Back to Journals » Journal of Pain Research » Volume 9
Can consistent benchmarking within a standardized pain management concept decrease postoperative pain after total hip arthroplasty? A prospective cohort study including 367 patients
Authors Benditz A , Greimel F, Auer P, Zeman F, Göttermann A, Grifka J, Meissner W , von Kunow F
Received 11 October 2016
Accepted for publication 10 November 2016
Published 19 December 2016 Volume 2016:9 Pages 1205—1213
DOI https://doi.org/10.2147/JPR.S124379
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Achim Benditz,1 Felix Greimel,1 Patrick Auer,2 Florian Zeman,3 Antje Göttermann,4 Joachim Grifka,1 Winfried Meissner,4 Frederik von Kunow1
1Department of Orthopedics, University Medical Center Regensburg, 2Clinic for anesthesia, Asklepios Klinikum Bad Abbach, Bad Abbach, 3Centre for Clinical Studies, University Medical Center Regensburg, Regensburg, 4Department of Anesthesiology and Intensive Care, Jena University Hospital, Jena, Germany
Background: The number of total hip replacement surgeries has steadily increased over recent years. Reduction in postoperative pain increases patient satisfaction and enables better mobilization. Thus, pain management needs to be continuously improved. Problems are often caused not only by medical issues but also by organization and hospital structure. The present study shows how the quality of pain management can be increased by implementing a standardized pain concept and simple, consistent, benchmarking.
Methods: All patients included in the study had undergone total hip arthroplasty (THA). Outcome parameters were analyzed 24 hours after surgery by means of the questionnaires from the German-wide project “Quality Improvement in Postoperative Pain Management” (QUIPS). A pain nurse interviewed patients and continuously assessed outcome quality parameters. A multidisciplinary team of anesthetists, orthopedic surgeons, and nurses implemented a regular procedure of data analysis and internal benchmarking. The health care team was informed of any results, and suggested improvements. Every staff member involved in pain management participated in educational lessons, and a special pain nurse was trained in each ward.
Results: From 2014 to 2015, 367 patients were included. The mean maximal pain score 24 hours after surgery was 4.0 (±3.0) on an 11-point numeric rating scale, and patient satisfaction was 9.0 (±1.2). Over time, the maximum pain score decreased (mean 3.0, ±2.0), whereas patient satisfaction significantly increased (mean 9.8, ±0.4; p<0.05). Among 49 anonymized hospitals, our clinic stayed on first rank in terms of lowest maximum pain and patient satisfaction over the period.
Conclusion: Results were already acceptable at the beginning of benchmarking a standardized pain management concept. But regular benchmarking, implementation of feedback mechanisms, and staff education made the pain management concept even more successful. Multidisciplinary teamwork and flexibility in adapting processes seem to be highly important for successful pain management.
Keywords: postoperative pain, total hip arthroplasty, pain management concept, benchmarking
Objective
A major factor for patient dissatisfaction, prolonged hospital stays with delayed recovery, and immobility after surgery is severe postoperative pain that is also associated with the development of chronic pain. The 40 surgical procedures with the highest pain scores (median Numerical Rating Scale [NRS] 6 or 7) include 22 orthopedic interventions on the extremities.1 Total hip arthroplasty (THA) is a highly stressful procedure for patients. The worst mean postoperative pain score on the NRS in 2,741 analyzed patients was 4.95 (2.53). THA is in eleventh place of the top 40 surgical procedures.1 In other studies, risk factors for chronic postsurgical pain (CPSP) were chronic preoperative pain, orthopedic surgery, and percentage of time with severe pain on day 1 after surgery.2 The quality of acute postoperative pain management is far from satisfactory,3 despite the availability of a large number of studies on techniques and medication. Pain control in patients after THA is mainly the responsibility of the treating orthopedist.4 We believe that inadequate pain treatment is often caused by organizational problems and lack of sufficient staff education in pain issues.5,6 Not only the physician but the entire health care team should also be responsible for pain management. In particular, nurses, who have much more contact with patients, are important in this respect.7,8 After surgery, the nurse is the main medical contact person for the patient.
