Back to Journals » Clinical Interventions in Aging » Volume 14
Can Serum Nutritional Related Biomarkers Predict Mortality Of Critically Ill Older Patients With Acute Kidney Injury?
Received 10 June 2019
Accepted for publication 9 September 2019
Published 18 October 2019 Volume 2019:14 Pages 1763—1769
DOI https://doi.org/10.2147/CIA.S218973
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Yu Gong,1 Feng Ding,2 Yong Gu2
1Department of Internal Medicine, Division of Nephrology, Shanghai Municipal Eighth People’s Hospital, Shanghai, People’s Republic of China; 2Division of Nephrology, Huashan Hospital, Fudan University, Shanghai, People’s Republic of China
Correspondence: Yu Gong
Department of Internal Medicine, Division of Nephrology, Shanghai Municipal Eighth People’s Hospital, 8 Caobao Road, Shanghai 200235, People’s Republic of China
Tel +86 21 18930718612
Email [email protected]
Background: Critically ill older patients with acute kidney injury (AKI), also referred to as acute renal failure, are associated with high in-hospital mortalities. Preexisting malnutrition is highly prevalent among AKI patients and increases in-hospital mortality rate. This study is to evaluate the predictive power of some serum nutritional related biomarkers predicting the 90 days in-hospital mortality of critically ill older patients with AKI.
Methods: A prospective, observational study was conducted in a university teaching hospital. One hundred and five critically ill older patients with AKI aged 60–95 were enrolled and were divided into survival group (n=44) and non-survival group (n=61) in the light of their final outcomes. Receiver operating characteristic analyses (ROC) were performed to calculate the area under ROC curve (AUC). Sensitivity and specificity of in-hospital mortality prediction were calculated.
Results: Significant differences were found between the survival group and non-survival group of critically ill older patients with AKI. AUC of low density lipoprotein (LDL) and albumin were 0.686 and 0.595, respectively. The asymptotic 95% confidence intervals of LDL and albumin were 0.524–0.820 and 0.488–0.696, respectively. Sensitivity of the 90 days in-hospital mortality prediction of LDL and albumin were 68.71% and 69.09%, respectively. Specificity of 90 days in-hospital mortality prediction of LDL and albumin were 69.23% and 50.0%, respectively.
Conclusion: LDL and albumin did not have sufficient power to predict the 90 days in-hospital mortality of critically ill older patients with AKI. Further research on the association between malnutrition and poor prognosis of critically ill older patients with AKI is needed in the future.
Trial registration: ClinicalTrials.gov identifier: NCT00953992.
Keywords: critically ill older patients, acute kidney injury, mortality, nutritional related biomarker
Plain Language Summary
Critically ill older patients with acute kidney injury (AKI), also as acute renal failure, are associated with high in-hospital mortality. In-hospital mortality prediction is of great importance in guiding treatment and predicting prognosis. This study is to evaluate predictive power of some serum nutritional related biomarkers predicting the 90 days in-hospital mortality of critically ill older patients with AKI. A prospective, observational study was conducted in a university teaching hospital. One hundred and five critically ill older patients with AKI aged 60 to 95 were enrolled and were divided into survival group and non-survival group in the light of their final outcomes. Receiver operating characteristic analyses (ROC) were performed to calculate the area under ROC curve (AUC). Significant differences were found between the survival group and non-survival group of critically ill older patients with AKI. AUC of low density lipoprotein (LDL) and albumin was 0.686 and 0.595, respectively. In this study, it was found LDL and albumin did not have sufficient power to predict the 90 days in-hospital mortality of critically ill older patients with AKI. Further researches on the association between malnutrition and poor prognosis of critically ill older patients with AKI are needed in the future.
