Back to Journals » Clinical Ophthalmology » Volume 10
Bleb related infections: clinical characteristics, risk factors, and outcomes in an Asian population
Authors Yap ZL, Chin YC, Ku JYF, Chan TK, Teh G, Nongpiur ME, Aung T, Perera SA
Received 3 August 2016
Accepted for publication 15 September 2016
Published 18 November 2016 Volume 2016:10 Pages 2303—2309
DOI https://doi.org/10.2147/OPTH.S118809
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Zhu Li Yap,1,2 You Chuen Chin,1 Judy Yu-Fen Ku,1 Tat Keong Chan,1,2 Gillian Teh,1,2 Monisha Esther Nongpiur,2,3 Tin Aung,1,2 Shamira A Perera1–3
1Singapore National Eye Centre, Singapore; 2Singapore Eye Research Institute, Singapore; 3Duke NUS Graduate Medical School, Singapore
Purpose: Comparison of the demographic, ocular, systemic and microbiological characteristics of eyes with bleb related infection (BRI) and bleb related endophthalmitis (BRE).
Methods: Retrospective chart review of patients with BRI from January 1996–July 2013. Identification done via the center’s longstanding endophthalmitis audit, BRI audit and laboratory database identifying all conjunctival swabs from blebs. Blebitis was defined as anterior segment inflammation with mucopurulent material in or around the bleb, with anterior chamber cells but no hypopyon. BRE was defined by the presence of hypopyon or vitreous inflammation.
Results: Twenty-nine patients with blebitis and 10 with BRE were identified. Mean age of subjects (n=39) was 68.4 (±13.3) with a preponderance of men (74.4%) and Chinese ethnicity (74.4%). BRE patients were 10.7 years older than blebitis patients (P=0.026). 28 (71.8%) subjects had primary open angle glaucoma. The presenting intraocular pressure (IOP) dropped in blebitis but almost doubled in BRE (P=0.011) compared to average preinfective IOP. Two weeks after treatment, IOPs in both groups returned to close to preinfective levels. Subjects with blebitis more often had an avascular bleb (88.0%) while those with BRE trended toward a moderately vascular bleb (50%). The distribution of causative microorganisms between the groups was similar.
Conclusion: Our study indicates that risk factors are similar in both groups even though the visual outcome and clinical course, in the form of IOP findings and bleb vascularity, can diverge significantly. The decreased IOP in blebitis subjects represents objective evidence of subclinical leaks or bleb sweating.
Keywords: bleb related endophthalmitis, blebitis, post-trabeculectomy
Introduction
All surgeries come with an attendant risk of infection, glaucoma filtration surgery being no exception. Literature cites the follow up adjusted incidence (number of events per patient-year) of bleb related infection (BRI) lying in the range of 0.4%–6.9% with a follow up ranging from 1.7 years to >8.5 years.1–10 While more recent papers are reporting significantly lower incidence rates of BRI, they are still significantly higher than the reported incidence of acute postoperative endophthalmitis after other types of intraocular surgery.
In general, BRI after glaucoma filtering surgery can be divided into localized blebitis and bleb related endophthalmitis (BRE); BRE being a potentially devastating sight-threatening condition with poor visual prognosis. The current premise is that blebitis precedes and leads to BRE if left untreated. While nearly all studies agree that diabetes, inferior bleb position, bleb leak and bleb manipulation are strong risk factors for BRI, dispute exists over others, such as age and gender.6,8,9,11–13 It is therefore pertinent that our study examines the risk factors in our population and their impact on the development of BRI.
Intraoperative use of anti-fibrotic agents mitomycin C (MMC) and 5-fluorouracil (5-FU) is becoming standard adjunctive therapy globally, as they reduce scarring and failure rates.4 Unfortunately, their use is associated with spontaneous bleb leaks and thus also BRI; with some large scale studies estimating a worrying 5-year complication risk of up to 23%.1,14 At the Singapore National Eye Centre, all trabeculectomies are performed with adjunctive anti-fibrotic agents, MMC being the preferred choice. Rates of BRE after using MMC have been reported at 1.1%–3.2%.2,4,15,16 While Mochizuki et al’s study demonstrated similar BRI rates of 1.3% and 1.1% with 5-FU and MMC, respectively.4 However, studies have not been able to demonstrate if either anti-fibrotic confers a greater risk for BRI.6,16,17
Previous reviews have mostly focused on BRE17–20 and largely overlooked blebitis, with the last review adequately discussing both BRIs published more than 5 years ago.21
Our study compares demographic, ocular, systemic and microbiological characteristics of eyes with BRI and BRE.
