEL Index, may be clinically useful for prediction of postoperative delirium after CABG at minimal cost.
The aim of this study was to retrospectively analyze the CARDEL index previously described and calculated,23 using a different prospectively collected database, to assess its usefulness as a marker to predict postoperative delirium after coronary artery bypass grafting.
Patients and Methods
Study Population
All patients undergoing CABG at a university cardiac surgery department, between January 1st, 2017 and December 31st, 2018 were included in a retrospective analysis. Patients with mental disorders, including Alzheimer’s disease, depression, epilepsy, dementia, patients who died within the first 24 hours after surgery, patients with pneumonia within 24 hours after surgery, and those who did not have complete laboratory tests were excluded from the study. The study included patients undergoing CABG with the use of cardio-pulmonary bypass (CPB). Depending on the presence [Delirium (+)] or absence [Delirium (-)] of delirium after surgery the patients were divided into two groups (Figure 1).
 |
Figure 1 Study flowchart. Abbreviation: n, number of patients. |
Data Collection
Demographic data, preoperative data and comorbidities were extracted from medical documentation. The information about preoperative comorbidities included: cardiovascular diseases (ie atrial fibrillation, congestive heart failure, myocardial infarction, hypertension), organ disorders (acute kidney injury, chronic obstructive pulmonary disease), metabolic (impaired glucose tolerance, diabetes, dyslipidemia, thyroid disorders) and neurological (transient ischemic attack, stroke). The patients were classified according to the Canadian Cardiovascular Society grading scale (CCS) for ischemia, heart failure was classified according to the New York Heart Association (NYHA), and EuroScore Logistic 2 scale to calculate perioperative risk for patients.26 Intraoperative and postoperative data were collected and included: laboratory testing, surgical data (total time of aortic cross-clamping, time of reperfusion, numbers of grafts, intraoperative hemofiltration), intubation and re-intubation times. In addition, we collected information regarding postoperative complications. The ICU length of stay (LOS) and hospitalization time, as well as 1-month and 1-year mortality were collected. We used CAM-ICU method for delirium screening, which was performed twice a day, by trained personnel (nurse or physician). The final diagnosis was made based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM V) 4 after chart review performed by the same trained team member for additional information that could aid the detection of delirium.
Ethical Consideration
We performed the study in accordance with the Helsinki Declaration. Patient consent to review their medical records was not required by the Bioethical Committee of the Pomeranian Medical University. The study was observational in nature; therefore, it received a waiver from the Bioethical Committee of the Pomeranian Medical University (decision no. KB-0012/257/06/18). We used only de-identified patient data to ensure confidentiality.
Statistical Analysis
To characterize the study population descriptive statistics were used. Categorical variables were presented as proportions. Continuous variables were presented as means with SD and a median. To compare qualitative data Chi-square test or chi-square test with Yates correction was used. To check the normality of distribution the Shapiro–Wilk test was used. In order to compare continuous variables, we used the Mann–Whitney U-test. We performed multivariate logistic regression analysis for variables associated with delirium. The parameters used for multivariate analysis are included in the CARDEL Index described by Kotfis et al.23 The CARDEL Index analysis was performed for patients with or without delirium. Index described previously by Kotfis et al: CARDEL Index = 0.108 × Age + 0.341 × HBA1C − 0.049 × PWR.23
Moreover, to determine the diagnostic value of the CARDEL index and its components for predicting delirium a receiver operating characteristic (ROC) analysis was performed. The p-value ≤ 0.05 was considered significant. We used licensed Statistica 13 (StatSoft, Inc. Tulsa, OK, USA).
Results
Out of entire group of 1098 patients included in the analysis, 164/1098 (14.93%) were diagnosed with POD (Table 1). Patients with POD were older (69.24±9.23 years vs 64.79±9.74 years, p<0.001), presented with higher index EuroScore Logistic II (6.79±8.79% vs 4.04±6.66%, p<0.001), had higher preoperative level of glycated hemoglobin (6.45±1.25 vs 6.18±1.02, p<0.001), creatinine (1.19±0.85 mg/dL vs 1.03±0.76 mg/dL, p<0.001), and lower level of GFR (68.50±22.58 mL/min/1.73m2 vs 78.19±20.34 mL/min/1.73m2, p<0.001).