Introduction
Acute kidney injury (AKI), previously referred to as acute renal failure (ARF), is a serious clinical state that affects more than 50% of critically ill patients worldwide and is independently related to longer hospital stay.1 AKI represents a frequent complication in older patients with increased mortality.2 Critically ill older patients with AKI are associated with high in-hospital mortalities. In clinical practice, in-hospital mortality prediction is of great importance in guiding treatment and predicting prognosis. Over the past years, several novel serum molecules have been found as biomarkers of early diagnosis of AKI and biomarkers of AKI progression,3–5 but they have not considered the malnutrition state of patients with AKI. Malnutrition is highly prevalent among patients with AKI and increases the in-hospital mortality rate.6 Serum nutritional related biomarkers such as pre-albumin, albumin, and cholesterol are recommended to assess the nutritional status of patients with AKI in accordance with the expert panel convened by the International Society of Renal Nutrition and Metabolism and the American Society of Nephrology.7 Xie et al.8 reported that a higher ratio of C-reactive protein/pre-albumin was associated with mortality of AKI patients and was a valuable predictor for the prognosis. However, there are no studies which have reported the association between malnutrition and poor prognosis of critically ill older patients with AKI. The prognostic relevance of preexisting malnutrition in critically ill older patients with AKI is still unknown. This study is to evaluate the predictive power of some serum nutritional related biomarkers predicting the 90 days in-hospital mortality of critically ill older patients with AKI.
Materials And Methods
A prospective, observational study was conducted in a university teaching hospital. In this study, 189 critically ill patients with AKI of all age groups (from 18 years old to 95 years old) were investigated. Among them, 105 critically ill older patients with AKI aged 60–95 were enrolled into this study according to the newly defined age stratification of older people of the World Health Organization. The critically ill older patients with AKI were divided into a survival group (n=44, mean age=74.0±7.94 years old) and a non-survival group (n=61, mean age=75.98±8.68 years old) in the light of their final outcomes. In the survival group, 31 were men and 13 were women. In the non-survival group, 45 were men and 16 were women. AKI was diagnosed on the basis of the Risk, Injury, Failure, Loss, or End-stage kidney disease criteria (RIFLE),9,10 which standardized the diagnosis of AKI. Patients with AKI caused by glomerulonephritis, post-renal obstruction, and kidney transplantation were excluded. The demographic and outcome characteristics and laboratory features including serum nutritional related biomarkers such as albumin, pre-albumin, total protein, triglyceride, serum total cholesterol (Cho), low density lipoprotein (LDL), and high density lipoprotein (HDL) of all critically ill older patients with AKI were recorded within 24 hours of the patients’ admission of hospital. Three kinds of severity scoring systems, including Sepsis-related Organ Failure Assessment (SOFA), version II of Acute physiology and chronic health evaluation II (APACHE II), and Simplified acute physiology score (SAPS II) counts were also assessed within the first 24 hours following admission. We compared the clinical characteristics, scores of three kinds of severity scoring systems, and laboratory test results including serum nutritional related biomarkers of the survivor group and the non-survivor group of critically ill older patients with AKI. Please see Table 1.
Analyses were performed using IBM SPSS Statistics, Version 20.0 (IBM Inc., Chicago, IL, USA). Continuous variables were analyzed by Student’s t-test and expressed as the mean±standard deviation or median and interquartile range. Categorical variables were analyzed by chi-square test or Fisher’s exact test. p-value<0.05 was considered statistically significant. Receiver operating characteristic (ROC) curves analysis was applied, and ROC curves were drawn up to assess the effectiveness of serum nutritional related biomarkers for the prediction of in-hospital mortality of critically ill older patients with AKI. Then, the area under the ROC curve (AUC) was calculated and analyzed.
All patients provided written informed consent, and this study was conducted in accordance with the Declaration of Helsinki.
Results
There were 105 critically ill older patients with AKI aged 60–95 who were analyzed (76 were male and 29 were female). Significant differences were found between the survival group and the non-survival group in the presence of sepsis, use of dopamine, outcomes, complications, complicated with multiple organ dysfunction syndrome (MODS), assisted breathing with ventilator, LDL, and Scores of SOFA, APACHEII, SAPS II. There were no significant differences found between the survival group and the non-survival group in baseline SCr, length of stay in hospital, length of stay in Intensive Care Unit (ICU), operation history, use of renal replacement therapy (RRT), C-reactive protein, Apolipoprotein-A1, Apolipoprotein-B, Body Mass Index (BMI), RIFLE stage, etc. Analysis of clinical characteristics and laboratory test results including serum nutritional related biomarkers of the survivor group and the non-survivor group of critically ill older patients with AKI is shown in Table 1.
