Back to Journals » Therapeutics and Clinical Risk Management » Volume 15
Biomarkers and sociodemographic factors predicting one-year readmission among liver cirrhosis patients
Authors Dai J, Zhao J , Du Y , McNeil EB, Chongsuvivatwong V
Received 1 February 2019
Accepted for publication 25 July 2019
Published 8 August 2019 Volume 2019:15 Pages 979—989
DOI https://doi.org/10.2147/TCRM.S203883
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Jingyi Dai,1,2,* Jun Zhao,3,* Yingrong Du,1 Edward B McNeil,2 Virasakdi Chongsuvivatwong2
1Department of Liver Diseases, The Third People’s Hospital of Kunming City, Kunming, Yunnan, People’s Republic of China; 2Epidemiology Unit, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand; 3School of Public Health and Management, Hubei University of Medicine, Shiyan, Hubei, People’s Republic of China
*These authors contributed equally to this work
Background: Hospital readmissions of patients with cirrhosis is a current problem in China. This study aims to estimate the readmission rate at one year after discharge and to identify associated risk factors of hospital readmission.
Methods: Between January 2012 and December 2015, 3,402 patients admitted with cirrhosis were included in the study. The primary outcome was one-year inpatient readmission. Principal components analysis was conducted on the laboratory test indicators to reduce the number of dimensions. Univariate and multivariate analyses were performed using clinical and demographic data to identify independent associated factors of readmission within one year. The odds ratio (OR) and 95% confidence interval were used to assess the strength of association for each factor.
Results: Two dimensions, namely “liver function” and “renal function”, were revealed. Patients with a longer length of stay in the index admission (OR: 1.03; 95% CI: 1.03–1.04) and a higher dimension score of liver function (OR: 1.09; 95% CI: 1.05–1.13) were more likely to be readmitted within one-year. Older patients had a significantly higher odds of one-year readmission than younger patients (OR: 1.61; 95% CI: 1.22–2.11), patients who were married had a higher odds than those who were single (OR: 1.62; 95% CI: 1.12–2.36), and patients with hepatitis C virus were more likely to be readmitted within one year than patients with hepatitis B virus (OR: 1.51; 95% CI: 1.19–1.91).
Conclusion: Biomarkers and sociodemographic factors can identify patients at high risk for readmission within one year. Our data indicates the need to emphasize proper liver care to older patients who have been hospitalized for a long time.
Keywords: cirrhosis, readmission, liver function, renal function
Introduction
Cirrhosis, the final common pathway for the majority of liver diseases, leads to 150,000 deaths in China each year.1 Discharging hospitalized patients with cirrhosis is a complex process because these patients are at risk for complications that require hospital readmission. In the United States, one-year readmission rates of decompensated cirrhosis patients reached more than 50%.2,3 Readmission results in a financial burden on the health care system and on patients and their family and caregivers.2,4 In addition, readmission may provoke anxiety among patients and undermine their confidence in their doctors and the medical system.5 Reducing the hospital readmission rate has been targeted as a high priority in the United States.5 In fact, reliable data of cirrhosis patients’ readmission rates in China are limited.
Hospital readmission has been used as a marker of poor patient management and worse patient prognosis.6 The limitation of treatment methods has prompted researchers to explore risk factors of readmission, such as biomarkers and sociodemographic factors. Inpatients perform routine tests on admission, which are often used to determine patients’ condition. As a measure of disease severity, the Model for End-Stage Liver Disease (MELD) score synthesizes three indicators of routine tests,7 but other biomarkers such as platelets, albumin, and cholinesterase are not fully utilized. While most studies have focused on short-term (30 days or so) readmissions, we chose to focus on the longer one-year window to identify potential sociodemographic factors affecting readmission of which social-demographic factors may play important roles.
Evaluating the factors that affect readmission among cirrhosis can help to identify risk factors that may be responsive to targeted interventions. In this study, we constructed a model using both clinical and nonclinical data to stratify readmission risk among patients with cirrhosis. Our aim was to estimate the readmission rate at one year after discharge and to identify associated risk factors of readmission.
Methods
Patients
This follow-up study on retrospective data was conducted at the Third People’s Hospital of Kunming city in China. This hospital cares for a large proportion of cirrhosis patients in the region. We queried electronic medical records of hospitalized cirrhosis patients discharged between 2012 and 2015.