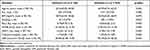 |
Table 1 Demographic and Preoperative Data |
Data regarding concomitant diseases are shown in Table 2. Patients with postoperative delirium presented significantly more frequently with myocardial infarction (p<0.001), atrial fibrillation (paroxysmal, p<0.001; persistent or permanent, p=0.029), diabetes (on insulin, p=0.001; on oral drugs, p=0.009), stroke (p=0.023), internal carotid artery stenosis (p=0.020), extracardiac atherosclerosis (p=0.003), renal failure (chronic, p<0.001; acute, p=0.010).
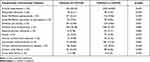 |
Table 2 Comorbidities in Patients with and without Delirium |
Increased levels of preoperative inflammatory parameters were seen in patients who developed delirium after CABG (Table 3): white blood cell count (8.52±3.22 vs 7.88±2.58 G/L, p=0.003), neutrophil count (5.59±2.87 G/L vs 5.09±2.29 G/L, p=0.016) and C-reactive protein (13.59±28.29 mg/L vs 8.30±23.79 mg/L, p<0.001). In addition, a decrease in platelet-to-WBC ratio (PWR) was seen in patients with delirium (29.39±11.89 vs 30.84±10.57, p=0.008).
 |
Table 3 Inflammatory and Derived Parameters for Patients with and without Delirium |
Outcome data are presented in Table 4. Patients with delirium had longer time of mechanical ventilation (1945.67±6141.51 minutes vs 1202.77±5797.96 minutes, p<0.001), longer CPB (cardiopulmonary bypass) time (57.32±16.75 vs 55.14±17.35 minutes, p=0.40) and longer hospital length of stay (13.82±14.84 days vs 9.19±7.87 days, p<0.001). Moreover, mortality at 1 year was significantly higher in the group of patients diagnosed with postoperative delirium (18.97% vs 9.64%, p<0.001).
 |
Table 4 Postoperative Outcome |
The CARDEL Index analysis was performed for patients with or without delirium. Index described previously by Kotfis et al.23 The CARDEL Index formula is shown below.
CARDEL Index = 0.108 × Age + 0.341 × HBA1C − 0.049 × PWR
The analysis showed statistically significant differences in the values of the CARDEL Index in patients with or without delirium (p <0.001). Data are presented in Table 5.
 |
Table 5 CARDEL Index in Patients with or without Delirium |
The Shapiro–Wilk test showed that the distribution slightly differs from the normal one (p = 0.001) (Figure 2).
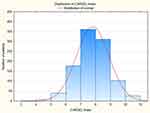 |
Figure 2 Distribution of the CARDEL Index. Abbreviation: CARDEL Index, Cardiac Delirium Index. Notes: Red line – Description of normal; Shapiro–Wilk test: p-value = 0.001. |
A multivariate logistic regression analysis was performed (Table 6), including advancing age, glycated hemoglobin and PWR for patients with delirium, which are the parameters included in the CARDEL Index.
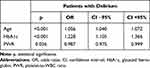 |
Table 6 Multivariate Logistic Regression Analysis for the Parameters Used in CARDEL Index |
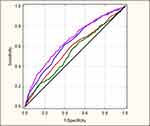
Figure 3 shows the ROC curve with the CARDEL Index.
The results show that the area under the curve for the CARDEL Index is larger than that of any of the other parameters (AUC 0.664, p<0.001) and has a cut-off value of 8.08 (Table 7).
