Back to Journals » Vascular Health and Risk Management » Volume 15
Blood pressure control in treated hypertensive Middle Eastern patients: a post hoc analysis based on JNC8 definitions
Authors Alhaddad IA , Hamoui O , Hammoudeh A , Mallat S
Received 27 September 2018
Accepted for publication 5 December 2018
Published 6 March 2019 Volume 2019:15 Pages 35—46
DOI https://doi.org/10.2147/VHRM.S188981
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Harry Struijker-Boudier
Imad A Alhaddad,1 Omar Hamoui,2 Ayman Hammoudeh,3 Samir Mallat4
1Cardiovascular Department, Jordan Hospital, Amman, Jordan; 2Cardiology Department, Clemenceau Medical Center, Beirut, Lebanon; 3Cardiology Department, Istishari Hospital, Amman, Jordan; 4Department of Internal Medicine, Nephrology Division, American University of Beirut Medical Center, Beirut, Lebanon
Background: Long-term blood pressure (BP) control is challenging due to the asymptomatic nature of hypertension and poor treatment adherence among patients. We conducted a post hoc analysis to assess “target BP” attainment and maintenance and to identify their associated factors in a sample of hypertensive Middle Eastern patients.
Methods: We previously conducted an observational study between May 2011 and September 2012 to assess antihypertensive treatment adherence and its determinants in a sample of 1,470 hypertensive patients in Lebanon and Jordan. The study consisted of 3 visits: at baseline, 3 months, and 6 months, where BP control, health-related quality of life, and treatment adherence were assessed. This post hoc analysis of data from the ADHERENCE study examined BP control in terms of target attainment at 3 months and 6 months, and target maintenance at 6 months in treatment-eligible patients as well as the determinants of BP control including the impact of the new JNC8 (Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure) guideline on treatment eligibility and target BP attainment in these patients.
Results: Based on JNC8 definitions, our results revealed that 81.2% of patients achieved BP control at 6 months. At 3 months, 62.2% achieved BP control; of those, only 57.5% maintained BP control till 6 months. Factors associated with higher BP target attainment at 3 months were higher educational level, new hypertension diagnosis, older age, and lower waist circumference, systolic BP, and diastolic BP at baseline. Factors associated with higher BP target attainment at 6 months were Lebanese nationality, new hypertension diagnosis, absence of chronic kidney disease, lower systolic BP at baseline, reaching BP target at 3 months, and having a BP target of <150/90 mmHg.
Conclusion: Older age, higher education levels, recent hypertension diagnosis, early achievement of target BP, and having milder disease at baseline were associated with better BP control. Moreover, JNC8 guideline reduced the number of treatment-eligible patients and increased BP target attainment.
Keywords: blood pressure control, JNC8 guidelines, JNC7 guidelines, adherence, Lebanon, Jordan, hypertension
Introduction
Hypertension is the leading cause of cardiovascular morbidity and mortality worldwide.1 According to recent estimates, hypertension affects one billion individuals worldwide and is deemed responsible for nine million deaths every year.2 The prevalence of uncontrolled hypertension ranges between 45% and 81% in hypertensive patients in different countries.3,4 Epidemiological studies linked uncontrolled hypertension to increased rates of ischemic heart disease and stroke.5,6 Likewise, several meta-analyses have shown that lowering blood pressure (BP) reduces the risk of major cardiovascular events in younger and older adults.7,8
Despite the advances in antihypertensive drugs, achieving long-term BP control is challenging owing to the asymptomatic nature of the disease and lack of adherence among patients.9 Poor treatment adherence increases the risk of hypertension complications and the financial burden on healthcare systems.10 Variable rates of treatment non-adherence were reported among elderly outpatients, ranging between 29% and 59%.11 In the same vein, we previously conducted an observational study on 1,470 hypertensive patients in Lebanon and Jordan to measure their adherence to antihypertensive treatment (the ADHERENCE study).12 Our results have shown that only 55.9% of evaluated patients reported adequate adherence to antihypertensive medications. Furthermore, we identified several factors associated with non-adherence, including poorer quality of life, being divorced/widowed, and having uncontrolled BP at end of study, while older age was associated with better medication adherence.12
Several guidelines have been developed to guide hypertension treatment in terms of treatment eligibility (initiation) and target BP in different patient populations. In 2003, the JNC7 (Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure) guideline was released, recommending that the target of BP control should be <140/90 mmHg in all hypertensive patients except those with diabetes or chronic kidney disease (CKD), for whom the target should be <130/80 mmHg.9 However, in the following years, several clinical trials were published, highlighting the need for a simpler and less strict classification of BP.13,14 In 2014, the JNC8 (Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure) guideline was published, driven by a systematic review of clinical trial evidence, and stated that BP control target should be <140/90 mmHg for all patients except those older than 60 years with no diabetes or CKD, in whom the target should be <150/90 mmHg.15
Using the same data of the ADHERENCE study, we performed this post hoc analysis to study “target BP” attainment and maintenance and the factors affecting them, including the impact of the new JNC8 guideline on treatment eligibility and target BP.