We identified unique index hospitalizations for adults (≥18 years) who were discharged with diagnoses consistent with cirrhosis as defined by the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM) diagnostic and procedural codes, after a review of each patient’s chart by two experienced hepatologists. The two experienced hepatologists identified unique index admissions for patients who were diagnosed with cirrhosis based on liver biopsy (when available), and combined factors including clinical characteristics, biochemical, and imaging examinations.
A patient is diagnosed as having compensated cirrhosis if no apparent decompensated events occur. Cirrhosis is classified as decompensated if the patient has complications such as ascites and/or jaundice (bilirubin >3 mg/dL) and/or upper digestive bleeding and/or encephalopathy at presentation. Our cohort subjects included all cirrhosis patients with and without decompensation in the first admission of the period of study. Patients were excluded if they: 1) died during the initial stay in hospital; 2) had hepatocellular carcinoma or HIV infection; 3) were end-stage renal failure or end-stage heart failure; or 4) received a liver transplant before or during the study period.
The first inpatient admission was considered as the index. Because the medical insurance department has a limit on the medical expenses for a single hospitalization in order to reduce overtreatment, we combined the records of those who were readmitted within the first 48 hrs of discharge into the index admission. The main outcome was whether the patient had at least one readmission in at least 48 hrs after the index admission. We also captured the records from the First Hospital Affiliated to Kunming Medical University to verify whether a patient was hospitalized during the study period.
Variables
Medical records for eligible patients were individually reviewed. Baseline variables included sex, age, ethnicity, occupation, marital status, etiology of cirrhosis, and 12 laboratory examination indicators. The pathogenesis of cirrhosis was ascertained from the medical record and categorized as hepatitis B virus (HBV), hepatitis C virus (HCV), alcoholic liver disease (documented history of alcoholic misuse and absence of other risk factors), multiple causes, and others (including autoimmune hepatitis, drug-induced hepatitis, and Wilsonian hepatitis). Patients with HBV or HCV with a remote history of alcohol consumption were classified as viral. The outcome was one-year inpatient readmissions.
Principal components analysis
We collected the patients’ laboratory tests from the electronic medical record in the hospital. The items currently considered routine and important for patients with cirrhosis were total bilirubin (TB), direct bilirubin (DB), albumin (ALB), cholinesterase (CHE), prothrombin time (PT), prothrombin activity percentage (PT.P), prothrombin International Normalization Ratio (INR), platelets (PLT), fibrinogen (FIB), urea nitrogen (URE), creatinine (CRE), and uric acid (UA). We checked the distributions of lab test indicators and transformed some of them using the natural logarithm transformation for those that had a skewed distribution, including INR, PT, DB, TB, CHE, PLT, URE, and CRE. Multi-collinearity was detected by the Kaiser-Meyer-Olkin (KMO) test. To overcome this problem, we used principal components analysis (PCA) to convert these correlated laboratory parameters into fewer dimensions, which are completely independent from each other yet still relatively understandable. Measure of sampling adequacy (MSA) of factor analytic data matrices revealed an overall value of 0.83 indicating an acceptable fit. We used a scree plot to determine the optimal number of dimensions needed and a biplot to visualize the two first principal components. The first two components explained 61.5% of the total variance of the 12 indicators.
Statistical analysis
Data were summarized as frequency counts and percentages for categorical variables, and mean with standard deviation or median with interquartile range for continuous variables. We used the χ2 test for categorical data and the Wilcoxon rank sum test for numerical data to examine univariate relationships between groups. We tried three multivariate logistic regression models and compared them with the AIC. Results indicated that the model using two dimensions from the PCA had a better fit (Table S1). Therefore, we used this model to identify independent predictors for readmissions within one year. The strengths of association were presented as odds ratios with 95% confidence intervals. Hosmer-Lemeshow goodness-of-fit test was used to evaluate the model fit.
Two-tailed P-values were reported, with values less than 0.05 considered as significant. All data analyses and visualizations were performed using R software version 3.4.1.8
Ethical consideration
Ethical approval was obtained from the Research Ethics Committee, Faculty of Medicine, Prince of Songkla University (REC: 61-048-18-1) and the Third People’s Hospital of Kunming (Ref: 2,017,082,860). Patient consent to review their medical records was not required by the ethics committees. The names and identification numbers of all patients were encrypted before use to ensure confidentiality. Approval to conduct the study was done in compliance with the Declaration of Helsinki.
Results
Study population
We identified 3,519 unique index admissions after applying the inclusion criteria. Ninety-eight patients with elective admission for scheduled therapeutic procedures (such as transjugular intrahepatic portosystemic shunt placement, hepatocellular cancer management) and 19 emergency patients admitted due to any diagnosis other than cirrhosis were excluded. Finally, 3,402 patients in the cohort with 6,625 admissions were analyzed.