Materials and methods
Approval from the Centralised Institutional Review Board of SingHealth was obtained and this retrospective, single-center study was conducted in adherence with the tenets of the Declaration of Helsinki. The review board did not require that written informed consent be obtained from the patients, as this was a retrospective study and all data was anonymous.
Patient notes were identified for review by the following means: (1) Patients who had been flagged as having BRE by our center’s endophthalmitis audit from January 1996–July 2013; (2) post-trabeculectomy patients with a history of a conjunctival swab on the microbiology laboratory database from April 2004–July 2013; (3) patients who had been labeled as having BRI in the glaucoma department’s internal audit, available from January 2006–July 2013.
All cases diagnosed by the treating glaucoma consultant as having blebitis or BRE, whether culture positive or negative, were included in the study. Blebitis was defined as anterior segment inflammation with mucopurulent material in or around the bleb, usually with anterior chamber cells but no hypopyon. If a hypopyon or any vitreous inflammation was present, it was categorized as BRE.1,2,5,16
Data recorded included baseline characteristics: demographic data, systemic disease(s), type of glaucoma, coexisting eye disease and previous eye surgeries. Surgical data: date of surgery and surgical procedure details (bleb location, forniceal- or limbal-based approach, use of anti-metabolites and timing of application, postoperative procedures and complications [eg, bleb leak, revision or manipulations]).
Visual acuity at presentation and after resolution of the infection, intraocular pressure (IOP) (throughout the infection period), treatment and functionality of the bleb after infection, and bleb morphology at presentation were also recorded.
Data on management of the infection included: time from onset of symptoms to presentation to the hospital, time before initial antibiotic treatment, type of antibiotic treatment, whether vitrectomy was performed, conjunctival swabs in all patients and vitreous culture results where applicable. In addition, the time from surgery until onset of the infection was analyzed.
Statistical analysis was performed using the statistical package IBM SPSS Statistics for Windows (Version 21.0; IBM Corp, Armonk, NY, USA). Differences between the 2 groups were examined using the independent sample Student’s t-test for continuous variables and chi square tests for categorical variables. An appropriate Bonferroni correction (α/number of variables evaluated) was applied to correct for the number of variables that were evaluated.
Results
Baseline characteristics
Of the 39 patients identified as having BRIs, 29 patients had blebitis and 10 had BRE. The baseline characteristics of subjects are shown in Table 1. The mean age ± standard deviation of all subjects (n=39) was 68.4±13.3 with 29 (74.4%) men and 29 (74.4%) Chinese. There was no significant difference in gender and ethnicity between those with blebitis compared with BRE. BRE patients were on average 10.7 years older than blebitis patients (P=0.026). The majority of subjects had primary open angle glaucoma (n=28, 71.8%) with 10 (25.6%) subjects having had previous cataract surgery. 18 (46.2%) subjects also had a coexisting eye condition such as lid or corneal disease. Among the comorbidities examined, subjects with BRE were more likely to be diabetic (60% vs 27.6%) but this did not reach significance (P=0.12).
Surgical procedure
Several factors relating to the trabeculectomy procedure were evaluated (Table 2). Majority of the subjects had a superotemporal bleb (n=15, 38.5%) with a fornix-based scleral flap (n=14, 35.9%). 29 (74.4%) subjects had MMC 0.4% applied with 15 (38.5%) subjects having 2–3 minutes of application. A total of 14 (35.9%) subjects had concomitant cataract extraction with intraocular lens implantation.
Bleb location, type of scleral flap, type of anti-metabolite used and its duration of application, and whether other associated procedures were performed were not found to be statistically significant.
Further, we compared the eye with trabeculectomy and subsequent BRI with the fellow eye that had also undergone trabeculectomy but without BRI (n=13) and found no statistically significant differences in the intraoperative procedures (Table 3).
