Back to Journals » OncoTargets and Therapy » Volume 9
Benefit of percutaneous endoscopic gastrostomy in patients undergoing definitive chemoradiotherapy for locally advanced nasopharyngeal carcinoma
Authors Xu Y , Guo Q , Lin J, Chen B , Wen J, Lu T, Xu Y, Zhang M, Pan J, Lin S
Received 20 July 2016
Accepted for publication 12 September 2016
Published 4 November 2016 Volume 2016:9 Pages 6835—6841
DOI https://doi.org/10.2147/OTT.S117676
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samir Farghaly
Yun Xu,1,2 Qiaojuan Guo,1,2 Jin Lin,1,2 Bijuan Chen,1,2 Jiangmei Wen,1,2 Tianzhu Lu,1,2 Yuanji Xu,1,2 Mingwei Zhang,1,2 Jianji Pan,1,2 Shaojun Lin1,2
1Department of Radiation Oncology, Fujian Provincial Cancer Hospital, 2Fujian Provincial Key Laboratory of Translational Cancer Medicine, Fuzhou, Fujian, People’s Republic of China
Background and aim: To evaluate the impact of percutaneous endoscopic gastrostomy (PEG) tube on nutritional status, treatment-related toxicity, and treatment tolerance in patients with locally advanced nasopharyngeal carcinoma (NPC) who underwent chemoradiotherapy.
Patients and methods: We enrolled 133 consecutive non-metastatic NPC (III/IV stage) patients, who were treated with prophylactic PEG feeding before the initiation of concurrent chemoradiotherapy (CCRT) between June 1, 2010 and June 30, 2014. Meanwhile, another 133 non-PEG patients, who were matched for age, gender, and tumor, node, metastases stage, were selected as historical control cohort. Weight and nutritional status changes from pre-radiotherapy to the end of radiotherapy were evaluated, and treatment tolerance and related acute toxicities were analyzed as well.
Results: We found that significantly more patients (91.73%) in the PEG group could finish two cycles of CCRT, when compared with those in the non-PEG group (57.89%) (P<0.001). We also indicated that more patients (50.38%) in the non-PEG group experienced weight loss of ≥5%, while the phenomenon was only found in 36.09% patients in the PEG group (P=0.019). In addition, the percentage of patients who lost ≥10% of their weight was similar in these two groups. Changes in albumin and prealbumin levels during radiotherapy in the non-PEG group were higher than those obtained for the PEG group with significant differences (P-values of 0.023 and <0.001, respectively). Furthermore, patients in the PEG group had significantly lower incidence of grade III acute mucositis than those in the non-PEG group (22.56% vs 36.84%, P=0.011). Tube-related complications occurred only in 14 (10.53%) patients in the PEG group, including incision infection of various degrees.
Conclusion: PEG and intensive nutrition support may help to minimize body weight loss, maintain nutritional status, and offer better treatment tolerance for patients with locally advanced NPC who underwent CCRT.
Keywords: locally advanced nasopharyngeal carcinoma, percutaneous endoscopic gastrostomy, chemoradiotherapy, nutritional status, treatment-related toxicity
Introduction
Nasopharyngeal carcinoma (NPC) is the most common head and neck malignancy in southern China.1 Seventy percent of patients at diagnosis present with locally advanced disease,2 which requires aggressive therapy to achieve adequate localregional control. Concurrent chemoradiotherapy (CCRT) is the standard treatment for locoregional advanced NPC (LA-NPC).3,4 Unfortunately, CCRT is associated with significant treatment-related toxicities, including mucositis, odynophagia, dysphagia, xerostomia, and vomiting.5,6 These complications can put patients at risk of malnutrition, thereby compromising treatment tolerance and efficacy, and increasing health care costs.7 Therefore, appropriate temporary nutritional support is an essential part of management protocols for locally advanced NPC patients undergoing definitive CRT.