The quality of postoperative pain management may be improved by implementing continuous quality improvement (CQI) strategies to detect and rectify insufficient pain management. Key elements of CQI include continuous reassessment and analysis of processes and outcomes.9 Several studies have shown the effectiveness of different types of pain management.10,11 Nonsteroidal anti-inflammatory drugs and lumbar plexus blockage have been shown to decrease postoperative pain scores.12,13
Consequently, we defined our standard for pain management for the perioperative treatment of THA and used the questionnaires of the German-wide project “Quality Improvement in Postoperative Pain Management” (QUIPS) from the first postoperative day onward.
Aim of the study
The study aimed at showing that pain management can be improved by consequent benchmarking of a pain management concept including feedback from and to trained nursing staff and that such improvements subsequently reduce postoperative pain. It was explicitly not the aim of this study to discuss the reasons for our specific pain management concept established by a multidisciplinary pain council.
Methods
Data assessment
The present prospective cohort study included the data of 367 patients who had undergone THA at our university medical center between 2014 and 2015. The data were collected for the QUIPS project, a benchmark initiative for comparing pain outcome parameters among participating hospitals. This project was established and validated in 2005 by one of the coauthors and is well accepted German-wide.9
This project has been supported by the German Society of Anesthesiologists and the German Society of Surgeons.14,15 The project was approved by the ethics committee and the data security board of the Jena University Hospital, Jena, Germany, as well as by the ethics committee of the University of Regensburg. The study is registered in the German Register of Clinical Studies (DRKS) under the number DRKS00006153 (WHO register). The study was carried out in accordance with the ethical standards of the Declaration of Helsinki of 1975. Patients were informed in written form as well as orally by the study personnel, and written informed consent was obtained from all subjects. Participation was voluntary, and withdrawal was possible at any time. Patients older than 18 years who had received THA and were able to communicate were included. Exclusion criteria were 1) patients not present at the ward at the time of data collection; 2) patients who had visitors at the time of data collection; 3) patients who refused to participate in the study; and 4) patients who were sedated or asleep or had cognitive dysfunction. Process data including preoperative, intraoperative, and postoperative variables were collected from the medical records on postoperative day 1.
The validated 15-item questionnaire asked for worst and least pain intensities since surgery using an NRS (NRS: 0 = no pain and 10 = worst pain imaginable).16 A specialized pain nurse visited a random sample of patients on the first postoperative day. Wards to be visited were randomized daily by drawing a number to prevent selection bias. The nurse interviewed the patients and documented postoperative pain treatment as well as analgesia-related complications. To avoid any interviewer–patient interaction bias, the nurse informed the patients that she was working independently from the health care team, that all information or judgment given in the interview would be treated confidentially, and that participation was voluntary. Data were anonymized after the interview.
Pain management concept
The following standardized pain management concept for patients undergoing THA was used for each patient in this study.
One hour before surgery, patients receive oral benzodiazepine premedication followed by spinal cord anesthesia with 4 mL of bupivacaine 0.5% and 0.1 mg of morphine intrathecal. Patients were sedated with propofol during surgery. During the first 12 hours (h) after surgery, the nurse in the intermediate care unit administers 3 mg of piritramide on demand in intervals. Ibuprofen 600 (3×) is used as standard analgesic on a regular daily basis. At the regular ward, oral controlled analgesia (OCA) is administered. Depending on the NRS, patients may receive additional analgesics if required: tramadol 100 mg (40 gtt) with the possibility of a repeat dose after 30 minutes (min) for NRS 3–6 and oxycodone 20 mg and a repeat dose after 1 h for NRS 7–10. In the case of persisting or increasing pain, the nurse will notify the physician. In addition, patients are advised on how to avoid pain by self-activation and are asked to report any occurrence of pain as well as its characteristics at an early stage, also during night time. Cool packs for the affected hip are also provided.