Figure 1 shows a graphical display of the correlation matrix for the 12 laboratory indicators. The graph clearly shows two clusters; the first cluster includes nine indicators, mostly related to liver function and coagulation, the other cluster containing three indicators is related to renal function.
 |
Figure 1 Graphical display of the correlation matrix of the lab indicators. |
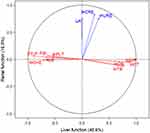
Results from principal components analysis
PCA revealed two independent dimensions as shown in Figure 2, confirming the two clusters suggested by Figure 1. The bundle of blue arrows is almost perpendicular with those of the red arrows. The red arrows for liver function were separated into two opposite directions; those indicating a healthy liver are on the left-hand side and those for a damaged liver are on the right. Correlations between values of the biomarker indicators and the two dimensions (loadings) are displayed in Table 1. Based on the meaning of indicators whose absolute correlation coefficients are greater than 0.5, we named the first dimension “liver function”, which loaded highly on INR, PT, DB, TB, ALB, CHE, PT.P, PLT, and FIB; and named the second dimension “renal function”, which loaded highly on URE, CRE and UA.
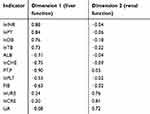 |
Table 1 Correlation coefficients between indicators and liver and renal function dimensions |
Descriptive statistic on the characteristics of the subjects
Demographic and clinical characteristics of patients’ index admissions are shown in Table 2. In general, 1,106 (32.5%) patients were farmers and 2,424 (71.3%) patients were male. 2,054 (60%) patients were aged between 40 and 60 years. The main origin of cirrhosis was hepatitis B virus (51.3%). The mean (standard deviation, SD) length of stay in the index admission was 21.8 (12.9) days. The mean (SD) value of the liver function dimension at discharge was −0.3 (2.1). The mean (SD) value of the renal dimension at discharge was −0.1 (1.2).
 |
Table 2 Univariate association for readmission within one year after index admission |
The readmission rate was plotted on a Kaplan-Meir curve as shown in Figure 3. A total of 997 (28.7%) patients were readmitted within one year of discharge. However, the actuarial probability of being readmitted within one year was 27.5%.
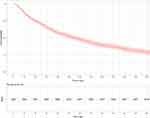 |
Figure 3 Kaplan-Meier curve showing probability of readmission within one year. |
Univariate analysis
The univariate association between each variable and one-year readmission are summarized in Table 2. All variables except gender and renal function dimension were significant and were therefore included in the multivariable analysis.
Multivariable analysis
In the multivariate logistic regression models (Table 3), age group, ethnicity, occupation, marital status, underlying cause of disease, length of stay in the index admission, and the dimension of liver function were consistently significantly associated with the risk of hospital readmission within one year while sex and renal dimension were consistently not significant. Patients with a longer length of stay in the index admission (OR: 1.03; 95% CI: 1.03–1.04) and a higher dimension score of liver function (OR: 1.09; 95% CI: 1.05–1.13) were more likely to be readmitted within one-year.
 |
Table 3 Logistic regression for predicting readmission within one year after index admission |
For other variables, patients who were older (≥60 years) had a significantly higher odds of one-year readmission than younger age patients (<40 years) (OR: 1.61; 95% CI: 1.22–2.11). Compared with farmers, patients who were staff or businesspersons had a higher odds of one-year readmission (OR: 1.73; 95% CI: 1.30–2.30, and OR: 1.5; 95% CI: 1.08–2.08, respectively). Patients who were married had a higher odds of one-year readmission than those who were single (OR: 1.62; 95% CI: 1.12–2.36). Finally, HCV patients were more likely to be readmitted within one year than HBV patients (OR: 1.51; 95% CI: 1.19–1.91).
Discussion
Our study found that readmission among patients with cirrhosis is common in the study area. We used principal components analysis to reduce the number of laboratory test indicators into two dimensions, namely “liver function” and “renal function”. Further analysis indicated that liver function and not renal function could significantly predict the risk of readmission within one year. Other significant predictors included age, ethnicity, occupation, marital status, underlying cause of disease, and length of stay in the index admission.