In this study, comparison of the differences of serum nutritional related biomarkers including pre-albumin, albumin, total protein, triglyceride, serum total cholesterol, HDL, LDL between the survivor group and the non-survivor group of critically ill older patients with AKI was conducted. As a result, significant differences (p<0.05) were found in LDL (p=0.025) and albumin (p=0.029) between the survival group and the non-survival group. Comparison of differences of serum nutritional related biomarkers between the survivor group and the non-survivor group of critically ill older patients with AKI is shown in Table 2.
 |
Table 2 Comparison Of Differences Of Serum Nutritional Related Biomarkers Between The Survivor Group And Non-Survivor Group Of Critically Ill Older Patients With Acute Kidney Injury |
Receiver operating characteristic (ROC) curves analysis was conducted in this study. ROC curves of LDL and albumin were drawn up to assess their effectiveness of predicting the 90 days in-hospital mortality of critically ill older patients with AKI. Please see Figure 1. Area under the ROC curve (AUC) of LDL and albumin was calculated, which was 0.686 and 0.595, respectively. The asymptotic 95% Confidence Interval of LDL and albumin was 0.524–0.820 and 0.488–0.696, respectively. In this study, the sensitivity of the 90 days in-hospital mortality prediction of LDL and albumin was 68.71% and 69.09%, respectively. The specificity of the 90 days in-hospital mortality prediction of LDL and albumin was 69.23% and 50.0%, respectively. These results indicated that LDL and albumin did not have sufficient power to predict the 90 days in-hospital mortality of critically ill older patients with AKI. The comparison of effectiveness of LDL and albumin in predicting the 90 days in-hospital mortality of critically ill older patients with AKI is shown in Table 3.
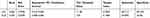 |
Table 3 Effectiveness Of Low Density Lipoprotein And Albumin In Predicting The 90 Days In-Hospital Mortality Of Critically Ill Older Patients With Acute Kidney Injury |
Discussion
AKI is associated with high mortality, particularly in critical ill older patients who are prone to develop AKI. AKI is one of the main causes leading to multiple organ dysfunction syndrome (MODS) and the in-hospital death of critically ill older patients. Critically ill older patients with AKI are usually associated with severe malnutrition and rapid changes in the condition. Accurate in-hospital mortality prediction is of great value in clinical practice. Since evidence-based medical evidence is lacking, the results of some clinical studies of geriatric AKI are not uniform. The assessment of nutrition status is a useful tool for the clinical monitoring of critically ill older patients with AKI. But the underlying diseases, primary disease, complications, accompanied diseases, and renal replacement therapy may interfere in the status of malnutrition of these patients.
