Back to Journals » International Journal of General Medicine » Volume 8
Burning feet in polycythemia vera – peripheral sensorimotor axonal neuropathy with erythromelalgia
Authors Wollina U
Received 8 December 2014
Accepted for publication 5 January 2015
Published 2 February 2015 Volume 2015:8 Pages 69—71
DOI https://doi.org/10.2147/IJGM.S78848
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Uwe Wollina
Department of Dermatology and Allergology, Academic Teaching Hospital Dresden-Friedrichstadt, Dresden, Germany
Abstract: Polycythemia vera is a rare myeloproliferative disease. Cutaneous symptoms are uncommon. We report about a 72-year-old female patient with JAK2V617F-positive polycythemia who developed peripheral sensorimotor axonal neuropathy and erythromelalgia. Possible causes and treatment are discussed.
Keywords: bone marrow diseases, myeloproliferative diseases, JAK2 mutations, burning sensations, peripheral neuropathy
Introduction
Polycythemia vera (PV) is a hematologic disease that is characterized by accumulation of phenotypically normal red blood cells, white blood cells, and platelets. The disease is diagnosed by a combined approach of laboratory investigations, bone marrow histology, and detection of characteristic mutations.1,2 A mutation of the JAK2 gene is found in 98% of PV patients and clearly distinguishes PV from secondary polycythemia.2 The typical JAK2V617F mutation induces a loss of inhibitory activity of the JH2 pseudokinase part on the JH1 of Janus kinase 2 (JAK2). This results in enhanced activity of JH1 kinase activity of JAK2. Mutated hematopoietic stem cells thereby become hypersensitive to their appropriate hematopoietic growth factors, resulting in myeloproliferation.2
PV is a rare disease. The annual incidence has been calculated to be from 0.01 to 2.61.3
Classical maintenance treatment consists of hydroxyurea and phlebotomy.4,5 More recently, Janus kinase inhibitors have become available, with promising results in clinical trials.6 Antithrombotic drugs are used to decrease the risk of thromboembolic events.5 Cutaneous manifestations are uncommon in PV. We report a case of peripheral sensorimotor axonal neuropathy combined by erythromelalgia.
Case report
A 72-year-old woman presented with a history of burning feet that started about one year earlier. On examination there was a livid red discoloration on the soles of the feet (Figure 1). Her medical history was remarkable for a diagnosis of PV in April 2011. The diagnosis was based on elevated hemoglobin, hematocrit, and red cell mass. JAK2V61F and PRV1 (polycythemia vera rubra-1) mutations were detected cytogenetically, excluding secondary erythrocytosis.
  | Figure 1 Palmar erythema with slight edema. Toes are involved as well. |
Routine laboratory investigation demonstrated normal blood glucose, transaminases, creatinine, thyroid hormones, and folate. Elevated were hematocrit (53%), leukocyte (11.4 Gpt/L), thrombocytes (410 Tpt/L), and serum vitamin B12 (920 pg/mL) levels. Paraproteinemia was excluded by electrophoresis. Vibratory testing with a tuning fork at 128 Hz was slightly decreased symmetrically on the distal part of the legs in a stocking-like pattern. Pinprick and proprioception were also decreased distally. The Achilles tendon reflex was absent. Dorsiflexion of the feet was weak, but patellar reflexes were present. Muscle hypotrophy was not obvious.
Previous treatment had consisted of antithrombotic drugs, acetylsalicylic acid and angrelide, and the cytoreductive compound hydroxycarbamide. Due to noncompliance, all medical treatments had to be stopped shortly after initiation. Thereafter, she received regular phlebectomy only. We suspected a diagnosis of erythromelalgia in combination with peripheral sensorimotor axonal neuropathy of the legs. The patient was referred for further diagnostics to the neurologist (Table 1).
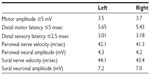  | Table 1 Electrophysiological findings |
Discussion
PV is a hematological disorder. Pruritus is the most frequent cutaneous symptom, with a negative impact on quality of life. A recent study in more than 400 PV patients reported aquagenic pruritus in 68.3% of patients. PV-associated pruritus does not respond to antihistamines, but can be treated with aspirin and paroxetine.7 Other cutaneous symptoms such as leg ulcers, livedo racemosa, and erythromelalgia are rare, and only case reports and case series have been published.8–10
Erythromelalgia can be divided into a primary and secondary subtype. In the present case, we refer to secondary erythromelalgia. Clinically, erythromelalgia is characterized by a triad of erythema, increased local temperature, and burning pain. Histologically, erythromelalgia demonstrates capillary proliferation, endothelial swelling, perivascular edema, and sparse lymphocytic infiltrates.10 Redness and burning pain were present in our patient but elevated temperature was missing. Symptoms were unresponsive to aspirin but the patient was also noncompliant.