Benchmarking and feedback
A multidisciplinary team of anesthetists, orthopedic surgeons, and nurses implemented a regular procedure of data analysis and internal benchmarking. Beside the main parameters, mean NRS maximum pain, minimum pain, activity-related pain and patient satisfaction, side effects such as nausea, dizziness, tiredness, and postoperative nausea and vomiting (PONV) prophylaxis were evaluated. In addition, functional parameters were analyzed, which means that patients were asked how much pain affected their ability to move in bed, their ability to cough or deep breath, their ability to sleep, and their mood in the last 24 h after surgery. The health care team was informed on any results and suggested improvements. Specially trained pain nurses started to train the other nurses. Nurses also received lessons in general pain management and in pain management required by patients after THA as well as pharmacological training according to our standards in pain management and to the German Guidelines of Pain Management in Nursing by the responsible doctors. Nurses were encouraged to use all treatment options available and were informed about possible risks. In addition, we emphasized the importance of using nonpharmacological therapeutic possibilities such as cooling the wound and different positioning of the patients.
Physicians and nurses were encouraged to improve communication regarding pain management in the regular monthly pain meetings. For example, if a nurse notices a missing order for standard pain medication, she has to call the physician immediately and not just when the pain medication is actually needed. Physicians on the other hand have to inform nurses about special patient requirements beyond the norm.
Furthermore, patients were asked to report pain to the nurses as early as possible and not try to bear the pain. Not only physicians but also nurses have to inform patients several times that they may ask for additional pain medication at any time, particularly during night time, because many patients are reluctant to call the nurse in the middle of the night.5
Statistical methods
Statistical analysis was done with SPSS (IBM SPSS Statistics, Version 23.0; IBM Corporation, Armonk, NY, USA). All single results were divided into intervals of 3 months (quarter of a year) to establish a time line. Metric variables were reported descriptively as mean (standard deviation). Statistical data were not normally distributed. Analyses included the chi-square test and the nonparametric Mann–Whitney U test to compare the effects. Accordingly, the spearman test was used for correlations. Statistical significance was set at p<0.05. With a sample size of n=157 in 2014 compared to n=210 in 2015, we had 80% power to detect an effect size of d=0.35, which can be considered as small.
Results
General results
A total of 367 patients receiving primary THA between January 2014 and December 2015 at our department were included in this study. The mean age was 64.6 years (±10.2), and 82.3% of the patients had an American Society of Anaesthesiologists (ASA) status of 2 or 3. Surgery was conducted by experienced orthopedic surgeons in a center of excellence for arthroplasty. The mean duration of surgery was 70.0 min (±23.5). A total of 73.8% of patients had reported chronic pain for >3 months before surgery in the operated area, with a mean NRS of 6.9 (±1.7; Table 1).
  | Table 1 Demographic data of the 367 included patients Abbreviations: ASA, American Society of Anaesthesiologists; SD, standard deviation; m, male; f, female; NRS, Numerical Rating Scale; min, minutes. |
Pain
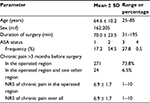
Mean NRS (0–10) was recorded for maximum pain, minimum pain, and activity-related pain (e.g., during movements). At the beginning, the mean maximum pain score was 4.0 (±3.1), which decreased to 3.0 (±2.4) in the second quarter of 2014. The score rose to 3.8 (±2.3) in the third quarter before continuously falling to the minimum of 2.8 (±2.2) in the second quarter of 2015. After that, the score rose insignificantly to 3.0 (±2.1) at the end of the observation period. The overall improvement was 24.4% (Figure 1). The score for minimum pain started at a mean NRS of 0.6 (±1.1) and was low throughout the whole observation period, with a significant overall improvement (Figure 1).
  | Figure 1 Timeline of mean NRS maximum, minimum, and activity-related pain. Abbreviation: NRS, Numerical Rating Scale. |
Activity-related pain overall followed the curves of the other two scores. Starting at a mean of 2.5 (±2.5), the score rose over the first two quarters of 2015 to 3.1 (±1.9). This rise was followed by a continuous decrease down to 0.7 (±0.7) in the third quarter of 2015, before a slight rise to 0.8 (±0.9) at the end of the surveillance period. This overall improvement was also significant (p<0.05; Figure 1).