Postoperative events
7 (25%) blebitis subjects and 1 (11.1%) BRE subject underwent bleb manipulation or anti-metabolite injection, which was statistically insignificant (P=0.65). Postoperative complications in the form of bleb leaks were recorded more often in blebitis (n=6, 21.4%) than in BRE (n=0, 0%) (P=0.3). None of the blebitis subjects evolved to having BRE, nor did any of the BRE subjects suffer from prior blebitis. Table 4 shows the time between surgery and diagnosis of infection. Blebitis subjects presented later than BRE subjects (70.12 vs 26.75, P=0.038). There were no repeat infections in the same eye.
  | Table 4 Comparison of postoperative events between subjects with blebitis and subjects with bleb related endophthalmitis (n=39) |
Factors related to blebitis/BRE
Other factors such as IOP, visual acuity, and bleb vascularity at presentation are shown in Table 4. Subjects with BRE had a higher IOP on the day of presentation compared to those with blebitis (22.0 vs 8.9, P=0.011) and at days 2–7 (17.7 vs 11.0, P=0.002). BRE was associated with significantly poorer visual acuity compared to blebitis at presentation (1.73 vs 0.53), days 2–7 (2.21 vs 0.78), day 14 (1.97 vs 0.62) and at 1-month postinfection (1.51 vs 0.44) (P<0.001 for all values).
Conjunctival cultures were performed on all subjects and sent for gram stain and culture on aerobic, anaerobic and fungal media. 46.2% of the cultures yielded negative results. Streptococcus spp. were the most frequently isolated microbe (15.4%), followed by Haemophilus influenzae (12.8%) and coagulase-negative Staphylococcus (10.2%) (Table 5). Distribution was similar between BRE and blebitis subjects.
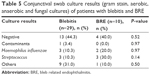  | Table 5 Conjunctival swab culture results (gram stain, aerobic, anaerobic and fungal cultures) of patients with blebitis and BRE |
Discussion
Characteristics are similar in both groups even though the visual outcome and clinical course, in the form of IOP findings and bleb vascularity, can diverge significantly. Notably, none of the blebitis subjects progressed onto BRE, conceivably due to timely intervention.
The racial distribution of BRI in our study was similar to local population demographics. While numerous studies have shown a male preponderance in the BRI group,1,17,22–24 most of these statistics have not reached significance. Our study concurs with this, with both groups being overrepresented by males (73.3% and 77.8%, P=0.71) (Table 1).
Most studies have been conducted in older populations with the average age of patients often being over 63. However, there is controversy over the degree of risk that age confers; some report a tendency for younger patients (<60 years of age) to develop BRI,4,6,9,12,24 while others display a noticeably older distribution.1,16,18,25 Our study supports the latter trend with BRE subjects being on average 10.7 years older than the blebitis group (P=0.026). Older patients are conferred a higher risk possibly because of their relatively immunocompromised state. This itself may be mediated via more comorbidities such as diabetes, which causes delayed healing of spontaneous bleb leaks and hence an increased susceptibility to trans-conjunctival passage of microorganisms.9,17,18
As in many other studies, the majority of our subjects had primary open angle glaucoma (n=28, 71.8%) with nearly half (n=18, 46.2%) having a coexisting eye condition. This reflects the underlying prevalence of this type of glaucoma among our trabeculectomy patients.12,19 Ocular conditions such as pigmentary glaucoma, juvenile glaucoma, nasolacrimal duct obstruction and ocular surface diseases have also been reported to increase the risk of BRIs but were not evaluated in our study.1,5,11,12,19
Studies over the decades have shown that several patient- and surgeon-related factors contribute to BRIs. Surgical practices such as limbal-based procedures produce higher, more avascular blebs, with a greater risk of infection.22 The approach used at our center was divided equally based on the surgeon’s choice and was not found to be significant in our study, concurring with the findings of the Collaborative Bleb-Related Infection Incidence and Treatment Study Group.9 Inferior limbal trabeculectomy blebs are associated with a higher risk of infection12,16,23 and this has shaped our current practice so that none were inferior trabeculectomies. The difference between superior nasally and superior temporally positioned blebs was not found to be significant (Tables 2 and 3).
Adjunctive anti-fibrotic use commonly produces blebs exhibiting epithelial breakdown with goblet cell depletion.26 This predisposes to thin walled, avascular blebs which lead to frank bleb leaks and have a decreased capacity for healing, possibly related to a limited blood supply causing ischemia.6,26–29 Neither anti-fibrotic agent was found to confer a greater risk for BRI (Tables 2 and 3), which concurs with other studies.5,8,12,13 The duration of exposure to the anti-fibrotic agent was also not significant (P=0.73). Furthermore, comparison of eyes with blebitis and BRE showed that both MMC and 5-FU displayed an almost identical risk profile in either group (Table 3).