Methods
The primary aim of the ADHERENCE study was to assess antihypertensive treatment adherence and its determinants. The detailed methodology of the study including study design and data collection is described in the published article by Alhaddad et al.12 The study was of an observational nature, performed between May 2011 and September 2012 in Jordanian and Lebanese hospitals and private clinics. It collected data for the 1,470 enrolled adults who were newly diagnosed with hypertension or have been uncontrolled after 6 months or more of antihypertensive treatment. The study was conducted in accordance with the Declaration of Helsinki. All participants signed a written informed consent before study entry and the study protocol was approved by the Institutional Review Boards of the American University of Beirut and the Jordan Hospital.
Patients’ data were collected at three separate visits: at baseline (inclusion) and two follow-up visits at 1–3 and 6 months. Collected data included patient sociodemographic, clinical, and disease-related characteristics. Adherence was assessed using Morisky, Green & Levine Scale16 and health-related quality of life was assessed using The Hypertension Quality of Life Questionnaire (MINICHAL).17 Blood pressure and anthropometric measurements and cardiovascular score (CVS) were assessed at every visit. In the previous analysis, treatment eligibility and BP targets were defined based on the JNC7 criteria. However, in the current analysis, the determination of treatment eligibility and BP targets were based on the JNC8 guideline, ie, the cutoff limits for treatment eligibility were systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg for all patients, except those ≥60 years of age with no diabetes or CKD diagnosis for whom the limits were SBP ≥150 mmHg or DBP ≥90 mmHg.
Outcome measures
Based on the JNC8 criteria, target BP was defined as SBP <140 mmHg and DBP <90 mmHg in all patients except those ≥60 years of age with no diabetes or CKD diagnosis for whom the target was set at SBP <150 mmHg and DBP <90 mmHg. The primary outcome in the current analysis was the percentage of patients reaching and maintaining target BP at month 6 (the patient is on-target at the 3- and 6-month visits). Secondary outcomes in this analysis included 1) the percentage of subjects reaching target BP at 3 and 6 months; 2) the determinants of reaching target BP at each visit; 3) the determinants of maintaining target BP (based on analyzing only patients who were on-target at the 3-month visit); and; 4) the impact of the new JNC8 guideline on treatment eligibility and target BP attainment in hypertensive patients.
Statistical analyses
Statistical analyses were performed using the statistical software SPSS (version 17.0; SPSS Inc., Chicago, IL, USA). Mean values and standard deviations were used to describe continuous variables, whereas percentages were used to describe categorical variables. Categorical data were compared using the Pearson chi-squared test, while continuous data were compared using the Student’s t-test. The level of statistical significance was set at p-value <0.05. MANOVA test was used to analyze the change in mean measurements between different time points (P-value based on Wilk’s Lambda). Moreover, we used multivariate logistic regression analysis to determine the effects of individual factors on BP control; variables which had a p-value <0.1 in univariate comparisons were included in the models. Adjusted odds ratios and their 95% confidence intervals were reported. Hosmer and Lemeshow test was used to assess the goodness-of-fit of the regression models.