Percutaneous endoscopic gastrostomy (PEG) tubes, placed with a minimally invasive technique, could improve patient comfort and tolerance. PEG tube placement is recommended by the American Gastroenterological Association for patients requiring nutrition supplementation for more than a month.8 For several decades, the role of PEG tubes has been specifically assessed for nutrition support in head and neck cancer (HNC) patients, particularly those with tongue, oropharyngeal, and hypopharyngeal carcinomas, and NPC.9–14 Those literatures suggested that prophylactic PEG tube placement could improve treatment tolerance, prevent weight loss and malnutrition, and improve overall survival for HNC patients. Besides, only one study specially evaluated the benefit of reducing weight loss from the placement of PEG tubes for NPC patients during CRT.15 But that study did not evaluate the tolerance of concurrent chemotherapy and other benefits of nutrition status from the PEG tube for LA-NPC patients during CCRT.
It is therefore essential to explore whether NPC patients could benefit from prophylactically placed PEG tubes during radiotherapy. The purpose of this case–control study was to evaluate the effects of PEG on body weight, serum albumin level, treatment tolerance, and acute toxicity in locally advanced NPC patients who underwent definitive CRT.
Patients and methods
Patient selection
This retrospective study was approved by the Institutional Review Board of Fujian Provincial Cancer Hospital with a waiver of written informed consent. Between June 1, 2010 and June 30, 2014, a total of 133 consecutive LA-NPC patients who received prophylactic PEG feeding at the physician’s discretion before the initiation of CRT were enrolled. Meanwhile, 133 non-PEG patients who were matched according to age, gender, and tumor, node, metastases stage were selected as historical control cohort (1:1 matching). Patients were staged according to the seventh edition of American Joint Committee on Cancer staging system and clinically confirmed as stage III/IV at the Fujian Provincial Cancer Hospital.
PEG placement
Evaluation for PEG tube placement included a complete health history and physical examination; all patients had no serious gastric or other gastrointestinal tract diseases, liver or kidney dysfunction, congestive heart failure, progressive malignant hypertension, dementia, respiratory failure, or coma. Patients were selected based on the inclusion criteria and counseled regarding the possibility of mucositis, dysphagia, and odynophagia by the radiation oncologist before radiation therapy. The possibility of PEG tube placement was discussed and based on patient preference. All PEG tubes were placed using the pull method as described previously.16 The patients received a single dose of antibiotics 1 day after PEG placement. The PEG tubes were placed before starting radiation therapy and removed after the disappearance of acute mucositis, allowing sufficient food intake through the mouth (about 4–6 weeks after the completion of radical radiotherapy).
Radiation treatment and chemotherapy
All the patients were treated with intensity-modulated radiotherapy (IMRT), with delineation of clinical and nodal target volumes carried out as reported previously.17 In brief, radiation target volumes included gross primary and nodal masses, with all areas of potentially involved regions. A total dose at a primary tumor site was 66–80 Gy (median, 70.95 Gy), with 55 patients (including 21 patients with T4 disease) receiving a boost treatment after definitive IMRT because of residual disease in the primary site and/or metastasis lymph nodes.
All patients assessed here were treated with cisplatin-based neoadjuvant chemotherapy (NACT) plus CCRT, except three who had only two CCRT cycles. The chemotherapy regimen was paclitaxel at 135 mg/m2 on day 1 and cisplatin at 80 mg/m2 on day 2. Stage IV patients received two NACT cycles; the chemotherapy regimen was gemcitabine at 1,000 mg/m2 (days 1 and 8) and paclitaxel at 135 mg/m2 (day 1). All patients received cisplatin-based CCRT regimens that included a single agent (100 mg/m2 cisplatin at day 1) and two drugs (135 mg/m2 paclitaxel combined with 80 mg/m2 cisplatin or 1,000 mg/m2 gemcitabine) every 3 weeks.
Nutritional support
Enteral feeding was carried out daily, generally in six sessions, and depending on the estimated calorie requirements of the patient, with main meals from 200 to 250 mL and secondary meals from 100 to 150 mL, for total amounts of 1,500 to 2,000 mL a day. To avoid stomach discomfort, food temperature was maintained between 38°C and 40°C. Before food injection, the tube’s position was confirmed and 20 mL warm water was first injected; then, food was administered and 20 mL warm water was used for gastric washing to prevent clogging.