A risk factor often implicated for BRI is multiple postoperative manipulations, although our study did not show this trend; possibly reflecting our relatively small sample size.12,16,22,28,30,31 Postoperative complications and manipulations did occur more often in our blebitis subjects than in BRE (21.4% vs 0%) but did not reach significance (Table 4). Blebitis subjects presented with the infection much later post-trabeculectomy, at 70.1 months vs 26.8 months in BRE patients (P=0.038) (Table 6). This may indicate that those with BRE have a more aggressive and acute clinical course or could be linked to the patients of an older age having a reduced ability to mount a robust immune response, hence the rapid progression to endophthalmitis. Whereas the younger blebitis subjects were able to suppress infection despite theoretically being at a higher risk and having more recorded instances of postoperative instrumentation.
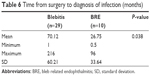  | Table 6 Time from surgery to diagnosis of infection (months)
|
Interestingly, we found a divergent course between the 2 BRIs regarding IOP. Preinfective IOP levels were similar between blebitis (12.8±3.2) and BRE (12.1±4.9). However, at presentation, mean IOPs in patients with blebitis dropped, while those with BRE almost doubled (8.9 mmHg vs 22.0 mmHg, P=0.011). The IOP in both groups stabilized by the second week posttreatment and closely resembled preinfective levels (Table 7). The lower IOP in the blebitis eyes may stem from occult or frank bleb leaks and sweating blebs, which are thought to initiate events.16,17 Compared to blebitis, BRE has significantly greater inflammation which frequently extends into the vitreous cavity.31 This may cause scarring of the bleb or trabeculitis and result in a higher IOP compared to blebitis.
At 6 months postinfection, patient with blebitis on average had visual acuity that was similar to preinfective levels 0.38 vs 0.48 (LogMAR acuity). Unfortunately, BRE patients did not fare as well, with preinfective vs 6-month postinfective readings of 0.61 vs 1.58, respectively.
Given the clinical course, it is expected that patients with BRE would have poorer visual acuity ( Table 7). Having a positive culture, which is more common in BRE, is also a significant risk factor for poor visual acuity.31 Blebitis on the other hand is a limited infection, which normally responds well to intensive topical antibiotic treatment. Our results indicate that while the mean IOP eventually returns to preinfective levels in a timely manner, the inflammatory damage wrought on the eye in BRE renders visual rehabilitation slow and likely with permanent impairment.
Bleb height was not a significant risk factor for either infection, with a relatively even distribution between the groups (P=0.32). Perhaps counter-intuitively, we found the increasing vascularity of the bleb at the time of presentation conferred some risk toward developing BRE (P=0.002); subjects with blebitis were more likely to have an avascular bleb (75.9%) than patients with BRE who tended to have moderately vascular blebs (50.0%) (Table 7).
We postulate that while the poor blood supply in avascular blebs is compatible with the poor immune response to infection, it could also work in containing the infection for a period of time, slowing the intraocular progression of the infection. Unsurprisingly, given the greater severity of inflammation, BRE subjects were more likely to present with a purulent bleb than their blebitis counterparts (90.0% vs 20.7%, P<0.001). This suggests that pus is a harbinger of poor outcome and is a strong indicator of blebitis being an antecedent to BRE.21,29
The distribution of microorganisms encountered in our study was slightly different to others (Table 5), which mostly implicate Streptococcus and Staphylococcus spp. in the US and East Asia, respectively.9,10,18,19,25,27,30 Almost half of our patients with BRIs were culture negative. While a few studies have reported similar rates of negative cultures,4,18 the overwhelming majority have yielded larger numbers of culture positive subjects.4,13,14,24,29 When positive, the vitreous and conjunctival cultures were correlated.
There are a few possibilities for this discrepancy: many of these studies utilized intraocular culture specimens,3,16,30,32 whereas our subjects had conjunctival swabs sent for gram stain and culture on aerobic, anaerobic and fungal mediums, and only BRE patients who underwent vitrectomy had vitreous cultures taken. Additionally, the initial culture was often performed in the emergency department by junior residents, employing nonstandardized methods.
The distribution of the causative microorganisms between the blebitis and BRE groups was very similar (Table 5), implying that no particular microorganism had a greater propensity to cause BRE.