From other studies, the readmission rate of cirrhosis patients ranges from 21.2% to 53% for 90 days3,9 and 19.7% for one year.10 This wide range may be due to the difference in patients’ severity and after discharge care. The rate in our study was in the lower part of this range suggesting that some inpatients may not be very severe. Patient’s choice of medical visit is completely independent in China. That is to say, if cirrhosis patients feel symptoms, they are free to choose hospitals. It is possible that inpatients may not be fully fit for in-patient treatment and the condition may be resolved with out-patient treatment.
Various indicators of liver subfunction such as substance synthesis (ALB, CHE), bile management (TB, DB) and coagulation regulation (PT, INR, PT.P, PLT, FIB) are well correlated and form a “liver function” dimension. Our data suggested that damage to the liver from the disease process consistently affected these subfunctions. High correlations were also found among biomarkers of renal function (URE, CRE, UA). In many systemic diseases, renal and liver function may be damaged together, such as systemic lupus erythematosus and chemical poisoning. However, among the chronic liver diseases in this series, the dimension of liver function was quite distinct from the renal dimension. This could be explained that most readmissions were due to liver problems. Thus, avoiding exposure to potential hepato-toxic substances such as alcohol and some hepatotoxic drugs are very important among these patients.
In our study, patients with HCV infection had a significantly higher risk of readmission compared to patients with other etiologies. This may be attributed to Hepatitis C patients usually having a more severe prognosis.11 Oral antiviral therapy is universal for hepatitis B cirrhosis patients and physicians assess the need for antiviral therapy for these patients in China.12 Patients with hepatitis B cirrhosis have benefited from years of oral antiviral therapy.13 On the other hand, for hepatitis C patients, direct acting antivirals as a new effective medication were not available during the study period.14
Our study showed that patients with a longer length of stay in the index admission were more likely to be readmitted in the year after discharge. This result is consistent with another study from the US.4 The longer length of stay may indicate a relatively poorer functional status of the index admission. These patients, therefore, need careful discharge planning and psychosocial support to decrease readmission rates.
Except for gender, sociodemographic factors identified in this study such as age group, ethnicity, occupation, marital status, underlying cause of disease, length of stay in the index admission, and the dimension of liver function were stronger predictors of readmission. Consistent with other studies, older age was associated with an increase in hospital readmissions.4,15
Minority ethnic group were less likely to be readmitted within one year compared to Han, the major ethnic group in China. This finding is contrary to a previous report by Joynt et al.16 but is consistent with a recent report by Singh et al.17 We did not have information on income and education level of the patient from this retrospective dataset. Chinese who belong to a minority ethnic group and farmers, groups which are likely to have a lower socio-economic status compared to Han and other occupational groups, were less likely to be readmitted. This is contrary to our initial expectation as patients with a lower socioeconomic status should have worse home care and thus be more likely to be readmitted. One possible explanation could be that they had stronger barriers for readmission such as financial constraints and transportation problems. A prospective cohort study with complete follow up is needed to confirm these findings.
Our study illustrates that married patients have a higher risk of one-year readmission than single patients. Married patients may gain more family support and thus have more access to medical services.
We found that the odds of readmission for males and females was not significantly different. Although other studies have found that readmissions among women were less likely than men in cirrhotic patients18 and in non-cirrhotic populations,19 the source of the protective benefit is not clear. It may be due to psychosocial differences in the way women seek healthcare.18 One may also hypothesize that hormone levels in men are affected due to damage of the estrogen inactivation. However, this mechanism is not confirmed and there is no evidence of any benefit of testosterone for cirrhotic patients.20
Our hospital is specialized in liver diseases. Patients with complicated renal problems often receive more sophisticated treatment at other hospitals where renal replacement therapy procedures are more commonly performed. Our results may have therefore suffered from referral bias. We were unable to account for potential censoring of patients after their discharge from hospital nor could we collect data on alcohol consumption. We attempted to minimize this effect by excluding patients who died within one year post-discharge. Lastly, the study was done in a single province of China, thus generalizability of our results to other countries must be made with caution.
In conclusion, factors affecting hospital readmission in cirrhosis patients are multiple and complex. Biomarkers and sociodemographic factors can identify patients at high risk for readmission with moderate accuracy. Our data indicate the need to emphasize proper liver care to older patients who have been hospitalized for a long time.
Acknowledgments
This work was supported by the Project of Health Science and Technology Talents Ten Hundred Thousand in Kunming. The authors would like to thank the valuable work of Mr. Jinyu Duan.
Disclosure
Dr. Zhao Jun received a grant from Hubei University of Medicine (Grant No. 2018QDJZR14). The authors report no other conflicts of interest in this work.
