Back to Journals » Research and Reports in Tropical Medicine » Volume 11
Basic Coagulation Profiles and Platelet Count Among Schistosoma mansoni-Infected Adults Attending Sanja Primary Hospital, Northwest Ethiopia
Authors Eyayu T , Zeleke AJ , Seyoum M, Worku L
Received 6 January 2020
Accepted for publication 7 April 2020
Published 22 April 2020 Volume 2020:11 Pages 27—36
DOI https://doi.org/10.2147/RRTM.S244912
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Mario Rodriguez-Perez
Tahir Eyayu,1 Ayalew Jejaw Zeleke,2 Masresha Seyoum,3 Ligabaw Worku2
1Department of Medical Laboratory Sciences, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 2Department of Medical Parasitology, School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 3University of Gondar Referral Hospital Laboratory, University of Gondar, Gondar, Amhara Regional State, Ethiopia
Correspondence: Tahir Eyayu
Department of Medical Laboratory Sciences, College of Health Sciences, Debre Tabor University, Debre Tabor, PO Box 272 Ethiopia
Tel +251 933512423
Email [email protected]
Purpose: To assess basic coagulation profiles and platelet count among Schistosoma mansoni-infected and non-infected adults.
Patients and Methods: A comparative cross-sectional study was conducted from February to April 2019 at Sanja Primary Hospital, northwest Ethiopia. A total of 200 adults (100 cases and 100 controls) were enrolled using convenient sampling technique. Both wet mount and Kato-Katz techniques were performed using a stool sample. The venous blood sample was collected to perform platelet count, basic coagulation and serological tests. The data were coded and entered into EpiData Manager (v4.4.2.1) and analyzed using SPSS version 20. Nonparametric tests were used during data analysis. P-value less than 0.05 was considered as statistically significant.
Results: Prothrombin time (PT), activated partial thromboplastin time (APTT) and international normalization ratio (INR) were significantly higher while the platelet count was significantly lower in S. mansoni-infected than healthy adults (P < 0.001). There were statistically significant differences in the median [IQR] value of PT, APTT, INR and platelet count between light, moderate and heavy infected groups (P < 0.05). Infection intensity had a positive correlation with basic coagulation profiles and a negative correlation with platelet count (P < 0.05) of S. mansoni-infected adults.
Conclusion: The prevalence of coagulation abnormality was higher in S. mansoni-infected adults than healthy controls. Coagulation test and platelet count should be used to monitor and manage schistosomiasis-related complications.
Keywords: Schistosoma mansoni, basic coagulation profiles, platelet count, northwest Ethiopia
Background
Schistosomiasis is a parasitic disease caused by blood-dwelling trematode of the genus Schistosoma. Three main species of schistosomes that infects human beings are Schistosoma mansoni, Schistosoma haematobium, and Schistosoma japonicum. Schistosoma mansoni causes intestinal and hepatic schistosomiasis in Africa, the Middle East, and South America.1 In Africa, an estimated 660 million people were at risk of schistosomiasis and around 201.5 million infected individuals were estimated.2 Almost 300,000 people die annually due to schistosomiasis in Africa alone.3 The pooled prevalence of S. mansoni among the Ethiopian population was 18.7% and the prevalence has been increasing over the past 15 years.4
Hemostasis is the physiological process which consists of a combination of cellular and biochemical events to maintain blood in the fluid state and prevent the escape of blood through clot formation. It depends on the balance among several complex regulated systems that consist of the vascular, coagulation, fibrinolytic system, and platelets. Those systems work together to prevent excessive bleeding and clotting problem. The coagulation system is involved in the conversion of soluble fibrinogen into fibrin clot and consists of various protein factors produced by the liver.5,6 Platelets are a component of blood with no cell nucleus which play a role in the process of stopping bleeding at the site of interrupted endothelium through platelet adhesion, aggregation, and activation of the coagulation system.7,8
Primary hemostasis consists of the activation of blood platelets that can be triggered by endothelial damage and the formation of a platelet plug. Activated platelets release adenosine diphosphate (ADP), which induce vasoconstriction, stimulate secondary coagulation, and promote further platelet activation and aggregation.6 Schistosomes use different mechanisms to prevent primary hemostasis. The schistosome tegument contains several enzymatic activities that lead to the degradation of ADP. This results in inhibition of ADP-mediated platelet activation and aggregation.9–11 In this manner, the enzyme expressed at the tegumental surface helps to limit blood clot formation around the worms by acting as an anticoagulant and permit the parasites free movement within the vasculature.11
