Back to Journals » International Journal of Women's Health » Volume 8
Can a community-based maternal care package in rural Ethiopia increase the use of health facilities for childbirth and reduce the stillbirth rate?
Authors Atnafu H, Belete Z, Kinfu H, Tadesse M, Amin M, Ballard K
Received 13 January 2016
Accepted for publication 20 April 2016
Published 18 August 2016 Volume 2016:8 Pages 421—428
DOI https://doi.org/10.2147/IJWH.S104160
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Habtamu Atnafu, Zelalem Belete, Hirut Kinfu, Mebkyou Tadesse, Mohammed Amin, Karen D Ballard
Hamlin Fistula Ethiopia, Addis Ababa Fistula Hospital, Addis Ababa, Ethiopia
Objective: To measure the impact of a maternal health package on health facility delivery and stillbirth rates.
Methods: This is a cross-sectional study in Ethiopia where a maternal package was integrated into eight health centers across three regions. The package included trained midwives with a mentoring program, transport for referral, and equipment and accommodation for the midwives. Ten health centers without the package but in the same districts as the intervention centers and eight without the package in different districts were randomly selected as the comparison groups. Women living in the catchment areas of the 26 health centers, who delivered a baby in the past 12 months, were randomly selected to complete a face-to-face survey about maternal health experiences.
Results: The maternal package did not significantly affect the stillbirth or facility delivery rates. Women were positively influenced to deliver in a health facility if their husbands were involved in the decision concerning the place of birth and if they had prior maternal experience in the health center. Barriers to delivering in a health facility included distance and ability to read and write.
Conclusion: Women served by health centers with a maternal health package did not have significantly fewer stillbirths and were not more likely to deliver their babies in a health facility. Husbands played an important role in influencing the decisions to deliver in a health facility.
Keywords: maternal health, institutional delivery, stillbirth, predictive factors, Ethiopia, global health
Introduction
Over the first decade of the 21st century, Ethiopia reported little change in maternal health, with a maternal mortality ratio between 673 and 676 per 100,000 live births1,2 and a stillbirth rate between 4.2% and 7.9%.3 Given that maternal and fetal outcomes have been shown to improve when there is a skilled birth attendant present at delivery,4,5 much effort has gone into reducing the 90% home delivery rate within the country.2
Although efforts to increase facility delivery rates in Ethiopia have been underway for many years, both government and nongovernmental organizations have recently stepped up their efforts to increase access to skilled birth attendants through greater numbers of community-based midwives and new health facilities and significant developments in road infrastructure and transport availability. Despite this, in 2013, just 23.1% of women had a skilled birth attendant present at the time of delivery.6 Moreover, while there have been improvements in maternal and fetal outcomes, it has been estimated that the current maternal mortality ratio remains relatively high at 420 per 100,000 live births7 and the stillbirth rate is estimated at 2.6%.8
Measuring the effectiveness of specific interventions aimed at increasing the uptake of maternal services is a complex process as the environment is susceptible to constant change, making it difficult to identify the precise mechanisms underlying any change in behavior or outcome. Indeed, a recent systematic review of 42 studies evaluating the effectiveness of maternal health interventions in resource-limited countries,9 including one Ethiopia-based study, recognized the complex nature of determining cause and effect but concluded that programs with multiple interventions tended to be more effective. Such a multi-pronged approach underlies the principles of health services strengthening,10 whereby interventions seek to augment critical components of a health system. For example, interventions aimed at improving maternal and neonatal health would consider the need for universal access to maternal care, the need to ensure that staff were skilled to provide high-quality care, that there was adequate emergency referral system in place, and that there was appropriate configuration of the maternal and neonatal health services across all levels of care.
Hamlin Fistula Ethiopia (HFE) is a charitable organization that has been working in Ethiopia since 1974. In addition to offering free comprehensive fistula care, the organization used a health systems strengthening approach in the provision of a maternal care package into government-run rural health centers across the country. The government health centers are staffed by health officers, midwives, and nurses, and the maternal care is free of charge. The maternal health package provided by HFE includes two Bachelor of Science (BSc)-trained midwives who were originally selected from rural areas and trained at the College of Midwifery in Addis Ababa. Once qualified, they are supported to provide high-quality maternal care in a rural health center. They are given free accommodation either within the health center grounds or nearby so that they are able to provide 24-hour cover. An experienced midwife mentor will, on average, visit them once a month to provide continuing professional development and provide advice over the phone when needed. The midwife mentor also acts as a mechanism for strengthening links across all levels of maternal care within the district and continues to support the midwives for the duration of their appointment at the health center.