Status of malnutrition is associated with higher in-hospital mortality and more complications. Some serum nutritional related biomarkers such as albumin, cholesterol, and pre-albumin have been proved to be useful to predict poor outcomes and higher mortality in AKI patients.11 Recent studies have focused on the relationship between malnutrition and AKI. In the study of Chertow et al.12 it was found that hypoalbuminemia was one of the predictors of death of critically ill patients with AKI due to acute tubular necrosis. Hypoalbuminemia was considered as one of the serum biomarkers of malnutrition of critically ill older patients with AKI. In the study of Li et al.13 it was found that hypoalbuminemia was one of the risk factors of the poor outcomes of renal function in older patients with AKI (≥75 years old) and other risk factors were low pre-albumin level, Body Mass Index (BMI), and more severe AKI stage.In the study of Liu et al,.14 hypoalbuminemia was found to be the major risk coefficient that affected the prognosis of older patients with AKI (80–100 years old) undergoing continuous renal replacement therapy (CRRT), and was related to the turnover of these patients.These results showed that malnutrition is one of the main causes of death and albumin is a predictor for the mortality of critically ill older patients with AKI. In the study of Nie et al.15 it was found that albumin, BMI, total blood count of white blood cell, and total blood count of platelets were the predictors of mortality of AKI patients. Albumin belongs to the biomarkers of malnutrition and total blood count of white blood cell is a biomarker of inflammation. Malnutrition and inflammation may lead to death of critically ill older patients with AKI. The results of the study of Nie et al indicated that albumin can be a predictor of mortality of AKI patients. These results were different from that of our study, which found albumin was associated with in-hospital mortality of critically ill older patients with AKI, but couldn’t effectively predict the 90 days in-hospital mortality. This was because the AKI patients in the study of Nie et al were patients with AKI of all age groups and the AKI patients in our study were critically ill older patients with acute kidney injury aged 60–95. The difference of patient’s age of two studies will inevitably lead to the difference of nutritional status of patients. The factors leading to malnutrition in older patients are more complex than they are in the general population. This is why in this study we found that albumin was associated with the in-hospital mortality of critically ill older patients with AKI but can’t effectively predict the 90 days in-hospital mortality.
Findik et al16 reported that low levels of preoperative serum albumin increase the mortality of patients with severe AKI after isolated coronary artery bypass graft surgery (CABG), which revealed that serum albumin level is an important predictor of the mortality of AKI patients undergoing cardiac surgery. But the target population of our study was critically ill older patients with AKI who have more underlying disease, complications, or accompanied disease which may interfere in the status of malnutrition of patients. At the same time, since these patients were critically ill older patients with AKI, most of them needed renal replacement therapy which could lead to loss of serum albumin of these patients.
In addition, other scholars have studied the clinical value of albumin in predicting mortality in different types of AKI patients, including critically ill patients with septic AKI and critically ill patients requiring CRRT. In the study of Shum et al.17 it was demonstrated that albumin, potassium, and pH value independently predicted 90-day mortality of critically ill patients with septic AKI. Kritmetapak et al.18 found that, in critically ill patients requiring CRRT, serum albumin is a good prognosticator of renal outcome, and dietary protein intake is a good predictor of survival.
In the patients undergoing surgical operation, some serum nutritional index can predict the patients’ mortalities. In the study of Kim et al.19 it was found that a preoperative serum albumin level of <3.8g/dL was independently associated with AKI and mortality in patients undergoing brain tumor surgery. Kim et al.20 found that the serum albumin level <3.0g/dL (within 2 postoperative days) was an independent risk factor for AKI of patients who undergo total knee arthroplasty. The results of these two studies make clear that the low serum albumin level before and after surgical operation is a predictor of the mortality of patients with AKI.
LDL is another serum index of malnutrition which induces dysfunction of the endothelium and causes vascular wall inflammation. In the study of Liu et al.21 it was found that the plasma LDL cholesterol level of patients undergoing percutaneous coronary intervention (PCI) may be helpful to identify the mortality of patients with contrast-induced-AKI (CI-AKI). CI-AKI is a special kind AKI which is induced by contrast medium and is a serious iatrogenic complication that accounts for a significant number of causes of hospital-acquired renal failure, with adverse effects on prognosis. The results showed that LDL was associated with mortality of patients with CI-AKI and a predictor for the mortality.