Results
Descriptive analyses
According to JNC8 guideline’s classification, 1,424 hypertensive patients (96.9%) were considered as treatment eligible and were thus included in this study, while 98.0% of patients were considered as treatment eligible in our previous analysis that was based on JNC7 guideline’s classification. Of the total study population, 822 patients (57.7%) were male. The mean age of our population was 54.2±12.1 years. The majority of patients (79.8%) were married and 617 patients (43.3%) were newly diagnosed with hypertension, while 807 patients (56.7%) had uncontrolled hypertension. As for comorbidities, 28.4% were diabetic and 8.6% had CKD. The baseline characteristics of treatment-eligible patients are detailed in Table 1.
  | Table 1 Baseline characteristics of treatment-eligible patients Abbreviations: CAD, coronary artery disease; CHF, congestive heart failure; CV, cardiovascular; CVD, cardiovascular disease. |
According to the JNC8 criteria, 83% of patients had a BP target <140/90 mmHg and 17% of patients had a BP target <150/90 mmHg. The cardiovascular disease (CVD) risk categories at baseline and follow-up visits are detailed in Table 2. Based on Morisky, Green & Levine Scale, 37.6% of subjects were classified as adherent at follow-up 1 (FU1), while 55.7% were classified as adherent at follow-up 2 (FU2). The mean MINICHAL score decreased from 14.2±8.7 at baseline to 9.8±8.1 at FU2 (Table 2).
At FU1, 847 patients (62.2%) reached their BP target and 515 patients (37.8%) did not. At FU2, 1,107 patients (81.2%) reached their BP target and 256 patients (18.8%) did not; only 76.8% of patients reached their BP target at FU2 based on our previous classification (JNC7). Seven hundred and sixty-seven patients (57.5%) reached their target at month 3 and maintained it till month 6 (Table 3).
The mean systolic/diastolic BP significantly decreased from 160.4/96.6 mmHg at baseline to 128.4/80.0 mmHg at FU2 (P<0.001). Moreover the mean weight was significantly reduced from 85.4 kg at baseline to 83.5 kg at FU2 (P<0.001) and the mean waist circumference (WC) significantly decreased from 98.3 cm at baseline to 96.6 cm at FU2 (P<0.001). The descriptive details of blood pressure and anthropometric measurements at different visits are illustrated in Table S1.
Subjects reaching BP target at FU1
On the univariate level, no significant difference was found between patients who reached BP target at FU1 and those who did not in terms of gender (P=0.572), nationality (P=0.073), marital status (P=0.276), work status (P=0.371), health insurance (P=0.100), diabetes (P=0.537), or co-morbidities (P=0.891). The mean age of patients who reached BP target at FU1 was greater than that of those who did not (P=0.006). Of patients newly diagnosed with hypertension, 67.1% reached BP target at FU1 of compared to 58.4% of patients with uncontrolled hypertension (P=0.001). Moreover, we observed significant differences (P<0.05) in baseline weight, WC, SBP and DBP between patients who reached BP target at FU1 and those who did not. A detailed comparison between patients who reached BP target at FU1 vs those who did not is illustrated in Table S2. Elderly patients with target (<150/90 mmHg) had the highest rate of reaching BP target at FU1 (72.5%) compared to patients with target (<140/90 mmHg) (60.1%) (P<0.001) (Table S3).
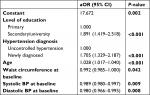
After adjustment for covariates, only education level, hypertension diagnosis, age, WC at baseline, SBP at baseline, and DBP at baseline remained associated with target achievement at FU1 on the multivariate level (Table 4).
Subjects who reached BP target at FU2
No significant difference was found between patients who reached BP target at FU2 and those who did not in terms of gender (P=1.000), age (P=0.131), marital status (P=0.231), work status (P=0.945), health insurance (P=0.870), nor co-morbidities (P=0.353). Lebanese patients had a higher rate of reaching BP target at FU2 (86.5%) as compared to Jordanian patients (76.2%) (P<0.001). Diabetes and CKD were associated with significantly lower rates of target achievement (P=0.004 and P=0.006 respectively). Eighty-six percent of patients with newly diagnosed hypertension reached their BP target at FU2 as compared to 77.6% of patients with uncontrolled hypertension (P<0.001). Patients who reached BP target at FU2 had significantly lower WC at baseline and FU1, SBP at baseline and FU1, and DBP at FU1 (P<0.001) (Table S4).