The package also includes a monthly mobile phone credit allowance to ensure finance does not prohibit the midwives from seeking advice or referring women to higher-level care. An ambulance is on call 24 hours a day to provide transport from the health center to hospital when required. HFE also supplies any necessary equipment and drugs for maternal care. For example, delivery beds, sphygmomanometers, solar equipment for lighting, and vacuum delivery packs. HFE currently provides the health package in 27 health centers across Ethiopia.
The aim of this study was to determine whether the Hamlin maternal health package increased the uptake of health facilities for delivery and reduced the stillbirth rate.
Materials and methods
This is a cross-sectional community-based study based in three zones of Ethiopia where the maternal package had been in operation for a minimum of 2 years: East Hararghe (East Ethiopia), South Gondor, and West Gojjam (North Ethiopia). Women in these three zones, who gave birth in the 12 months prior to the data collection, were the source population. The study was designed to collect data from women served by: 1) health centers with maternal package, 2) health centers without the package but within the same district as the supported centers, and 3) health centers outside of the intervention district. Although women can access maternal care from more than one health center, the distances between them is far and transport is limited. It is therefore possible to identify the households that are served by the different health centers.
The primary outcome measure was stillbirth rate, as this was considered to be an objective measure that reasonably reflects the ability of the maternal package to increase facility deliveries and provide high-quality maternal care. The sample size was therefore based on a reduction in stillbirths among women served by health centers with the maternal package compared to those without the package. The stillbirth rate in the Amhara and Oromia regions, where the study was based, is 46 stillbirths per 1,000 births.2 We considered that a reduction to 25 stillbirths per 1,000 births would reflect a clinically relevant change. A 95% confidence interval (CI) and 80% power to reject the hypothesis was used and the sample size increased by applying a design effect of 1.2. This resulted in a need for 1,457 study participants in each of the three groups and a total sample size of 4,371 women who had delivered a baby in the previous 12 months.
Within the three zones, there were eight health centers with the maternal health package, and the households served by these health centers were sampled to obtain the intervention group. The two comparison groups were obtained by sampling households served by a random selection of ten health centers within the same districts as the intervention centers and a random selection of eight health centers in different districts to the intervention health centers. After identifying the 26 health centers, four or five health posts linked to the health centers were selected according to the distance from the health center, providing one near, two of medium distance, and one remote health post. This provided a total of 116 health posts. Finally, 28,000 households served by each of the selected health posts were then randomly chosen for surveying (Figure 1). Since 3.5% of the population is pregnant each year, this provides a potential sample of 4,900 women who have delivered a baby in the past 12 months. Allowing for a 10% error in data collection enables us to achieve our desired sample size of 4,373.
  | Figure 1 Sampling process. |
Following ethical approval from the Amhara and Oromia health bureaus, data were collected through the use of a piloted, structured questionnaire, which asked questions about obstetric and maternal care experiences as well as demographic details. It was translated into local languages and following training, administered face-to-face by 237 health extension workers working in the villages. Before participating in the study, women were read a participant information sheet and asked to sign or use their fingerprint to consent to taking part in the study.
During the data collection period, the research team visited all of the research sites to ensure that the survey was being administered properly and was also being administered to the selected households. Over this time, 5% of the administered questionnaires were re-administered by the research team to verify data quality.
Data were checked for completeness and consistency and then cleaned, coded, and entered into SPSS version 20 (IBM Corporation, Armonk, NY, USA) for analysis. Women who had reported having had eclampsia or a severe antepartum bleed were classified as having “a complication during pregnancy” and women who had reported having experienced a prolonged labor of more than 24 hours or a ruptured uterus were classified as having a “complicated labor”.
Median differences in parity were determined using a Kruskal–Wallis test. Group differences (three groups) in stillbirth rate, institutional delivery rates, and antenatal care (ANC) uptake were determined using a Pearson’s chi-square test. Following this, univariate analysis of factors that might be associated with institutional delivery was undertaken. Finally, bivariate binary logistic analysis, using a forward conditional model, was undertaken to determine which factors (including the presence of the maternal care package) were predictive of institutional delivery. Potential factors were included in the analysis if the P-value was 0.20 or less in the univariate analysis. Odds ratios with 95% CIs were used to consider the strength of the factors in predicting institutional delivery. Data were collected from May 2014 to December 2014.