Our patient had additional signs of chronic symmetrical peripheral neuropathy with motor and sensory symptoms. We discussed the possibility of drug-induced peripheral neuropathy. Hydroxyurea-induced erythromelalgia is a very rare event.11 Hydroxycarbamide has been reported to cause peripheral neuropathy when it is combined with didanoside and stavudine (as in human immunodeficiency virus). The effect is dose-dependent. Such combined medication was never given to the patient.
Hydroxycarbamide 600 mg/day has been considered safe.12 The patient had taken hydroxycarbamide for no longer than 8 weeks, which makes this a rather unlikely cause. Acetylsalicyclic acid and angrelide are not known to cause neuropathy.
Therefore, we considered symmetrical peripheral sensorimotor axonal neuropathy as the underlying cause. Diagnosis of peripheral neuropathy in general follows a stepwise algorithm. In patients with signs and symptoms of chronic polyneuropathy and a typical clinical phenotype in association with a known cause of peripheral neuropathy, like diabetes or alcoholism, additional blood tests and electrophysiological studies are not informative. If there is no known cause, ancillary studies should initially aim at the identification of diabetes, alcohol misuse, or renal failure, all of which were negative in our patient. In the remaining patients, electrophysiological studies are recommended (Table 1).13
PV-associated neuropathy has been classified in group five of the peripheral neuropathies in the 1993 Amsterdam guideline.13 PV can cause neurological symptoms such as headaches, dizziness, and fatigue. None of these were present in our patient. On the other hand, PV is rarely associated with peripheral sensorimotor axonal neuropathy. The underlying mechanism is hypoxia due to blood hyperviscosity and abnormal platelet aggregation. Timely recognition of this symptom and more frequent phlebotomy may prevent severe damage.14 On the other hand, no relationship between severity of peripheral axonal neuropathy and duration of PV disease was found.14 Unfortunately, sensorimotor axonal neuropathy is irreversible.14–16
Disclosure
The author reports no conflicts of interest in this work.
References
Alvarez-Larrán A, Ancochea A, et al. WHO-histological criteria for myeloproliferative neoplasms: reproducibility, diagnostic accuracy and correlation with gene mutations and clinical outcomes. Br J Haematol. 2014;166:911–919. | |
Roda P, Ferrari A, Tang X, et al. Determination of accuracy of polycythemia vera diagnoses and use of the JAK2V617F test in the diagnostic scheme. Ann Hematol. 2014;93:1467–1472. | |
Titmarsh GJ, Duncombe AS, McMullin MF, et al. How common are myeloproliferative neoplasms? A systematic review and meta-analysis. Am J Hematol. 2014;89:581–587. | |
Dingli D, Tefferi A. Hydroxyurea: the drug of choice for polycythemia vera and essential thrombocythemia. Curr Hematol Malig Rep. 2006;1:69–74. | |
Assi TB, Baz E. Current applications of therapeutic phlebotomy. Blood Transfus. 2014;12 Suppl 1:75–83. | |
Rosenthal A, Mesa RA. Janus kinase inhibitors for the treatment of myeloproliferative neoplasms. Expert Opin Pharmacother. 2014;15:1265–1276. | |
Siegel FP, Tauscher J, Petrides PE. Aquagenic pruritus in polycythemia vera: characteristics and influence on quality of life in 441 patients. Am J Hematol. 2013;88:665–669. | |
Shanmugam VK, McNish S, Shara N, et al. Chronic leg ulceration associated with polycythemia vera responding to ruxolitinib (Jakafi(®)). J Foot Ankle Surg. 2013;52:781–785. | |
Shimizu A, Tamura A, Ishikawa O. Livedo racemosa as a cutaneous manifestation of polycythemia vera. Eur J Dermatol. 2006;16:312–313. | |
Bakkour W, Motta L, Stewart E. A case of secondary erythromelalgia with unusual histological findings. Am J Dermatopathol. 2013;35:489–490. | |
Moore RD, Wong WM, Keruly JC, McArthur JC. Incidence of neuropathy in HIV-infected patients on monotherapy versus those on combination therapy with didanosine, stavudine and hydroxyurea. AIDS. 2000;14:273–278. | |
Butler D, Nambudiri VE, Nandi T. Hydroxyurea-associated acral erythema in a patient with polycythemia vera. Am J Hematol. 2014;89:931–932. | |
Rosenberg NR, Portegies P, de Visser M, Vermeulen M. Diagnostic investigation of patients with chronic polyneuropathy: evaluation of a clinical guideline. J Neurol Neurosurg Psychiatry. 2001;71:205–209. | |
Mihalj M, Titlić M, Bonacin D, Dogaš Z. Sensomotor axonal peripheral neuropathy as a first complication of polycythemia rubra vera: a report of 3 cases. Am J Case Rep. 2013;14:385–387. | |
Poza JJ, Cobo AM, Martí-Massó JF. Peripheral neuropathy associated with polycythemia vera. Neurologia. 1996;11:276–279. | |
Poncelet AN. An algorithm of evaluation of peripheral neuropathy. Am Fam Physician. 1998;57:755–764. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