Among patients with different BP targets at baseline, the highest rate of BP target achievement at FU2 was in patients with target <150/90 mmHg (P=0.003). The highest rate of patients reaching BP target at FU2 was found among patients who reached BP target at FU1 (91.9%) and in those who had relatively lower CVS at FU1 (P<0.001). As expected, treatment adherence at FU1 was associated with higher rates of BP target achievement at FU2 (P=0.034) (Table S5).
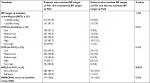
After adjustment for covariates, only nationality, hypertension diagnosis, CKD, BP target at baseline, SBP at FU1, and reaching target at FU1 remained associated with target achievement at FU2 on the multivariate level, where patients who reached BP targets at FU1 were 3.5 times more likely to reach their targets at FU2 than those who did not. Likewise, patients of Lebanese nationality, new hypertension diagnosis, no CKD, or BP target of <150/90 mmHg were twice as likely to achieve BP target at FU2. The detailed results of the logistic regression analysis are listed in Table 5.
Subjects reaching BP target at FU1 and maintaining BP target at FU2
Only nationality and treatment adherence at FU1 were significantly associated with target maintenance till FU2. Further details on the association between target maintenance and patient characteristics are shown in Tables S6 and S7. After adjustment for covariates, nationality and hypertension diagnosis were associated with target maintenance on the multivariate level (Table 6).
Discussion
The current work is a post hoc analysis on the same raw data of the already-published ADHERENCE study; however, patients were reclassified as treatment eligible/non-eligible and BP targets were re-evaluated based on the new guideline (JNC8). This has caused differences in the results because we were dealing with two different populations and assessing the new population based on criteria which are different from those used in the previous evaluation.
This study is the first to analyze the impact of changes in recommendations for management of hypertension on treatment eligibility and target achievement in a population of Middle Eastern patients. Our findings indicated that increased rates of target BP attainment on the short term (FU1) were associated with older age, higher education levels, recent hypertension diagnosis and having lower SBP and DBP at baseline. However, the presence of hypertension comorbidities was not associated with a significant worsening of control rates. These data are in discordance with several observational studies, which reported that the existence of hypertension comorbidities is associated with poor medication adherence and challenging BP control.18,19 An interesting observation in our study is that the mean weight and WC of enrolled patients were significantly lower at FU2 visit than at baseline and FU1 visit. Along with the higher number of patients achieving BP control at FU2, these data confirm the value of lifestyle modification and weight reduction in BP control.20,21
In addition, we found that reaching the BP target and reporting of adequate treatment adherence at FU1 visit were significantly associated with better control at FU2 visit. This is in accordance with the former Lebanese I-PREDICT study, which showed that early control of BP was associated with good control maintenance. The study also concluded that the presence of diabetes was a predictor of poor control;22 in our study, diabetes was significantly associated with BP target attainment at the second evaluation visit (6 months).
Of note, we detected significant differences between Lebanese and Jordanian patients in terms of target BP attainment and maintenance. For example, a significantly higher number of Lebanese patients achieved target BP at FU2 and maintained such attainment till FU2, compared to Jordanian patients. This confirms data in the literature that suggests that BP control varies between different cultures and raises the need for cross-cultural studies to elucidate the reasons underlying these differences.23
Two groups of patients have been affected by the new JNC8 recommendation in our study: 1) Those who were treatment-eligible under the JNC7 guideline and are no longer considered for antihypertensive treatment (1.1% in the current analysis); and 2) those who were considered off-target based on JNC7 classification and were reclassified as on-target under the same treatment based on JNC8 classification (4.4% in this study). There is probably another group of patients who achieved target control using strict antihypertensive regimens under the JNC7 guideline and are now considered for less strict regimens or no treatment under the JNC8 recommendations. However, the assessment of these patients was not in the scope of our study.
A meta-analysis of data of 1 million adults showed that when BP increases above 115/75, the risk of CVD increases without threshold.24 In 2016, the Systolic Blood Pressure Intervention Trial (SPRINT) was published, reporting that ambulatory patients >75 years of age should be treated to a SBP target of less than 120 mmHg.25 In 2017, the American College of Cardiology and the American Heart Association recommended a target for BP control that is less than 130/80 mmHg.26 These recent data may contribute to a revision of the JNC8 guideline in the near future.