Data collection
Patient records were reviewed to collect pre-radiotherapy and end of radiotherapy nutrition status information, including baseline body weight, and hemoglobin, albumin, and prealbumin levels. Pre-radiotherapy information was obtained at the beginning of radiation therapy, while end of radiotherapy information was obtained at the end of radiation therapy. The treatment-related complications were recorded for the duration of radiotherapy. Acute toxicity was graded according to the Radiation Therapy Oncology Group/European Organization for the Treatment of Cancer radiation toxicity criteria.18 Changes in nutrition status during radiotherapy were defined as a difference between pre-radiotherapy and end of radiotherapy. Radiation interruptions were defined as the interruption time of radiation >7 days.19
Statistical analyses
Statistical analyses were carried out using the SPSS statistical software package, version 18.0 (SPSS, Inc., Chicago, IL, USA). The chi-square test was used to compare proportions in the subsets analyzed. The Mann–Whitney U-test was used to assess non-normal distribution parameters of independent samples. A two-tailed P<0.05 was considered as statistically significant.
Results
Patient characteristics
Baseline clinical characteristics of both PEG and non-PEG cohorts are summarized in Table 1. Overall, age, gender distribution, pathology, and T, N and clinical stages were similar between the two groups. Most of the patients received CCRT of single-agent cisplatin, while only 22 patients in stage IVb received CCRT of the two-drug regimen, including 7 and 15 patients in the non-PEG and PEG groups, respectively.
Weight loss
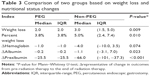
Table 2 illustrates the degrees of weight loss during radiation therapy for PEG and non-PEG groups. A total of 226/266 patients (84.96%) treated with definitive CRT lost weight, including 115 patients who lost between 5% and 10% of their baseline body weight and 16 others who lost ≥10% of their initial body weight. Only 22 patients retained their baseline body weight, while 18 individuals gained weight at the time of radiation therapy completion.
  | Table 2 Percent weight loss during radiation therapy for the two groups |
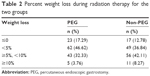
Among the 133 patients treated without PEG tubes, 67 patients (50.38%) lost ≥5% of their baseline body weight at the end of radiation therapy, which was significantly higher than the value obtained for the PEG group (36.09%, P=0.019). Median weight losses (from first to last days of radiation therapy) in the PEG and non-PEG groups were 2.0 and 3.0 kg, respectively, indicating a reduction of 3.8% and 5.0%, respectively (P=0.009 and P=0.010, for absolute and percentage weight loss, respectively). These results are shown in Table 3.
Nutritional status
Changes in albumin and prealbumin levels during radiotherapy in the non-PEG group were higher than those obtained for the PEG group, with significant differences (P-values of 0.023 and <0.001, respectively). No significant differences were noted in the hemoglobin levels at the end of IMRT between PEG and non-PEG patients (P=0.074), as detailed in Table 3.
Treatment compliance and acute toxicity
A total of 91.73% and 57.89% patients completed two cycles of CCRT in PEG and non-PEG groups, respectively (P<0.001). Treatment interruptions were observed in 5.26% and 9.77% patients for the PEG and non-PEG groups, respectively (P=0.163). Acute toxicity rates are also shown in Table 4 for both patient groups. The most common non-hematologic toxicity was mucositis, followed by xerostomia and skin desquamation. No patient had more than grade IV acute mucositis in either group. Only 22.56% patients had grade III acute mucositis in the PEG group; this incidence was significantly lower compared with the 36.84% obtained for the non-PEG group (P=0.011).
  | Table 4 Treatment-related side effects on two groups |
Tube-related complications
PEG tubes have occasionally been associated with significant morbidity indexes, including incision infection, bowel perforation, gastrointestinal hemorrhage, peritonitis, tube dislodgement and clogging, and even death. For all patients, gastric tube removal time was between 1 and 3 months; none of the patients required it for >3 months, which meant that no patient in this study was tube-dependent. Eleven patients (8.27%) suffered from varying degrees of incision infection; there was one case each of peritonitis, gastrointestinal hemorrhage, and tube dislodgement. These patients were treated with antibiotics and a symptomatic approach. Thanks to effective treatment, the complications were cured, with no impact on radiotherapy.