Results
A total of 4,442 correctly completed surveys were available for analysis, of which, 1443 were completed by women served by health centers with the maternal package, 1524 by women served by health centers in the same district as the intervention health centers, and 1373 by women served by health centers outside of the intervention district. The mean age of women was 28.5 (standard deviation [SD] 5.9) years. The vast majority (97.7%; n=3,046) of women in West Gojjam and South Gondor were orthodox Christians, and the vast majority (98%; n=1,216) in East Hararghe were Muslims. Almost all (96.6%; n=4,288) of the women were married, and 94% (n=4,164) were either housewives or farmers or undertook a combination of both of these occupations.
Most women (78%; n=3,387) were unable to read or write and just 714 (16.5%) had completed primary education and 236 (5.5%) had completed secondary education. Over half (55%; n=2,458) of the women were unaware of their monthly household income, and 1,072 (24%) reported their monthly income to be below 900 Ethiopian Birr (45 USD). Most women (83.2%; n=3,693) were multiparous.
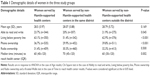
As illustrated in Table 1, the three study groups were of a similar age and equal proportions owned a radio. The women served by the health centers with the maternal package were similar in other demographic features to women served by nonintervention centers outside of the district. However, a greater proportion of women served by nonintervention health centers in the same district were living further away from the health center, fewer women had a phone, were able to read and write, and were living below the poverty line, compared with the other two groups.
Stillbirths
The stillbirth rate within the total population was 2.1% (n=95). Women served by health centers with the maternal package had a stillbirth rate (1.8%; n=27) similar to those served by centers without the package in the same district (1.9%; n=30), but there was a nonsignificant (P=0.063) greater proportion (2.7%; n=38) of stillbirths in women served by nonintervention health centers outside the districts when compared with women living within the districts where the packages were provided.
Women served by health centers with the maternal package had a lower parity (median 4; interquartile range [IQR] 2–5) than women served by centers without the package in the same district (median 5; IQR 2–5) and those centers outside the district (median 5; IQR 2–5) (P<0.001).
The stillbirth rate was higher (2.8%; n=44) in grand multiparous women (≥5) than in those with a parity of 1–4 (1.8%; n=51) (P=0.023).
Facility deliveries
A greater proportion (43.4%; n=647) of women served by centers with the package delivered their baby in a health facility compared to those who were served by nonintervention centers in the same district (39%; n=611) and those served by nonintervention centers outside of the district (29.7%; n=413) (P<0.001). Fewer women served by the nonintervention centers outside the district attended for ANC (49.4%; n=679) compared to those served by centers with the maternal package (56.9%; n=821) and those without the maternal package but in the same district as the intervention centers (64.4%; n=982) (P<0.001).
The univariate analysis revealed that several factors influenced the uptake of institutional delivery (Table 2). In particular, having a husband involved in decisions about where to deliver and prior experience of the maternal services at a health facility experience were strongly associated with the use of health facilities for delivery of the baby born over the preceding 12 months.
Finally, the multiple covariate logistic regression model revealed seven factors that were independently predictive of a health facility delivery: 1) husband’s involvement in the decision about delivery place; 2) uptake of ANC; 3) previously delivered in a health institution; 4) ability to read and write; 5) being primigravid; 6) possession of a radio; and 7) having a complicated labor. Two further factors were found to reduce the chances of delivering in a health facility: 1) having to walk for 1 or more hours to reach a health facility and 2) being served by health centers outside the intervention district (Table 3).
  | Table 3 Adjusted risk estimates for delivering in a health facility |
As illustrated in Table 3, husband’s involvement in the decision about where to deliver the baby and prior experience of the health facility maternal care services remained very strong predictors for a health facility delivery. While women served by health centers with the maternal health package were not more likely to deliver in a health facility, women served by health centers outside of the intervention districts were less likely to deliver their baby in a health facility.
Discussion
While instinctively, we expect interventions that aim to improve maternal care will lead to significantly better outcomes for the mother and baby, the complex nature of health care environments often leads to incongruous results. Our study revealed that a maternal health package containing multiple interventions, when integrated into community-based health centers, did not significantly decrease the stillbirth rate. We also found that women served by the health centers with the maternal package had a lower parity than women served by centers without the package, which should have put them at a reduced risk of stillbirth.
When other factors were accounted for, the package also did not increase the use of health facilities for childbirth. We did, however, find that the health centers in the same district as those with a maternal package had similar outcomes, whether they had a maternal health package or not and centers outside of the district did less well. Indeed, there was a nonsignificant reduction in stillbirths and a significant increase in facility deliveries among women served by health centers in the district where the intervention was placed compared to those served by health centers outside of the intervention districts.