Our study had some limitations. For a start, enrolled patients in this study were recruited from hospitals and private clinics, limiting the generalizability of our findings to the general population. Second, the diagnosis of diabetes and CKD was based on self-reporting, which may undermine the prevalence of both conditions in our sample. Moreover, one limitation of this study was the performance of single office blood pressure measurement at each visit instead of ambulatory blood pressure monitoring, which could interfere with the reproducibility of measurements. Other limitations stem from the cross-sectional design of our study, such as the failure to account for changes in BP parameters over the long term. Due to limitations inherent to observational studies, our findings are limited to association and causality may not be inferred.
Conclusion
To recapitulate, our study showed that older age, higher education levels, recent hypertension diagnosis, early achievement of target BP, and having milder disease (lower SBP or DBP) at baseline were associated with better BP control. Moreover, the JNC8 guideline reduced the number of treatment-eligible patients, while it increased the number of patients who achieved BP target under the same therapeutic regimens.
Acknowledgment
This study was supported by funding from AstraZeneca.
Disclosure
The authors report no conflicts of interest in this work.
References
Kearney P, Whelton M, Reynolds K, Muntner P, Whelton P, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. | ||
World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013. Geneva: World Health Organization; 2013. | ||
Wolf-Maier K, Cooper RS, Kramer H, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43(1):10–17. | ||
Centers for Disease Control and Prevention (CDC). Vital signs: awareness and treatment of uncontrolled hypertension among adults-United States, 2003–2010. MMWR Morb Mortal Wkly Rep. 2012;61:703–709. | ||
Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. | ||
Boehme AK, Esenwa C, Elkind MS. Stroke risk factors, genetics, and prevention. Circ Res. 2017;120(3):472–495. | ||
Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. | ||
Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet. 2001;358(9290):1305–1315. | ||
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. | ||
Lee GK, Wang HH, Liu KQ, Cheung Y, Morisky DE, Wong MC. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS One. 2013;8(4):e62775. | ||
Stewart RB, Caranasos GJ. Medication compliance in the elderly. Med Clin North Am. 1989;73(6):1551–1563. | ||
Alhaddad IA, Hamoui O, Hammoudeh A, Mallat S. Treatment adherence and quality of life in patients on antihypertensive medications in a Middle Eastern population: adherence. Vasc Health Risk Manag. 2016;12:407–413. | ||
JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008;31(12):2115–2127. | ||
Ogihara T, Saruta T, Matsuoka H, et al. Valsartan in elderly isolated systolic hypertension (VALISH) study: rationale and design. Hypertens Res. 2004;27(9):657–661. | ||
James PA, Oparil S, Carter BL, et al. Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. | ||
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. | ||
Roca-Cusachs A, Badia X, Dalfó A, et al. [Relationship between clinical and therapeutic variables and health-related quality of life in patients with hypertension. MINICHAL Study]. Med Clin (Barc). 2003;121(1):12–17. Spanish. | ||
Wong ND, Lopez VA, L’Italien G, Chen R, Kline SE, Franklin SS. Inadequate control of hypertension in US adults with cardiovascular disease comorbidities in 2003–2004. Arch Intern Med. 2007;167(22):2431–2436. | ||
Ogedegbe G. Barriers to optimal hypertension control. J Clin Hypertens (Greenwich). 2008;10(8):644–646. | ||
Appel LJ, Champagne CM, Harsha DW, et al; Writing Group of the PREMIER Collaborative Research Group. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289(16):2083–2093. | ||
Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998;279(11):839–846. | ||
Mallat SG, Samra SA, Younes F, Sawaya MT. Identifying predictors of blood pressure control in the Lebanese population - a national, multicentric survey – I-PREDICT. BMC Public Health. 2014;14(1):1142. | ||
Rich MW, Gray DB, Beckham V, Wittenberg C, Luther P. Effect of a multidisciplinary intervention on medication compliance in elderly patients with congestive heart failure. Am J Med. 1996;101(3):270–276. | ||
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. | ||
SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–2116. | ||
Whelton PK, Carey RM, Aronow WS, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–e248. |
Supplementary materials
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.