Discussion
PEG tubes have been used to provide nutrition support and reduce the severity of malnutrition during radiotherapy for HNC patients.9–14 This large sample study assessed PEG nutritional support for NPC patients. Our data indicated that PEG tube placement constituted a feasible nutritional intervention with several advantages: effective reduction of treatment-related weight loss, nutritional status maintenance, incidence reduction of treatment-related side effects, and improved CRT tolerance to CCRT. This study demonstrated the feasibility of prophylactic PEG tube placement in NPC patients during radiotherapy.
Weight loss is a nutritional indicator that reflects reduced intake or nutritional imbalance. Weight loss is commonly observed in HNC patients during treatment, especially NPC patients receiving CRT.20,21 Prophylactic PEG tubes, which were adopted in our study, have been reported by other investigators to be highly effective in reducing treatment-related weight loss in HNC patients.22,23 Recently, a meta-analysis also demonstrated that PEG tube placement was an effective measure that reduces weight loss and is a better choice in malnutrition management in the HNC patients undergoing radiotherapy or CRT. In accordance with those studies, we found that PEG maintains a patient’s body weight and reduces the incidence of weight loss and the absolute value of weight loss. Several retrospective studies demonstrated that weight loss is the strongest independent predictor of survival in patients with HNC.21,24 Recently, two reports from China indicated that NPC patients with high weight loss during treatment have significantly poor survival.25,26 Therefore, it is necessary to maintain weight in cancer patients during the treatment period. Although unplanned weight loss among those not receiving nutrition via prophylactic PEG tubes appeared to be temporary and reversible in the ensuing recovery period, others have demonstrated that loss of >5% of baseline body weight during radiation treatment may decrease the efficacy of treatment.27–29 Unfortunately, survival differences between both groups cannot be assessed here due to the relatively short follow-up time.
Our study also showed that PEG tube placement effectively improved nutritional status and mitigated the decreased albumin and prealbumin levels. But our study found that there was no difference in the hemoglobin levels between the two groups. These results were easy to understand. The syntheses of albumin and prealbumin was affected by the nutritional status of patients.30 The half-life of prealbumin and albumin is short, which is more sensitive to nutritional status than hemoglobin.31,32 Patients with PEG tube placement can be guaranteed enough nutrient intakes. So the syntheses of albumin and prealbumin was not heavy influenced in PEG group.
Furthermore, our study highlights the importance of prophylactic nutritional approach using PEG tubes to support nutritional status and decrease the cumulative incidence of treatment-related side effects during CCRT of locally advanced NPC. Many studies have shown that CCRT increases treatment-related toxicity, especially acute mucositis, which could lead to treatment interruption and chemotherapy tolerance.33,34 The reason may lie in the nutritional status. It is possible that the improvement in nutritional status obtained through PEG may translate into reduced CRT-related toxicity. Nutrition support for patients undergoing CCRT was confirmed to be an important measure for maintaining both energy and protein.35 Multiple studies demonstrated that PEG tubes can ameliorate malnutrition in patients with HNC undergoing radiation therapy.14,15,36,37
More importantly, we found that prophylactic PEG significantly improved CRT tolerance. Although prophylactic PEG group patients had a high rate of two-cycle concurrent chemotherapy completion, our study showed that no significant differences in treatment interruption were obtained between both groups. Previous reports demonstrated that longer treatment interruptions significantly reduce progression-free and overall survival rates.38–41 Moreover, malnutrition itself can alter patient prognosis because it causes decreased immune function and treatment tolerance, unplanned breaks during therapy, and weight loss, which are associated with worse disease control.42 With the high acceptability rate of concurrent and intensive chemotherapy, prophylactic PEG could bring survival benefit. Our team will further extend follow-up time in this population to evaluate potential survival benefits.