Coagulation factors play a role in secondary hemostasis in conjugation with platelet and vascular endothelium. Two pathways are involved. The intrinsic pathway is activated by binding of coagulation factor XII to collagen or negatively charged foreign substances. The extrinsic pathway is induced by tissue factor, which is expressed in endothelial tissue.6 The presence of the adult worm in the vein and extravasation of schistosome eggs causes an obstruction in blood vessels and induces endothelial dysfunction or damage, which plays a role in the activation of the extrinsic pathway.12 Both the extrinsic and the intrinsic pathway lead to the activation of thrombin. The S. mansoni tegument antigen can inhibit the proteolytic activity of thrombin, a central component in the coagulation cascade. The inhibition of thrombin activity is a potential strategy to prevent the formation of fibrin clots around the adult parasite.13
Schistosomiasis is associated with consistent hematologic changes. Adult worms and eggs are potential activators of blood coagulation by disturbing blood flow and endothelial function, which leads to hypercoagulability. Schistosomiasis patients have elevated levels of coagulation activation markers and extensive fibrin deposition over hepatic egg granulomas, which indicates the persistent activation of the coagulation system and thrombin generation throughout the advanced stage of the disease.14
In contrast, studies showed that patients have a reduced level or activity of different coagulation factors, fibrinogen, and regulatory proteins. Therefore, increased consumption of coagulation factors and decreased hepatic synthesis of these factors due to liver abnormality result in hypocoagulable state on patients.14 As the disease progresses, there may be massive hepatosplenomegaly associated with anemia, thrombocytopenia and coagulation disorder.15
Schistosomiasis exhibits high morbidity and mortality associated with periportal fibrosis, portal hypertension, and splenomegaly. Blood clotting abnormalities are associated with reduced liver function and increased liver fibrosis. Around 5–7% of patients infected by S. mansoni progress to the most severe form of Hepatosplenic Schistosomiasis (HSS) and a quarter of patients with HSS have hyperfibrinolysis, a severe blood clotting disorder which may increase their risk of gastrointestinal bleeding.16 Around 25–50% of patients showed a decrease in platelet count. Thrombocytopenia has been reported among 75% of patients with more advanced disease.17
However, studies regarding the effect of S. mansoni infection on basic coagulation profiles and platelet count among infected adults was not conducted in our country, even though the prevalence is high. Therefore, this study was aimed to assess basic coagulation profiles and platelet count among S. mansoni infected adults.
Patients and Methods
Study Design, Period, Area and Population
An institution-based comparative cross-sectional study was conducted at Sanja Primary Hospital from February to April 2019. Sanja district is located 65 km northwest of Gondar town and 792 km from Addis Ababa. The district has a population of 26,000 people located on altitude of 1800 m above sea level. Its annual rainfall and average temperature range from 800 to 1800 mm and 25°C to 42°C, respectively.18 In Sanja town there are one hospital, one health center, and five private clinics that provide health care service. Sanja town is traversed by one river and one stream, namely, Sanja River and Maho stream, which serve as sources of water for bathing, washing clothes, and other domestic and recreational purposes. They may constitute the major sources of S. mansoni infection.
The study populations were S. mansoni-infected and non-infected adults. Pregnant women, adults with multiple parasite infections, adults who were on anticoagulant therapy, adults having a history of chronic disease like hypertension, cardiac disease, and diabetes mellitus, chronic renal disease and inherited bleeding disorders, adults who were positive for human immunodeficiency viruses (HIV), hepatitis B surface antigen test (HBsAg) and hepatitis C virus (HCV), those who were smokers and alcohol abuse were excluded from the study for all groups.
Sample Size Determination and Sampling Technique
According to rules of thumb that have been recommended by van Voorhis and Morgan, 30 participants per group are required to detect real differences, which lead to about 80% power.19 To increase the accuracy of the study, the study participants recommended by the rule of thumb has to be increased by more than three-fold. Thus, 200 study participants (100 S. mansoni-infected and 100 healthy adults who were sex and age match control) were enrolled in the study. A convenience sampling technique was used to select study participants. All clinically suspected individuals for intestinal parasite infection and full fill the inclusion criteria who presenting themselves to Sanja Primary Hospital general outpatient department (OPD) were enrolled in the case group. All health-seeking individuals attending at VCT clinic of Sanja Primary Hospital and who fulfill the inclusion criteria was enrolled in control group.