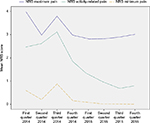
Patient satisfaction was also recorded on an NRS. At the beginning, patient satisfaction was 9.0 (±1.18), rising more or less continuously to 9.8 (±0.4; p<0.05) at the end of the study. Only the third quarter of 2014 showed a small bend in accordance with the other NRS (Figure 2).
  | Figure 2 Timeline of mean NRS patient satisfaction. Abbreviation: NRS, Numerical Rating Scale. |
Side effects and functional parameters
A comparison of the side effects and functional parameters between 2014 and 2015 showed improvement in all parameters. The side effects nausea, tiredness, and dizziness just showed a tendency toward decrease, but the functional parameters were significantly decreased. The decrease in pain affecting the ability to move had significantly dropped from 60.5% to 29.5% (p<0.001) from 2014 to 2015. In 2014, 10.2% of patients had reported their mood being influenced by pain in contrast to only 1.0% in 2015 (p<0.001), and the interference of pain with the ability to sleep from 29.2% to 13.8%, respectively (p<0.001; Table 2).
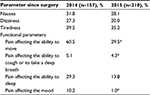  | Table 2 Side effects and functional parameters Note: *p<0.001. |
Comparison among 49 anonymized hospitals
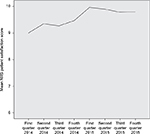
In comparison to the other 48 anonymized hospitals, our clinic was in first place during the 2-year study period from the beginning, showing the lowest mean maximum pain score of 3.13 (±2.27; Figure 3). With regard to patient satisfaction, our hospital also ranked first with a mean NRS of 9.61 (±0.85; Figure 4).
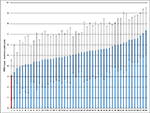  | Figure 3 Comparison of mean NRS maximum pain among 49 anonymized hospitals. Note: The red bar shows our hospital while the blue bars show other hospitals. Abbreviation: NRS, Numerical Rating Scale. |
Discussion
The hypothesis we wanted to show was that pain management can be improved by consistent benchmarking and implementation of a pain management concept including feedback from and to educated staff and that such improvements subsequently reduce postoperative pain and improve patient satisfaction.
In comparison with the other 48 hospitals, our results had already been acceptable at the beginning of the project in 2014, particularly with regard to benchmarking, ranking first. Yet, we tried to even further improve our perioperative pain management and to hold the first rank. Therefore, we intensified our multidisciplinary pain meetings. Our pain meetings are also attended by nurses from the Department of Anesthesia and from the wards. These nurses are able to explain the respective situation of a patient to less experienced nurses. Inexperienced nurses are often afraid of administering oral medication to patients. Due to the lack of a sufficient number of staff, patients sometimes do not receive the required pain medication without delay.17–19 Because the situation of strained human resources could not be helped, we decided to train the existing staff more intensively as described earlier. After the introduction of the concept, first positive effects were seen very soon, for instance, the NRS for maximum and minimum pain decreased from 4.0 and 3.1 to 3.0 and 2.4 at the end of the second quarter 2014. Patient satisfaction also increased from 9.0 (±1.2) to 9.4 (±1.4). Most pain researchers state that the minimally significant difference clinically is an NRS difference of 2. Therefore, on the one hand these results may not be overinterpreted; on the other hand, when initially starting at an NRS of 4, the positive tendency of decreasing to 3.1 can be seen, whereas an improvement of 2 (with 4 as starting point) seems to be not realistic after THA. Only activity-related pain initially rose from 2.5 (±2.5) to 2.6 (±2.3), for which we have no real explanation. All participants in the project were very pleased with the results, so that staff training was set back to normal because the time needed for additional training had been difficult to integrate into clinical routine during the first 6 months. Finding suitable dates for the training sessions was rather difficult on account of the shift work of the nursing staff. However, we failed to take into account that two wards had to be restructured in the fall that also included a replacement of nurses. This may explain a subsequent rise in all pain parameters. Maximum pain scores rose to 3.8 (±2.3), a value that was nearly as high as that at the starting point. Minimum pain scores rose to 0.9 (±1.2) and activity-related pain to 3.1 (±1.9). Patient satisfaction had also slightly decreased.
As mentioned earlier, when discussing the results in our multidisciplinary pain meeting, we found two possible explanations. First, two wards had been restructured. Some nurses had been replaced by new nurses and some retiring graduated nurses by auxiliary staff. Second, many physicians had left, and the newly appointed physicians were not familiar with our pain management concept. Thus, our educational program was intensified again, not as intensive as in the beginning, but driven by staff demand. This measure reversed the negative effect within 3 months, so that a satisfying steady state could be achieved in 2015.