PEG tubes are widely used to provide long-term feeding access. Although generally considered safe, PEG tubes can be associated with significant complications. A recent systematic review noted mortality and major complication rates of 2.2% and 7.4%, respectively. Minor complications, however, such as tube malfunction or dislodgement, tube leakage, minor bleeding, ileus, or superficial infections, ranged from 1% to 30%.43 We did observe acceptable rates of PEG tube-related complications, with 14 patients (10.53%) suffering from varying degrees of incision infection, peritonitis, gastrointestinal hemorrhage, and tube dislodgement. A study by Olson et al showed that the prophylactic approach results in more gastrostomy tube complications rates in patients who may have never needed a gastrostomy tube during the course of their concurrent systemic and radiation therapy.44 Therefore, it is necessary to select patients who need a PEG tube and benefit from placement of PEG tube at CRT.
There are several limitations in this study. First, although this was a well-designed study, its retrospective nature has an inherited and fundamental pitfall. Selection biases would be the main potential biases, because receiving PEG tube was according to patients’ will. Well-compliant patients would be more prone to receiving PEG tube, which would have affected the results of this study. Thus, a prospective study with multicenter participation is warranted to demonstrate the benefits of PEG. Second, considering the short follow-up time, we could not determine whether prophylactic gastrostomy results in survival benefits, and longer follow-up is needed to address this issue.
Conclusion
Overall, we showed that PEG tube feeding may be beneficial in patients with advanced NPC, especially those undergoing more intense treatment regimens, by preventing weight loss, reducing treatment-related toxicity, and maintaining nutritional status. PEG tube placement may be an essential nutrition support to improve treatment tolerance and likely improve survival. Further studies, including prospective trials, are needed to delineate the value of prophylactic PEG in long-term survival and quality of life of advanced NPC patients.
Acknowledgments
This work was funded by National Clinical Key Specialty Construction Program, and Key Clinical Specialty Discipline Construction Program of Fujian, People’s Republic of China. This research was also supported by a grant from the National Natural Science Foundation of China (grant No 81470134) and Fujian Provincial Natural Science Foundation of China (grant No 2014J0101). The authors thank Dr He Huang, Endosopy Room of Fujian Provincial Cancer Hospital, for his help with the placement of the PEG tube into patients with NPC.
Disclosure
The authors report no conflicts of interest in this work.
References
Wei WI, Sham JS. Nasopharyngeal carcinoma. Lancet. 2005;365(9476):2041–2054. | ||
Afqir S, Ismaili N, Errihani H. Concurrent chemoradiotherapy in the management of advanced nasopharyngeal carcinoma: current status. J Cancer Res Ther. 2009;5(1):3–7. | ||
Lee AW, Tung SY, Chan AT, et al. Preliminary results of a randomized study (NPC-9902 Trial) on therapeutic gain by concurrent chemotherapy and/or accelerated fractionation for locally advanced nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2006;66(1):142–151. | ||
Bahl M, Siu LL, Pond GR, et al. Tolerability of the Intergroup 0099 (INT 0099) regimen in locally advanced nasopharyngeal cancer with a focus on patients’ nutritional status. Int J Radiat Oncol Biol Phys. 2004;60(4):1127–1136. | ||
Du CR, Ying HM, Kong FF, Zhai RP, Hu CS. Concurrent chemoradiotherapy was associated with a higher severe late toxicity rate in nasopharyngeal carcinoma patients compared with radiotherapy alone: a meta-analysis based on randomized controlled trials. Radiat Oncol. 2015;10:70. | ||