References
1. Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the global burden of disease study 2013. Lancet. 2016;387(10015):251–272. doi:10.1016/S0140-6736(15)00551-6
2. Volk ML, Tocco RS, Bazick J, Rakoski MO, Lok AS. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107(2):247–252. doi:10.1038/ajg.2011.314
3. Bajaj JS, Reddy KR, Tandon P, et al. The 3‐month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology. 2016;64(1):200–208. doi:10.1002/hep.28414
4. Chirapongsathorn S, Krittanawong C, Enders FT, et al. Incidence and cost analysis of hospital admission and 30‐day readmission among patients with cirrhosis. Hepatol Commun. 2018;2(2):188–198. doi:10.1002/hep4.1137
5. Chirapongsathorn S, Talwalkar JA, Kamath PS. Readmission in cirrhosis: a growing problem. Curr Treat Options Gastroenterol. 2016;14(2):236–246. doi:10.1007/s11938-016-0091-1
6. Wong EL, Cheung AW, Leung MC, et al. Unplanned readmission rates, length of hospital stay, mortality, and medical costs of ten common medical conditions: a retrospective analysis of Hong Kong hospital data. BMC Health Serv Res. 2011;17(11):149. doi:10.1186/1472-6963-11-149
7. Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end‐stage liver disease. Hepatology. 2001;33(2):464–470. doi:10.1053/jhep.2001.22172
8. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2018.
9. Tapper EB, Halbert B, Mellinger J. Rates of and reasons for hospital readmissions in patients with cirrhosis: a multistate population-based cohort study. Clin Gastroenterol Hepatol. 2016;14(8):1181–8. e2. doi:10.1016/j.cgh.2016.04.009
10. Johnson KB, Campbell EJ, Chi H, et al. Advanced disease, diuretic use, and marital status predict hospital admissions in an ambulatory cirrhosis cohort. Dig Dis Sci. 2014;59(1):174–182. doi:10.1007/s10620-013-2832-5
11. Wang Z, Sheng YY, Dong QZ, Qin LX. Hepatitis B virus and hepatitis C virus play different prognostic roles in intrahepatic cholangiocarcinoma: a meta-analysis. World J Gastroenterol. 2016;22(10):3038–3051. doi:10.3748/wjg.v22.i10.3038
12. Zheng X, Wang J, Yang D. Antiviral therapy for chronic hepatitis B in China. Med Microbiol Immunol. 2014;204(1):115–120. doi:10.1007/s00430-014-0380-z
13. Wang Y, Jia J. Control of hepatitis B in China: prevention and treatment. Expert Rev Anti Infect Ther. 2011;9(1):21–25. doi:10.1586/eri.10.143
14. Xie Q, Xuan JW, Tang H, et al. Hepatitis C virus cure with direct acting antivirals: clinical, economic, societal and patient value for China. World J Hepatol. 2019;11(5):421–441. doi:10.4254/wjh.v11.i5.421
15. Garcia-Perez L, Linertova R, Lorenzo-Riera A, Vazquez-Diaz JR, Duque-Gonzalez B, Sarria-Santamera A. Risk factors for hospital readmissions in elderly patients: a systematic review. QJM. 2011;104(8):639–651. doi:10.1093/qjmed/hcr070
16. Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for medicare beneficiaries by race and site of care. Jama. 2011;305(7):675–681. doi:10.1001/jama.2011.123
17. Singh S, Lin YL, Kuo YF, Nattinger AB, Goodwin JS. Variation in the risk of readmission among hospitals: the relative contribution of patient, hospital and inpatient provider characteristics. J Gen Intern Med. 2014;29(4):572–578. doi:10.1007/s11606-013-2723-7
18. Berman K, Tandra S, Forssell K, et al. Incidence and predictors of 30-day readmission among patients hospitalized for advanced liver disease. Clin Gastroenterol Hepatol. 2011;9(3):254–259. doi:10.1016/j.cgh.2010.10.035
19. Gonzalez JR, Fernandez E, Moreno V, et al. Sex differences in hospital readmission among colorectal cancer patients. J Epidemiol Community Health. 2005;59(6):506–511. doi:10.1136/jech.2004.028902
20. Sinclair M, Grossmann M, Gow PJ, Angus PW. Testosterone in men with advanced liver disease: abnormalities and implications. J Gastroenterol Hepatol. 2015;30(2):244–251. doi:10.1111/jgh.12695
Supplementary material
 |
Table S1 Comparison of models for predicting readmission within one year after index admission |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.