In the study of Shao et al.22 it was found that hypoalbuminemia in critically ill patients is independently associated with an increased risk of AKI progressing to stage 4 chronic kidney diseases (CKD4).The results suggested that albumin is independently associated with the progression of critically ill patients with AKI. This result is similar to that of our study. It has been proved that pre-existing and/or hospital-acquired malnutrition was identified as an important factor contributing to the persistent high mortality in acutely ill patients with AKI.23 Appropriate dietary management of patients with AKI is essential to improve their long-term prognosis.24 Nutrition management has more important clinical value in critically ill older patients with AKI. Reasonable nutritional therapy is fundamental to reduce the mortality of AKI patients. However, due to the strict control of transfusion volume of patients with AKI, many nutrients can’t be effectively replenished. New techniques of renal replacement therapy, including continuous renal replacement therapy (CRRT), offer the opportunity to adapt nutrition to each individual patient’s need, and there is no reason to reduce nutrition because of fluid restriction, as is often necessary in intermittent hemodialysis.25
There is high heterogeneity in the critically ill older patients with AKI. The cause is not very clear and the mechanism is not found. Critically ill older patients with AKI are associated with high in-hospital mortality rates. Although there is a certain relationship between the malnutrition and poor prognosis, it was found that LDL and albumin can’t predict the 90 days in-hospital mortality of critically ill older patients with AKI in this study.
Conclusion
LDL and albumin did not have sufficient power to predict the 90 days in-hospital mortality of critically ill older patients with AKI. Further research with more patients and centers on the association between malnutrition and poor prognosis of critically ill older patients with AKI is needed in the future.
Abbreviations
AKI, acute kidney injury; ROC, receiver operating characteristic analyses; AUC, area under receiver operating characteristic analyses curve; LDL, low density lipoprotein; RIFLE, risk, injury, failure, loss, or end-stage kidney disease criteria; Cho, serum total cholesterol; HDL, high density lipoprotein; BMI, body mass index; RRT, renal replacement therapy; SOFA, sepsis-related organ failure assessment; APACHE II, version II of Acute physiology and chronic health evaluation II; SAPS II, Simplified acute physiology score; MODS, multiple organ dysfunction syndrome; ICU, intensive care unit.
Ethics Approval And Informed Consent
The protocol for this research project has been approved by the Ethics Committee of Huashan Hospital, Fudan University, and the reference number is 2009-206.
Data Availability
All data generated or analysed during this study are included in this published article.
Acknowledgment
The authors gratefully acknowledge Mrs Fen Zhang for the assistance with medical statistics.
Author Contributions
Yu Gong, Feng Ding, and Yong Gu contributed substantially to the conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hoste EA, Bagshaw SM, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411–1423. doi:10.1007/s00134-015-3934-7
2. Kayatas K, Sahin G, Tepe M, Kaya ZE, Apaydin S, Demirtunç R. Acute kidney injury in the elderly hospitalized patients. Ren Fail. 2014;36(8):1273–1277. doi:10.3109/0886022X.2014.934693
3. Da ER, Yokota LG, Sampaio BM, et al. Urinary neutrophil gelatinase-associated lipocalin is excellent predictor of acute kidney injury in septic elderly patients. Aging and Disease. 2018;9(2):182–191. doi:10.14336/AD.2017.0307
4. Wysocki J, Batlle D. Urinary angiotensinogen: a promising biomarker of AKI progression in acute decompensated heart failure: what does it mean? Clin J Am Soc Nephrol. 2016;11(9):1515–1517. doi:10.2215/CJN.07780716
5. Kota SK, Pernicone E, Leaf DE, Stillman IE, Waikar SS, Kota SB. BPI fold- containing family a member 2/parotid secretory protein is an early biomarker of AKI. J Am Soc Nephrol. 2017;28(12):3473–3478. doi:10.1681/ASN.2016121265
6. Fiaccadori E, Lombardi M, Leonardi S, Rotelli CF, Tortorella G, Borghetti A. Prevalence and clinical outcome associated with preexisting malnutrition in acute renal failure: a prospective cohort study. J Am Soc Nephrol. 1999;10(3):581–593.
7. Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008;73(4):391–398. doi:10.1038/sj.ki.5002585
8. Xie Q, Zhou Y, Xu Z, et al. The ratio of CRP to prealbumin levels predict mortality in patients with hospital-acquired acute kidney injury. BMC Nephrol. 2011;12:30. doi:10.1186/1471-2369-12-30
9. Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P; Acute Dialysis Quality Initiative workgroup.. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):R204–212. doi:10.1186/cc2872
10. Kellum JA, Bellomo R, Ronco C. Definition and classification of acute kidney injury. Nephron Clin Pract. 2008;109(4):c182–187. doi:10.1159/000142926
11. Berbel MN, Pinto MP, Ponce D, Balbi AL. Nutritional aspects in acute kidney injury. Rev Assoc Med Bras. 2011;57(5):600–606.