Data Collection Procedure
Questionnaire Survey
Sociodemographic characteristics of study participant were collected using a pretested structured questionnaire written in Amharic (the local language). Trained clinicians who were working at Sanja Primary Hospital general OPD and VCT clinic assessed clinical information and patient history.
Sample Collection and Laboratory Analysis
Stool examination: - A single stool specimen of about 5gm was collected from each study participant. A clean, dry, and leak-proof container, which labeled with a unique ID number was used to collect the sample. First, each stool specimen was examined using direct wet mount technique and then double Kato-Katz slides were prepared on a template holding 41.7 mg of stool. Eggs counted for S. mansoni were recorded and later converted into eggs per gram (EPG) of stool, multiplying by a factor of 24. Finally, Infection intensity (light, moderate, and high) was classified according to WHO criteria.20
Blood sample collection: - Five milliliters (mL) of venous blood was collected by following standard operating procedures. The collected blood sample was dispensed into two test tubes. The first 2.7 mL of the collected blood sample was transferred into 0.3 mL of the 3.2% sodium citrate anticoagulated test tube. Platelet-poor plasma was obtained by centrifuging at 1500 rpm for 15 minutes for PT and APTT analysis. The remaining 2.3 mL blood was transferred into EDTA test tube for platelet count. The plasma left after platelet count was used for serological testing including HBsAg, HCV, HIV tests.
Urine sample collection:- Urine was collected using a clean urine cup from all women study participants to screen pregnancy.
Platelet count was determined using BS-Kt6200 3-Part Laboratory Fully Auto Hematology Analyzer (Guangzhou Bisen Medical Co., Ltd. Guangzhou, China).
Basic coagulation profiles (PT, APTT, and INR) were determined using HumaClot Dueplus coagulation analyzer (Wiesbaden, Germany). The HumaClot Dueplus is a highly sensitive 2-channel photo-optical instrument that offers clotting, chromogenic and immunoturbidimetric testing capabilities.
Serological tests: - HBsAg and HCV antibody tests were determined by using colloidal gold enhanced immune- chromatographic assay (Cortez Diagnostics RapidCard™ InstaTest Test device for HBsAg and The HCV RapiCard™ for HCV antibody; Cortez Diagnostic, Inc. China,). Both tests have more than 98.7% specificity and sensitivity.
Human immune deficiency virus testing: - to exclude HIV/AIDS patients HIV screening test was carried out using Stat pack, Abon, and SD bioline HIV 1/2 antibody screening test kit and following the manufacturer’s instruction. The test had 99% sensitivity and 100% specificity.
Urine HCG test: - to exclude pregnant women urine HCG (human chorionic gonadotropin) test was determined for both the cases and control group by using a rapid chromatographic immunoassay test strip (Guangzhou Wondfo Biotech Co Ltd, Guangzhou, China) which detects the HCG concentrations greater than 20 mIU/mL in a urine sample.
Data Quality Control
To maintain the quality of data, appropriate training was given for data collectors. To ensure the accuracy of the egg counts conducted by laboratory technologists, quality control was performed by re-reading all slides by an expert laboratory technologist. Standard operating procedures and manufacturer instructions were strictly followed throughout the procedures and all reagents were stored and prepared according to the manufacturer’s instruction.
Data Management and Analysis
Data were coded and entered into EpiData Manager (v4.4.2.1) statistical software and then exported to SPSS version 20 for analysis. Homogeneity of variance was checked by using Levene’s statistics. The Kolmogorov–Smirnov and Shapiro–Wilk normality test was used for checking the distribution of continuous variables, and it revealed that the data were not normally distributed for each group. Nonparametric tests, Mann-Witney U-test, Kruskal Wallis H and Dunn-Bonferroni pairwise were used for comparison of basic coagulation profiles and platelet count between groups. Spearman’s rank correlation analysis was used to assess the correlation of variables. The results were presented as the median and interquartile range (IQR) for each group. In all statistical analysis, p-value < 0.05 was considered as statistically significant.