Limitations
As with most related studies, limitations include the small sample size and retrospective case design and inadvertent poor documentation. As a single center report, there may be an inherent bias in the surgical techniques employed and geographic variability of microorganisms. The acquisition of cultures was not always systematic, standardized or timely and differed from many other studies. Documentation in some areas was lacking – in particular, surgical details and specific descriptions of the bleb on presentation.
Unfortunately, the timing of antibiotic commencement was also poorly documented and not shown to be significant in our study. This knowledge could have strengthened our hypothesis that a delay in treatment would result in BRE. A prospective case control study in which more cases of infection would be collected could corroborate our current findings.
Conclusion
Our findings reinforced a previously identified risk factor – age; and suggested other risk factors, male gender and diabetes, may have some bearing though they did not reach significance. It would thus be prudent for clinicians to note particularly if patients have these risk factors, and adjust their management as necessary.
Our study also showed that there was no significant difference in the position of a superior bleb, anti-fibrotic agent used and time the anti-fibrotic agent was applied, hence clinician preference can be exercised without much concern.
Finally, with the strong suggestion that patients with blebitis often presented with a lower IOP, clinicians should be particularly vigilant about a bleb leak or sweating bleb. Similarly, clinicians must be attuned to the fact that BRE patients often present with a higher IOP and institute early and aggressive treatment where required. Despite the potentially devastating effects of BRE, timely and appropriate management can result in a good outcome.
Acknowledgments
The abstract of this paper was submitted and accepted for the ARVO Annual Meeting, May 4–8, 2014 in Orlando, FL, USA. Unfortunately, due to extenuating circumstances, it was not presented at the conference. The abstract was published in Investigative Ophthalmology & Visual Science, April 2014, Vol 55, 4316 (http://iovs.arvojournals.org/article.aspx?articleid=2269816).
Disclosure
The authors report no conflicts of interest in this work.
References
DeBry PW, Perkins TW, Heatley G, Kaufman P, Brumback LC. Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin. Arch Ophthalmol. 2002;120(3):297–300. | ||
Higginbotham EJ, Stevens RK, Musch DC, et al. Bleb-related endophthalmitis after trabeculectomy with mitomycin C. Ophthalmology. 1996;103(4):650–656. | ||
Kangas TA, Greenfield DS, Flynn HW Jr, Parrish RK 2nd, Palmberg P. Delayed-onset endophthalmitis associated with conjunctival filtering blebs. Ophthalmology. 1997;104(5):746–752. | ||
Mochizuki K, Jikihara S, Ando Y, Hori N, Yamamoto T, Kitazawa Y. Incidence of delayed onset infection after trabeculectomy with adjunctive mitomycin C or 5-fluorouracil treatment. Br J Ophthalmol. 1997;81(10):877–883. | ||
Poulsen EJ, Allingham RR. Characteristics and risk factors of infections after glaucoma filtering surgery. J Glaucoma. 2000;9(6):438–443. | ||
Jampel HD, Quigley HA, Kerrigan-Baumrind LA, et al. Risk factors for late-onset infection following glaucoma filtration surgery. Arch Ophthalmol. 2001;119(7):1001–1008. | ||
Shigeeda T, Tomidokoro A, Chen YN, Shirato S, Araie M. Long-term follow-up of initial trabeculectomy with mitomycin C for primary open-angle glaucoma in Japanese patients. J Glaucoma. 2006;15(3):195–199. | ||
Olayanju JA, Hassan MB, Hodge DO, Khanna CL. Trabeculectomy-related complications in Olmsted County, Minnesota, 1985 through 2010. JAMA Ophthalmol. 2015;133(5):574–580. | ||
Yamamoto T, Sawada A, Mayama C, et al. The 5-year incidence of bleb-related infection and its risk factors after filtering surgeries with adjunctive mitomycin C: collaborative bleb-related infection incidence and treatment study 2. Ophthalmology. 2014;121(5):1001–1006. | ||