Al-Sarraf M, LeBlanc M, Giri PG, et al. Chemoradiotherapy versus radiotherapy in patients with advanced nasopharyngeal cancer: phase III randomized Intergroup study 0099. J Clin Oncol. 1998;16(4):1310–1317. | ||
Ravasco P, Monteiro-Grillo I, Marques Vidal P, Camilo ME. Impact of nutrition on outcome: a prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head Neck.2005;27(8):659–668. | ||
American Gastroenterological Association medical position statement: guidelines for the use of enteral nutrition. Gastroenterology. 1995;108(4):1280–1281. | ||
Rustom IK, Jebreel A, Tayyab M, England RJ, Stafford ND. Percutaneous endoscopic, radiological and surgical gastrostomy tubes: a comparison study in head and neck cancer patients. J Laryngol Otol. 2006;120(6):463–466. | ||
Raykher A, Russo L, Schattner M, Schwartz L, Scott B, Shike M. Enteral nutrition support of head and neck cancer patients. Nutr Clin Pract. 2007;22(1):68–73. | ||
Hunter AM. Nutrition management of patients with neoplastic disease of the head and neck treated with radiation therapy. Nutr Clin Pract. 1996;11(4):157–169. | ||
Murayama KM. Enteral feeding tube placement in head and neck cancer patients: special considerations. Nutr Clin Pract. 1997;12(1 Suppl):S34–S37. | ||
Lee JH, Machtay M, Unger LD, et al. Prophylactic gastrostomy tubes in patients undergoing intensive irradiation for cancer of the head and neck. Arch Otolaryngol Head Neck Surg. 1998;124(8):871–875. | ||
Romesser PB, Romanyshyn JC, Schupak KD, et al. Percutaneous endoscopic gastrostomy in oropharyngeal cancer patients treated with intensity-modulated radiotherapy with concurrent chemotherapy. Cancer. 2012;118(24):6072–6078. | ||
Peerawong T, Phungrassami T, Pruegsanusak K, Sangthong R. Comparison of treatment compliance and nutritional outcomes among patients with nasopharyngeal carcinoma with and without percutaneous endoscopic gastrostomy during chemoradiation. Asian Pac J Cancer Prev. 2012;13(11):5805–5809. | ||
Ponsky JL, Gauderer MW, Stellato TA. Percutaneous endoscopic gastrostomy. Review of 150 cases. Arch Surg. 1983;118(8):913–914. | ||
Lin S, Pan J, Han L, Zhang X, Liao X, Lu JJ. Nasopharyngeal carcinoma treated with reduced-volume intensity-modulated radiation therapy: report on the 3-year outcome of a prospective series. Int J Radiat Oncol Biol Phys. 2009;75(4):1071–1078. | ||
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995;31(5):1341–1346. | ||
Kwong DL, Sham JS, Chua DT, Choy DT, Au GK, Wu PM. The effect of interruptions and prolonged treatment time in radiotherapy for nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 1997;39(3):703–710. | ||
Nguyen NP, Moltz CC, Frank C, et al. Dysphagia following chemoradiation for locally advanced head and neck cancer. Ann Oncol. 2004;15(3):383–388. | ||
Langius JA, van Dijk AM, Doornaert P, et al. More than 10% weight loss in head and neck cancer patients during radiotherapy is independently associated with deterioration in quality of life. Nutr Cancer. 2013;65(1):76–83. | ||
Silander E, Nyman J, Bove M, Johansson L, Larsson S, Hammerlid E. Impact of prophylactic percutaneous endoscopic gastrostomy on malnutrition and quality of life in patients with head and neck cancer: a randomized study. Head Neck. 2012;34(1):1–9. | ||
Salas S, Baumstarck-Barrau K, Alfonsi M, et al. Impact of the prophylactic gastrostomy for unresectable squamous cell head and neck carcinomas treated with radio-chemotherapy on quality of life: prospective randomized trial. Radiother Oncol. 2009;93(3):503–509. | ||
Takenaka Y, Yamamoto M, Nakahara S, et al. Factors associated with malnutrition in patients with head and neck cancer. Acta Otolaryngol. 2014;134(10):1079–1085. | ||
Zeng Q, Shen LJ, Guo X, Guo XM, Qian CN, Wu PH. Critical weight loss predicts poor prognosis in nasopharyngeal carcinoma. BMC Cancer. 2016;16:169. | ||
Du XJ, Tang LL, Mao YP, et al. Value of the prognostic nutritional index and weight loss in predicting metastasis and long-term mortality in nasopharyngeal carcinoma. J Transl Med. 2015;13:364. | ||