 |
Table 7 Characteristics of the ROC Curve Results for Selected Parameters |
Discussion
Despite the development of technology and research methods, the rate of delirium detection remains inadequate. In this study the authors aimed to searching for the most ideal model for predicting delirium based on preoperative clinical data and laboratory results, to determine their usefulness in predicting POD after coronary artery bypass grafting. The analysis of these patient groups showed that the delirium risk factors listed by Bilotta et al were statistically significant.9 The delirium (+) group was characterized by higher age, increased overall risk of surgery on the ESL2 scale, as well as increased inflammatory parameters, increased creatinine and HbA1C levels. These patients have statistically significant more concomitant diseases such as atrial fibrillation, myocardial infarction, diabetes, strokes, acute and chronic renal failure, atherosclerosis and internal carotid artery stenosis. In this group, the hospital stay was also longer, and the 30-day and 1-year mortality was increased. The analysis of these data forces us to look for methods of predicting the occurrence of delirium in order to implement preventive treatment and provide patients with special care. The authors retrospectively analyzed the CARDEL Index (Cardiac Delirium Index) which is based on objective preoperative parameters included in multivariable model based on advancing age, glycated hemoglobin and platelet-to WBC ratio for optimal prediction of postoperative delirium.23
The results of the study showed that any of these factors independently is not as good as the CARDEL Index at predicting POD after coronary artery by-pass grafting. The advantage of this predictive model is that it uses information based on the components of the immune system that are routine laboratory parameters. As mentioned above, the pathophysiology of POD is multifactorial and includes inflammatory elements and the immune system. Another advantage of the CARDEL Index is that it is easy to calculate and cheap because it uses routine, readily available and objective pre-operative parameters.
In one of the cohort studies, Kotfis et al analyzed an association between postoperative delirium after cardiac surgery and elevated preoperative level of glycated hemoglobin.27 The results showed that diabetic patients developed delirium after CABG more often than non-diabetic ones. Elevated pre-operative level of glycated hemoglobin is a risk factor for POD irrespective of diabetes.27
One study showed that postoperative neurological complications may be associated with abnormal preoperative lymphocyte count in patients undergoing carotid endarterectomy.28 This immune system response is associated with an increased number of neutrophils, decreased number of lymphocytes and decreased number of platelets.29 When considering delirium, some degree of neuritis may be manifested by the elevation in neutrophil counts and the neutrophil-to-lymphocyte ratio.20 One study by Egberts et al showed an association between delirium and elevated NLR in elderly patients.24
Although the C-reactive protein is used as an acute phase marker, its increase cannot be substituted for inflammation in delirious patients, as it is not specific in this case. However, Macdonald et al found that serum CRP levels evaluated on admission to the hospital or shortly thereafter were highly predictive of postoperative delirium in acutely ill elderly patients.30 Pfister et al reported that elevated CRP levels were associated with delirium after hip surgery.31
The values of the obtained CARDEL Index were statistically significant (p<0.001). The sensitivity was 0.593 and the specificity was 0.653 in this group. This result indicates that CARDEL Index may be useful for prediction of delirium after cardiac surgery with the use of readily available routine parameters. The possibility of selecting patients with an increased risk of POD development may constitute the basis for the implementation of preventive measures. One of them may be more frequent examination of patients in order to diagnose delirium in the initial phase, which will facilitate treatment. To date, there are no guidelines that would recommend the use of pharmacological therapy as delirium prophylaxis. Prophylaxis using standard non-pharmacological interventions, ie: restoration of senses (hearing aids, glasses), proper hydration and nutrition, adequate pain control, early mobility and allowing early contact with the family and caregivers should be implemented early during postoperative course, especially in patients who are at increased risk of delirium.18
The CARDEL Index is currently the only available predictive index in cardiac surgery. Researchers in other surgical departments around the world have also developed their own predictors of postoperative delirium. Hayashi et al focused on delirium after primary lung cancer surgery. On the basis of a statistical analysis, 3 parameters were identified as responsible for the development of delirium, namely: cerebrovascular disease history (x 2), squamous cell carcinoma and age above 75 years. The values of the estimated risk are as follows: 0 to 1 point denoted low risk, 2 points denoted intermediate risk, scoring 3 to 4 points indicated high risk. In this case, it was also proven that despite the low frequency of delirium (6.7%), it significantly worsened the prognosis and overall survival.32 Due to the presence of a factor specific to lung cancer surgery as one of the parameters, it is not possible to use it in other surgical fields.
This study has some important limitations.33 One of the most important limitations is the performance of the study in the same cardiac surgery center. This could lead to the unknowing duplication of the same errors that may contribute to the development of delirium, and which will not occur in another center. Due to the high frequency, only CABG procedure was selected as a homogeneous group, but this may not necessarily be extrapolated to other cardiac surgery procedures. Additionally, this study was a population study which, in the absence of full knowledge about other possible delirium risk factors, could lead to some inaccuracies. That poses some limitations, however, it is worth implementing further studies in other centers to analysis the CARDEL Index.