12. Chertow GM, Lazarus JM, Paganini EP, Allgren RL, Lafayette RA, Sayegh MH. Predictors of mortality and the provision of dialysis in patients with acute tubular necrosis. The Auriculin Anaritide Acute Renal Failure Study Group. J Am Soc Nephrol. 1998;9(4):692–698.
13. Garrido JM, Candela-Toha AM, Parise-Roux D, Tenorio M, Abraira V, Del Rey JM. Impact of a new definition of acute kidney injury based on creatinine kinetics in cardiac surgery patients: a comparison with the RIFLE classification. Interact Cardiovasc Thorac Surg. 2015;20(3):338–344. doi:10.1093/icvts/ivu393
14. Liu S, Cheng QL, Zhang XY, Ma Q, Liu YL, Pan R. Application of continuous renal replacement therapy for acute kidney injury in elderly patients. Int J Clin Exp Med. 2015;8(6):9973–9978.
15. Nie S, Feng Z, Xia L, Bai J, Xiao F, Liu J. Risk factors of prognosis after acute kidney injury in hospitalized patients. Front Med. 2017;11(3):393–402. doi:10.1007/s11684-017-0532-9
16. Findik O, Aydin U, Baris O, Parlar H, Alagoz GA, Ata Y. Preoperative low serum albumin levels increase the requirement of renal replacement therapy after cardiac surgery. The Heart Surgery Forum. 2016;19(3):E123–E127. doi:10.1532/hsf.1577
17. Shum HP, Kong HH, Chan KC, Yan WW, Chan TM. Septic acute kidney injury in critically ill patients - a single-center study on its incidence, clinical characteristics, and outcome predictors. Ren Fail. 2016;38(5):706–716. doi:10.3109/0886022X.2016.1157749
18. Kritmetapak K, Peerapornratana S, Srisawat N, Somlaw N, Lakananurak N, Dissayabutra T. The impact of macro-and micronutrients on predicting outcomes of critically ill patients requiring continuous renal replacement therapy. PloS One. 2016;11(6):e0156634. doi:10.1371/journal.pone.0156634
19. Kim K, Bang JY, Kim SO, Kim S, Kim JU, Song JG. Association of preoperative hypoalbuminemia with postoperative acute kidney injury in patients undergoing brain tumor surgery: a retrospective study. J Neurosurg. 2017;5:1–8. doi:10.1093/neuros/nyw145
20. Kim HJ, Koh WU, Kim SG, et al. Early postoperative albumin level following total knee arthroplasty is associated with acute kidney injury: A retrospective analysis of 1309 consecutive patients based on kidney disease improving global outcomes criteria. Medicine. 2016;95(31):e4489. doi:10.1097/MD.0000000000004864
21. Liu YH, Liu Y, Chen JY, Zhou Y, Chen ZJ, Yu DQ. LDL cholesterol as a novel risk factor for contrast-induced acute kidney injury in patients undergoing percutaneous coronary intervention. Atherosclerosis. 2014;237(2):453–459. doi:10.1016/j.atherosclerosis.2014.10.022
22. Shao M, Wang S, Parameswaran PK. Hypoalbuminemia: a risk factor for acute kidney injury development and progression to chronic kidney disease in critically ill patients. Int Urol Nephrol. 2017;49(2):295–302. doi:10.1007/s11255-016-1453-2
23. Druml W. Nutritional management of acute renal failure. J Ren Nutr. 2005;15(1):63–70.
24. Garrett BM. The nutritional management of acute renal failure. J Clin Nurs. 1995;4(6):377–382.
25. Kierdorf HP. The nutritional management of acute renal failure in the intensive care unit. New Horiz. 1995;3(4):699–707.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