Vaziri K, Kishor K, Schwartz SG, et al. Incidence of bleb-associated endophthalmitis in the United States. Clin Ophthalmol. 2015;9: 317–322. | ||
Kim EA, Law SK, Coleman AL, et al. Long-Term Bleb-Related Infections After Trabeculectomy: Incidence, Risk Factors, and Influence of Bleb Revision. Am J Ophthalmol. 2015;159(6):1082–1091. | ||
Soltau JB, Rothman RF, Budenz DL, et al. Risk factors for glaucoma filtering bleb infections. Arch Ophthalmol. 2000;118(3):338–342. | ||
Sharan S, Trope GE, Chipman M, Buys YM. Late-onset bleb infections: prevalence and risk factors. Can J Ophthalmol. 2009;44(3):279–283. | ||
Busbee BG. Advances in knowledge and treatment: an update on endophthalmitis. Curr Opin Ophthalmol. 2004;15(3):232–237. | ||
Kuang TM, Lin YC, Liu CJ, Hsu WM, Chou CK. Early and late endophthalmitis following trabeculectomy in a Chinese population. Eur J Ophthalmol. 2008;18(1):66–70. | ||
Greenfield DS, Suner IJ, Miller MP, Kangas TA, Palmberg PF, Flynn HW Jr. Endophthalmitis after filtering surgery with mitomycin. Arch Ophthalmol. 1996;114(8):943–949. | ||
Lehmann OJ, Bunce C, Matheson MM, et al. Risk factors for development of post-trabeculectomy endophthalmitis. Br J Ophthalmol. 2000;84(12):1349–1353. | ||
Busbee BG, Recchia FM, Kaiser R, Nagra P, Rosenblatt B, Pearlman RB. Bleb-associated endophthalmitis: clinical characteristics and visual outcomes. Ophthalmology. 2004;111(8):1495–1503; discussion 1503. | ||
Ye H, Sun X, Gan D, et al. Bleb-associated endophthalmitis in a Chinese population (2003–2010): clinical characteristics and visual outcome. Eur J Ophthalmol. 2012;22(5):719–725. | ||
Zahid S, Musch DC, Niziol LM, Lichter PR; Collaborative Initial Glaucoma Treatment Study G. Risk of endophthalmitis and other long-term complications of trabeculectomy in the Collaborative Initial Glaucoma Treatment Study (CIGTS). Am J Ophthalmol. 2013;155(4):674–680, 680.e1. | ||
Prasad N, Latina MA. Blebitis and endophthalmitis after glaucoma filtering surgery. Int Ophthalmol Clin. 2007;47(2):85–97. | ||
Jampel HD, Solus JF, Tracey PA, et al. Outcomes and bleb-related complications of trabeculectomy. Ophthalmology. 2012;119(4):712–722. | ||
Solus JF, Jampel HD, Tracey PA, et al. Comparison of limbus-based and fornix-based trabeculectomy: success, bleb-related complications, and bleb morphology. Ophthalmology. 2012;119(4):703–711. | ||
Wolner B, Liebmann JM, Sassani JW, Ritch R, Speaker M, Marmor M. Late bleb-related endophthalmitis after trabeculectomy with adjunctive 5-fluorouracil. Ophthalmology. 1991;98(7):1053–1060. | ||
Leng T, Miller D, Flynn HW Jr, Jacobs DJ, Gedde SJ. Delayed-onset bleb-associated endophthalmitis (1996–2008): causative organisms and visual acuity outcomes. Retina. 2011;31(2):344–352. | ||
Matsuo H, Tomita G, Araie M, et al. Histopathological findings in filtering blebs with recurrent blebitis. Br J Ophthalmol. 2002;86(7):827. | ||
Mac I, Soltau JB. Glaucoma-filtering bleb infections. Curr Opin Ophthalmol. 2003;14(2):91–94. | ||
Alwitry A, King AJ. Surveillance of late-onset bleb leak, blebitis and bleb-related endophthalmitis – a UK incidence study. Graefes Arch Clin Exp Ophthalmol. 2012;250(8):1231–1236. | ||
Sbeity Z, Radcliffe N, Palmiero PM, Tello C, Liebmann J, Ritch R. Non-contact in vivo scanning laser microscopy of blebitis. Eye. 2009;23(7):1615–1616. | ||
Song A, Scott IU, Flynn HW Jr, Budenz DL. Delayed-onset bleb-associated endophthalmitis: clinical features and visual acuity outcomes. Ophthalmology. 2002;109(5):985–991. | ||
Yamamoto T, Kuwayama Y, Nomura E, Tanihara H, Mori K; Japan Glaucoma Society Survey of Bleb-related I. Changes in visual acuity and intra-ocular pressure following bleb-related infection: the Japan Glaucoma Society Survey of Bleb-related Infection Report 2. Acta Ophthalmol. 2013;91(6):e420–e426. | ||
Waheed S, Liebmann JM, Greenfield DS, et al. Recurrent bleb infections. Br J Ophthalmol. 1998;82(8):926–929. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