It is difficult to fully explain these findings, but it is possible that interventions introduced into one health center may have a positive effect on nearby centers. Equally, it may be that there is a “district” effect, brought about by factors unrelated to the maternal health package. Ideally, we would want to identify whether the stillbirth occurred during the antenatal period or during labor, particularly as a higher rate of intrapartum stillbirths is suggestive of poorer quality health center care. Although we were unable to obtain this information, we have reported elsewhere11 that women delivering in a health center are more likely to report an obstructed labor of more than 24 hours or other obstetric emergency. It is likely, therefore, that a significant proportion of women experience the stillbirth prior to reaching the health center.
Although the maternal health package did not independently increase facility delivery rates, many factors were found to be important predictors of a woman delivering in a health facility. In particular, a husband’s involvement in decisions about the delivery place had a strong positive influence on delivering in a health facility, with women being nearly seven times more likely to deliver their babies in a health facility when compared to those whose husband was not involved in the decision about the delivery place. Other studies have also identified the positive role of husbands in encouraging women to deliver in a health facility,12,13 highlighting the need for a family approach to health promotion messages about the value of the maternal services.
Similar to other studies,14–16 we found that women who attended for ANC were over three times more likely to deliver their babies in a health facility compared with women who did not have ANC. While this reinforces the importance of encouraging women to attend for ANC, it is also worth noting that over half of the women receiving ANC still deliver their babies at home.11,17 Future research to identify barriers to facility delivery in women having ANC would be beneficial.
Similar to other studies,18 we observed that primigravid women were more likely to deliver in a health facility than multiparous women. This is encouraging as we also found that women who had previously delivered a baby in a health facility were more likely to deliver future babies in the facility. If primigravid women are increasingly accepting the health messages about the importance of childbirth with a skilled birth attendant, it is likely that their future births will also take place in a health facility.
Our results also add to the vast body of literature,2,13,19 showing that distance from a health facility and ability to read and write influence the uptake of a health facility delivery. While there has been a steady rise in the literacy rate over the past 5–10 years,2 it is important to recognize that there are many generations of women who have not attended school. These women need to be supported in accessing health information and making choices about their maternal care. The Ethiopian government has increased the number of community-based health facilities, but more needs to be done to ensure that women are aware of the maternal health services offered within these facilities. Access to the services also needs to be improved, allowing women to reach a facility for full ANC and within good time when labor commences.
Our study is limited by not taking a prospectively random approach to the selection of the intervention and nonintervention health centers. Unfortunately, for logistic reasons, randomized control studies are rarely carried out in sub-Saharan African countries where the health care arena frequently undergoes change. Indeed, in a review of 42 maternal health interventional studies,9 less than a third had a control group and just 17% of all studies were randomized. Our study was therefore limited by our intervention centers being selected prior to our random selection of the nonintervention centers. In addition, around the time of our study, the impact of several national improvements in the provision of maternal care was beginning to materialize,20 and many of these improvements in service mirrored aspects of our maternal package intervention. For example, our package included easily accessible transport for laboring mothers, something that was subsequently introduced at a national level. We also provided two additional midwives in each of the intervention centers and soon after, the increased numbers of government-trained midwives were ready to be placed in centers across the country. Nevertheless, our package still contained additional features such as a mentoring program and necessary equipment, which along with the rest of the package of care was tested for effectiveness.
Conclusion
Measuring the effectiveness of maternal health interventions is complex but essential if limited resources are to be used proficiently. Although we found that our maternal package did not significantly alter the stillbirth and facility delivery rates, husbands’ involvement in the decision about the delivery place and prior experience of the maternal services were important factors positively influencing the health facility delivery, and distance and education were barriers to accessing services. Future maternal health interventions need to take a family centered approach and access to the services need to be further facilitated.
Acknowledgments
The authors are very grateful to Johnson & Johnson for the funding they provided to HFE, which allowed us to undertake this work. Many people contributed toward the research, including the health extension workers who collected the data; the health center staff who assisted in data verification; volunteers Greg Morris, Clara Cantalapiedra, and Jacinta Evans who entered the data; Harriet Andrews, Camilla Ducker, and Ellen Pieterse who assisted with the data verification and training of data collectors. Last but not least, the authors are grateful to the women who kindly allowed us into their homes and their generosity in giving us the time to ask them personal questions.