Conclusion
Detecting a sensitive and specific marker of delirium can improve patients’ outcome and prognosis. Undoubtedly, the use of biomarkers may aid early identification of patients prone to delirium, shorten its duration and help in identifying pathogenic mechanisms leading to delirium. The variables included in the CARDEL index model, namely advancing age, glycated hemoglobin and platelet-to-WBC ratio are completely uncorrelated and therefore completely independent of each other. The authors conclude that the CARDEL index and included variables can be a helpful tool for prediction delirium in patients after coronary artery by-pass grafting.
Funding
This research received no external funding.
Disclosure
The authors declare no conflicts of interest for this work.
References
1. Pezzella AT, Ferraris VA, Lancey RA. Care of the adult cardiac surgery patient: part I. Curr Probl Surg. 2004;41:458–516. doi:10.1016/j.cpsurg.2004.03.001
2. O’Brien SM, Feng L, He X, et al. The society of thoracic surgeons 2018 adult cardiac surgery risk models: part 2-statistical methods and results. Ann Thorac Surg. 2018;105:1419–1428. doi:10.1016/j.athoracsur.2018.03.003
3. Bowdish ME, D’Agostino RS, Thourani VH, et al. The society of thoracic surgeons adult cardiac surgery database: 2020 update on outcomes and research. Ann Thorac Surg. 2020;109:1646–1655. doi:10.1016/j.athoracsur.2020.03.003
4. American Psychiatric Association. Neurocognitive Disorders. In: Diagnostic and Statistical Manual of Mental Disorders. ISBN 0-89042-555-8. DSM Library; American Psychiatric Association; 2013.
5. Ibrahim K, McCarthy CP, McCarthy KJ, et al. Delirium in the cardiac intensive care unit. J Am Heart Assoc. 2018;7(4):e008568. doi:10.1161/JAHA.118.008568
6. McPherson JA, Wagner CE, Boehm LM, et al. Delirium in the cardiovascular ICU: exploring modifiable risk factors. Crit Care Med. 2013;41:405–413. doi:10.1097/CCM.0b013e31826ab49b
7. Rengel KF, Pandharipande PP, Hughes CG. Postoperative delirium. Press Medicale. 2018;47:e53–e64. doi:10.1016/j.lpm.2018.03.012
8. Kotfis K, Szylińska A, Listewnik M, et al. Early delirium after cardiac surgery: an analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin Interv Aging. 2018;13:1061–1070. doi:10.2147/CIA.S166909
9. Bilotta F, Lauretta MP, Borozdina A, Mizikov VM, Rosa G. Postoperative delirium: risk factors, diagnosis and perioperative care. Minerva Anestesiol. 2013;79:1066–1076.
10. Licker M, Schweizer A, Ellenberger C, Tschopp JM, Diaper J, Clergue F. Perioperative medical management of patients with COPD. Int J COPD. 2007;2:493–515.
11. Wada H, Miyauchi K, Daida H. Gender differences in the clinical features and outcomes of patients with coronary artery disease. Expert Rev Cardiovasc Ther. 2019;17:127–133. doi:10.1080/14779072.2019.1561277
12. Leung JM, Sands LP, Lim E, Tsai LT, Kinjo S. Does preoperative risk for delirium moderate the effects of postoperative pain and opiate use on postoperative delirium? Am J Geriatr Psychiatry. 2013;21:946–956. doi:10.1016/j.jagp.2013.01.069
13. Zubrzycki M, Liebold A, Skrabal C, et al. Assessment and pathophysiology of pain in cardiac surgery. J Pain Res. 2018;11:1599–1611. doi:10.2147/JPR.S162067
14. Swart LM, van der Zanden V, Spies PE, de Rooij SE, van Munster BC. The comparative risk of delirium with different opioids: a systematic review. Drugs Aging. 2017;34:437–443. doi:10.1007/s40266-017-0455-9
15. Rudolph JL, Ramlawi B, Kuchel GA, et al. Chemokines are associated with delirium after cardiac surgery. J Gerontol a Biol Sci Med Sci. 2008;63:184–189. doi:10.1093/gerona/63.2.184
16. Marra A, Kotfis K, Hosie A, et al. Delirium monitoring: yes or no? That is the question. Am J Crit Care. 2019;28:127–135. doi:10.4037/ajcc2019874
17. Marra A, Boehm LM, Kotfis K, Pun BT. Monitoring for delirium in critically ill adults. In: Hughes CG, Pandharipande PP, Ely EW, editors. Delirium: Acute Brain Dysfunction in the Critically Ill. ISBN 978-3-030-25751-4. Cham: Springer International Publishing; 2020:13–25.
18. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263–306. doi:10.1097/CCM.0b013e3182783b72
19. Inoue S, Vasilevskis EE, Pandharipande PP, et al. The impact of lymphopenia on delirium in ICU patients. PLoS One. 2015;10:e0126216. doi:10.1371/journal.pone.0126216
20. Simone MJ, Tan ZS. The role of inflammation in the pathogenesis of delirium and dementia in older adults: a review. CNS Neurosci Ther. 2011;17:506–513. doi:10.1111/j.1755-5949.2010.00173.x
21. Marcantonio ER, Rudolph JL, Culley D, Crosby G, Alsop D, Inouye SK. Serum biomarkers for delirium. J Gerontol a Biol Sci Med Sci. 2006;61:1281–1286. doi:10.1093/gerona/61.12.1281
22. Kotfis K, Bott-Olejnik M, Szylińska A, Listewnik M, Rotter I. Characteristics, risk factors and outcome of early-onset delirium in elderly patients with first ever acute ischemic stroke - a prospective observational cohort study. Clin Interv Aging. 2019;14:1771–1782. doi:10.2147/CIA.S227755
23. Kotfis K, Ślozowska J, Safranow K, Szylińska A, Listewnik M. The practical use of white cell inflammatory biomarkers in prediction of postoperative delirium after cardiac surgery. Brain Sci. 2019;9:1–18. doi:10.3390/brainsci9110308
24. Egberts A, Mattace-Raso FU. Increased neutrophil-lymphocyte ratio in delirium: a pilot study. Clin Interv Aging. 2017;12:1115–1121. doi:10.2147/CIA.S137182
25. Kulaksizoglu B, Kulaksizoglu S. Relationship between neutrophil/lymphocyte ratio with oxidative stress and psychopathology in patients with schizophrenia. Neuropsychiatr Dis Treat. 2016;12:1999–2005. doi:10.2147/NDT.S110484
26. Nashef SAM, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41:734–735. doi:10.1093/ejcts/ezs043
27. Kotfis K, Szylińska A, Listewnik M, Brykczyński M, Ely EW, Rotter I. Diabetes and elevated preoperative hba1c level as risk factors for postoperative delirium after cardiac surgery: an observational cohort study. Neuropsychiatr Dis Treat. 2019;15:511–521. doi:10.2147/NDT.S196973
28. Kotfis K, Biernawska J, Zegan-Barańska M, Żukowski M. Peripheral blood lymphocyte subsets (CD4+, CD8+ T cells, NK cells) in patients with cardiovascular and neurological complications after carotid endarterectomy. Int J Mol Sci. 2015;16:10077–10094. doi:10.3390/ijms160510077
29. Zahorec R. Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102:5–14.
30. Macdonald A, Adamis D, Treloar A, Martin F. C-reactive protein levels predict the incidence of delirium and recovery from it. Age Ageing. 2007;36:222–225. doi:10.1093/ageing/afl121
31. Pfister D, Siegemund M, Dell-Kuster S, et al. Cerebral perfusion in sepsis-associated delirium. Crit Care. 2008;12:R63. doi:10.1186/cc6891
32. Hayashi K, Motoishi M, Sawai S, Horimoto K, Hanaoka J. Postoperative delirium after lung resection for primary lung cancer: risk factors, risk scoring system, and prognosis. PLoS One. 2019;14:e0223917–e0223917. doi:10.1371/journal.pone.0223917
33. Ban JW, Emparanza JI, Urreta I, Burls A. Design characteristics influence performance of clinical prediction rules in validation: a meta-epidemiological study. PLoS One. 2016;11:e0145779. doi:10.1371/journal.pone.0145779
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.