Analyzing the different interventions provided, there was no single intervention which was especially effective in comparison to the others. In our opinion all respects have to be addressed and only work hand in hand.
Regarding the side effects and functional parameters measured in the study, positive effects were found for all parameters. Nausea, dizziness, and tiredness only showed a tendency toward decrease because piritramide is used within the first 12 h in our intermediate care unit. In contrast, scores for pain affecting the ability to move, cough, and breathe as well as a patient’s mood had significantly improved from 2014 to 2015. The less pain patients feel, the less are these parameters affected. Thus, patient satisfaction is increased as observed in our study. Furthermore, these results show that improvements in pain management are not caused by overtreatment (e.g., inadequate opioid or local anesthetic dosing).
Another very important factor is external benchmarking with other hospitals that enables the classification of own results. As part of the QUIPS project,14 we had the opportunity of benchmarking with other hospitals in an anonymized manner. When only considering patients after THA, our clinic ranked first in patient satisfaction and had the lowest maximum pain score.
To maintain this rank, we use a well-balanced education concept. Every new nurse or physician is trained in pain issues as soon as possible to avoid a similar decline as in 2014.
In the field of orthopedics, there are no similar findings or present studies to be compared. However, based on the QUIPS project, similar positive effects have been described in improving pain management after septorhinoplasty20 or comparing pain after cesarean section.15
Although better pharmacological solutions and techniques have been developed over the past years, the findings by Rawal in 1994 held still true in this study.
Thus it appears that the solution of the problems of postoperative pain management lies not so much in the development of new techniques but in development of an organization to exploit existing expertise.6
The difficulty in clinical practice is to maintain this level of quality management and to have sufficient staff for conducting such daily surveys. Cost-effectiveness has become one of the most important factors in hospital management. Successful quality management requires time as well as money for additional staff. Outside Germany, the corresponding project PAIN OUT (www.pain-out.eu) offers a similar tool for feedback and benchmarking.
Although in countries without such a nationwide project, single hospitals or associated hospitals may easily implement benchmarking by comparing the data of different wards within the hospital, only a few hospitals have been able to implement a successful quality management concept for perioperative pain management.5 Wards or hospitals with lower marks could benefit from the experience of those with higher marks.
This study has several limitations. We have no information about the excluded patients. Patients who were not present at the ward or did not want to participate are not included in the registry, which may be a potential source of bias. Furthermore, postoperative pain and pain management were only assessed within the first 24 h. To also observe functional parameters (e.g., mobilization), a longer follow-up should be planned for further studies. Another problem was that patients could only be interviewed Tuesdays to Fridays, because no pain nurse to collect data was available on weekends. Surgery was not conducted on Sundays, so that no patients were available on Mondays, which may also represent some kind of selection bias. Although the results show statistical significance, the clinical significance of pain reduction might be weaker, as the initial level of pain was rather low and patient satisfaction high. However, the decrease in pain affecting the ability to move had significantly dropped from 60.5% to 29.5%, suggesting that reduction in pain intensity was translated into functional improvement of considerable amount. Moreover, in our opinion the results can also be transferred to other fields with a worse start point and an even better clinically significant improvement.
Conclusion
The study showed that – although our existing concept for perioperative pain management after THA had already yielded rather good results beforehand – the implementation of a CQI process further improved results. We have been running this concept in clinical routine for over 2 years. The acceptance in everyday life is high through all professional groups. All parameters of process and outcome quality improved in the first interval of the observation period. After a temporary decrease, results could be maintained on a high level. These results suggest that – next to high-quality pharmacological treatment – interdisciplinary teamwork and benchmarking with direct feedback mechanisms and staff education are also very important for decreasing postoperative pain and increasing patient satisfaction after THA. We think that these findings can also be transferred to other fields of surgery. Yet, after first improvements you may never rest on your laurels.
Acknowledgments
We are grateful to Melanie Schmidt for collecting the data. We also thank Monika Schoell for the linguistic review of our article. This work was supported by the German Research Foundation (DFG) within the funding programme Open Access Publishing.