Author contributions
Karen Ballard and Habtamu Atnafu contributed to the design of the study, the data collection, data entry, data analysis, and writing of the manuscript. Zelalem Belete contributed to the design of the study and writing of the manuscript. Hirut Kinfu, Mebkyou Tadesse, and Mohammed Amin contributed to the data collection and writing of the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Central Statistical Agency. Ethiopia Demographic & Health Survey 2005. Addis Ababa, Ethiopia: Central Statistical Agency. | ||
Central Statistical Agency. Ethiopia Demographic & Health Survey 2011. Addis Ababa, Ethiopia: Central Statistical Agency. | ||
Yifru B, Asres B. Perinatal mortality trends in Ethiopia. Ethiop J Health Sci. 2014;(24):29–40. | ||
Khan K, Wojdyla D, Say L, Gulmezoglu AM, Van Look PFA. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367(9516):1066–1074. | ||
Aminu M, Unkels R, Mdegela M, Utz B, Adaji S, van den Broek N. Causes of and factors associated with stillbirth in low- and middle-income countries: a systematic literature review. BJOG. 2014;121(S4):141–151. | ||
Ministry of Health. Health and Health-Related Indicators 2012/13. Addis Ababa, Ethiopia: Ministry of Health; 2014. Available from: http://www.moh.gov.et/documents/26765/0/Health+and+Health+Related+Indicators+2005+E.C/1b5b2a9f-a960-4024-8d92-519195364023?version=1.0. Accessed September 7, 2015. | ||
WHO, The World Bank, United Nations Population Division. Trends in Maternal Mortality: 1990 to 2013. Geneva: WHO; 2014. | ||
WHO, The World Bank, United Nations Population Division. Trends in Maternal Mortality: 1990 to 2010. Geneva: WHO; 2012. | ||
Nyamtema A, Urassa D, van Roosmalen J. Maternal health interventions in resource limited countries: a systematic review of packages, impact and factors for change. BMC Preg Childbirth. 2011;11:30. | ||
Ergo A, Eichler R, Koblinsky M, Shah N. Strengthening Health Systems to Improve Maternal, Neonatal and Child Health Outcomes: A Framework. Washington, DC: USAID; 2011. Available from: http://www.mchip.net/sites/default/files/HSS%20and%20MNCH%20Framework_final.pdf. Accessed March 12, 2016. | ||
Ballard K, Belete Z, Kinfu H, Tadesse M, Amin M, Atnafu H. The impact of antenatal and intra-partum care on the stillbirth rate among 4,441 women in rural Ethiopia. Int J Gynecol Obs. 2016. EPub 2016 Mar 12. | ||
Fikrie A, Dimissie M. Prevalence of institutional delivery and associated factors in Dodota Woreda (district), Oromia regional state, Ethiopia. Reprod Health. 2012;(9):33. | ||
Shah R, Rehfuess E, Maskey M, Fischer R, Bhandari P, Delius M. Factors affecting institutional delivery in rural Chitwan district of Nepal: a community-based cross-sectional study. BMC Preg Childbirth. 2015;15:27. | ||
Pervin J, Moran A, Rahman M, et al. Association of antenatal care with facility delivery and perinatal survival: a population-based study in Bangladesh. BMC Preg Childbirth. 2012;12:111. | ||
Mengesha Z, Biks G, Ayele T, Tessema G, Koye D. Determinants of skilled attendance for delivery in Northwest Ethiopia: a community based nested case control study. BMC Public Health. 2013;13:130. | ||
Karkee R, Lee A, Khanal V. Need factors for utilization of institutional delivery services in Nepal: an analysis from Nepal Demographic and Health Survey, 2011. BMJ Open. 2014;4(3):e004372. | ||
Yifru B, Asres B. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop J Health Sci. 2014;24(Suppl):93–104. | ||
Devasenapathy N, George M, Jerath S, et al. Why women choose to give birth at home: a situational analysis from urban slums of Delhi. BMJ Open. 2014;4:e004401. | ||
Abeje G, Azage M, Setegn T. Factors associated with institutional delivery service utilization among mothers in Bahir Dar city administration, Amhara region: a community based cross sectional study. Reprod Health. 2014;11:22. | ||
Ethiopian Ministry of Health (Ethiopia). Health Sector Development Program IV 2010/11-2014/15. Addis Ababa, Ethiopia; 2010. Available from: http://www.nationalplanningcycles.org/sites/default/files/country_docs/Ethiopia/ethiopia_hsdp_iv_final_draft_2010-2015.pdf. Accessed September 7, 2015. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.