Lin YH, Chang KP, Lin YS, Chang TS. Evaluation of effect of body mass index and weight loss on survival of patients with nasopharyngeal carcinoma treated with intensity-modulated radiation therapy. Radiat Oncol. 2015;10:136. | ||
Langius JA, Bakker S, Rietveld DH, et al. Critical weight loss is a major prognostic indicator for disease-specific survival in patients with head and neck cancer receiving radiotherapy. Br J Cancer. 2013;109(5):1093–1099. | ||
Shen LJ, Chen C, Li BF, Gao J, Xia YF. High weight loss during radiation treatment changes the prognosis in under-/normal weight nasopharyngeal carcinoma patients for the worse: a retrospective analysis of 2433 cases. PLoS One. 2013;8(7):e68660. | ||
Winkler MF, Pomp A, Caldwell MD, Albina JE. Transitional feeding: the relationship between nutritional intake and plasma protein concentrations. J Am Diet Assoc. 1989;89(7):969–970. | ||
Klein S. The myth of serum albumin as a measure of nutritional status. Gastroenterology. 1990;99(6):1845–1846. | ||
Huebers HA, Finch CA. The physiology of transferrin and transferrin receptors. Physiol Rev. 1987;67(2):520–582. | ||
Lazarus CL, Logemann JA, Pauloski BR, et al. Swallowing disorders in head and neck cancer patients treated with radiotherapy and adjuvant chemotherapy. Laryngoscope. 1996;106(9 Pt 1):1157–1166. | ||
Lee AW, Lau WH, Tung SY, et al; Hong Kong Nasopharyngeal Cancer Study Group. Preliminary results of a randomized study on therapeutic gain by concurrent chemotherapy for regionally-advanced nasopharyngeal carcinoma: NPC-9901 Trial by the Hong Kong Nasopharyngeal Cancer Study Group. J Clin Oncol. 2005;23(28):6966–6975. | ||
Isenring EA, Capra S, Bauer JD. Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br J Cancer. 2004;91(3):447–452. | ||
Wiggenraad RG, Flierman L, Goossens A, et al. Prophylactic gastrostomy placement and early tube feeding may limit loss of weight during chemoradiotherapy for advanced head and neck cancer, a preliminary study. Clin Otolaryngol. 2007;32(5):384–390. | ||
Zhang Z, Zhu Y, Ling Y, Zhang L, Wan H. Comparative effects of different enteral feeding methods in head and neck cancer patients receiving radiotherapy or chemoradiotherapy: a network meta-analysis. OncoTargets Ther. 2016;9:2897–2909. | ||
Suwinski R, Sowa A, Rutkowski T, Wydmanski J, Tarnawski R, Maciejewski B. Time factor in postoperative radiotherapy: a multivariate locoregional control analysis in 868 patients. Int J Radiat Oncol Biol Phys. 2003;56(2):399–412. | ||
Herrmann T, Baumann M. [Prolongation of latency or overall treatment time by unplanned radiation pauses. The clinical importance of compensation]. Strahlenther Onkol. 2005;181(2):65–76. | ||
Langendijk JA, de Jong MA, Leemans CR, et al. Postoperative radiotherapy in squamous cell carcinoma of the oral cavity: the importance of the overall treatment time. Int J Radiat Oncol Biol Phys. 2003;57(3):693–700. | ||
Tarnawski R, Fowler J, Skladowski K, et al. How fast is repopulation of tumor cells during the treatment gap? Int J Radiat Oncol Biol Phys. 2002;54(1):229–236. | ||
van Bokhorst-de van der Schuer, van Leeuwen PA, Kuik DJ, et al. The impact of nutritional status on the prognoses of patients with advanced head and neck cancer. Cancer. 1999;86(3):519–527. | ||
Grant DG, Bradley PT, Pothier DD, et al. Complications following gastrostomy tube insertion in patients with head and neck cancer: a prospective multi-institution study, systematic review and meta-analysis. Clin Otolaryngol. 2009;34(2):103–112. | ||
Olson R, Karam I, Wilson G, Bowman A, Lee C, Wong F. Population-based comparison of two feeding tube approaches for head and neck cancer patients receiving concurrent systemic-radiation therapy: is a prophylactic feeding tube approach harmful or helpful? Support Care Cancer. 2013;21(12):3433–3439. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.