Disclosure
The authors report no conflicts of interest in this work.
References
Gerbershagen HJ, Pogatzki-Zahn E, Aduckathil S, et al. Procedure-specific risk factor analysis for the development of severe postoperative pain. Anesthesiology. 2014;120(5):1237–1245. | ||
Fletcher D, Stamer UM, Pogatzki-Zahn E, et al. Chronic postsurgical pain in Europe: an observational study. Eur J Anaesthesiol. 2015;32:725–734. | ||
Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin. 2014;30(1):149–160. | ||
Chughtai M, Jauregui JJ, Mistry JB, et al. What influences how patients rate their hospital after total knee arthroplasty? Surg Technol Int. 2016;28:261–265. | ||
Filos KS, Lehmann KA. Current concepts and practice in postoperative pain management: need for a change? Eur Surg Res. 1999;31(2):97–107. | ||
Rawal N. Postoperative pain and its management. Ann Acad Med Singapore. 1994;23(6 suppl):56–64. | ||
Johanson LS. Interprofesssional collaboration: nurses on the team. Medsurg Nurs. 2008;17(2):129–130. | ||
Labbé B, Vaillant C, Commergnat V. Rôle de l’infirmière à la consultation pluridisciplinaire de la douleur. [Nurse’s role in the multidisciplinary consultation for pain]. Rev Infirm. 2003;95:30–31. French. | ||
Meissner W, Ullrich K, Zwacka S. Benchmarking as a tool of continuous quality improvement in postoperative pain management. Eur J Anaesthesiol. 2006;23(2):142–148. | ||
Fikentscher T, Grifka J, Benditz A. Perioperative Schmerztherapie in der Orthopädie. [Perioperative pain therapy in orthopedics]. Orthopade. 2015;44:727–740. German. | ||
Kainzwaldner V, Rachinger-Adam B, Mioc-Curic T, et al. Qualität der postoperativen Schmerztherapie: Evaluation eines etablierten anästhesiologischen Akutschmerzdiensts. [Quality of postoperative pain therapy: evaluation of an established anesthesiology acute pain service]. Anaesthesist. 2013;62(6):453–459. German. | ||
Højer Karlsen AP, Geisler A, Petersen PL, Mathiesen O, Dahl JB. Postoperative pain treatment after total hip arthroplasty: a systematic review. Pain. 2015;156(1):8–30. | ||
Volk T. Neue und evidenzbasierte Aspekte in der postoperativen Schmerztherapie. [New and evidence-based aspects of postoperative pain therapy]. Orthopade. 2008;37(10):953–954. German. | ||
Meissner W, Mescha S, Rothaug J, et al. Quality improvement in postoperative pain management: results from the QUIPS project. Dtsch Arztebl Int. 2008;105(50):865–870. | ||
Marcus H, Gerbershagen HJ, Peelen LM, et al. Quality of pain treatment after caesarean section: results of a multicentre cohort study. Eur J Pain. 2015;19(7):929–939. | ||
Rothaug J, Weiss T, Meissner W. Externe Validität der schmerzbedingten Funktionsbeeinträchtigung: Messen wir, was wir messen wollen? [External validity of pain-linked functional interference: are we measuring what we want to measure?]. Schmerz. 2012;26(4):396–401. German. | ||
Cabilan CJ, Eley R, Hughes JA, Sinnott M. Medication knowledge and willingness to nurse-initiate medications in an emergency department: a mixed-methods study. J Adv Nurs. 2016;72(2):396–408. | ||
Sawhney M, Maeda E. Nursing knowledge and beliefs regarding patient-controlled oral analgesia (PCOA). Pain Manag Nurs. 2013;14(4):318–326. | ||
Riemondy S, Gonzalez L, Gosik K, Ricords A, Schirm V. Nurses’ perceptions and attitudes toward use of oral patient-controlled analgesia. Pain Manag Nurs. 2016;17(2):132–139. | ||
Wittekindt D, Wittekindt C, Schneider G, Meissner W, Guntinas-Lichius O. Postoperative pain assessment after septorhinoplasty. Eur Arch Otorhinolaryngol. 2012;269(6):1613–1621. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.