Results
General Characteristics of Study Participants
A total of 200 participants (100 cases and 100 controls) were included in the study. The median age of the study subject was 27 years old (IQR: 12 years old) and 103 (51.5%) were males. The majority of study participants were orthodox in religion 183 (91.5%), living in rural area 114 (57%) and farmers 55 (27.5%). Socio-demographic data explored by using chi-square showed that there is no significant association between socio-demographic data and S. mansoni infection (Table 1).
|
Table 1 Socio-Demographic Characteristics of Study Participants at Sanja Primary Hospital General OPD and VCT Clinic, 2019 |
Intensity of S. mansoni Infection
The overall median of EPG of stool was 204. The median of EPG in males and females were 228 and 192, respectively, and the difference was not statistically different (p = 0.95). From a total of 100 S. mansoni-infected adults 40 (40.0%), 24 (24.0%) and 36 (36.0%) were due to light, moderate and heavy infection, respectively.
Prevalence of Abnormal Coagulation Profiles and Platelet Count Among Case and Control Groups
The percentages of prolonged PT, INR, APTT, and thrombocytopenia were higher in S. mansoni-infected adults than in healthy controls. Among S. mansoni-infected adults, 55 (55%), 41 (41%) and 37 (37%) had prolonged PT, INR, and APTT respectively. Moreover, 24 (24%) of S. mansoni-infected adults had thrombocytopenia. On the other hand, 8 (8%), 4 (4%) and 7 (7%) had prolonged PT, INR, and APTT, respectively among healthy controls. Also, only 3 (3%) had thrombocytopenia (Figure 1).
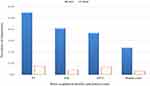 |
Figure 1 Prevalence of abnormal coagulation profiles and platelet count of study participants at Sanja Primary Hospital, 2019. |
Comparison of Basic Coagulation Profiles and Platelet Count Among Study Groups
In the healthy control group, the median [IQR] values of PT, APTT, INR, and platelet count were 13.5 [1.5], 31.2 [3.18] seconds, 1.13 [0.08] and 268.0 [81] × 103/μL, respectively. The median [IQR] values of PT, APTT, INR, and platelet count were 14.25 [3.2], 34.3 [5.73] seconds, 1.21 [0.32] and 199 [93] × 103/μL for S. mansoni-infected adults, respectively.
Since data were not normally distributed, a non-parametric test (Mann-Witney U-test) was used to compare the median difference in basic coagulation profiles and platelet count between cases and controls. A Mann-Witney U-test revealed a significant difference in the median of PT, INR, APTT, and platelet count of S. mansoni-infected adults and healthy control subjects (p <0.001).
Kruskal–Wallis H-test revealed that the median [IQR] of PT, INR, APTT, and platelet count showed statistically significant difference among healthy controls, light, moderate and heavy infected groups (p <0.001 in each). The heavy infected group recorded the highest median score of PT, INR, and APTT and the lowest median value of platelet count than the other groups (Table 2).
|
Table 2 Comparison of Basic Coagulation Profiles and Platelet Count Among Study Groups at Sanja Primary Hospital, 2019 |
In multiple pairwise comparisons analysis using Dunn-Bonferroni pairwise comparison test, the median [IQR] values of PT, INR, and APTT of heavily infected adults were significantly higher than the healthy controls and lightly infected adults (p < 0.05). Also, the median [IQR] value of platelet count was significantly lower in heavily infected adults compared to healthy controls and lightly infected adults (p <0.001). On the contrary, the median [IQR] value of PT, INR, and APTT did not show significant differences between healthy controls and lightly infected, lightly and moderately infected and between moderately and heavily infected adult groups (p > 0.05). Similarly, platelet count did not show significant differences between lightly and moderately infected and between moderately and heavily infected adult groups (p > 0.05) (Table 3).
|
Table 3 Multiple Pairwise Comparisons of Basic Coagulation Profiles and Platelet Count Among Study Groups at Sanja Primary Hospital, 2019 |
Correlation of Infection Intensity with Basic Coagulation Profiles and Platelet Counts
In S. mansoni-infected adults, Spearman’s rank-order correlation analysis showed that number of S. mansoni eggs per gram of stool had been significantly and positively correlated with basic coagulation profiles (PT, INR, and APTT) (Spearman’s rho correlation coefficient r= 0.477, 0.463, and 0.332, respectively; p <0.05) (Figure 2A–C). Additionally, platelet count of S. mansoni-infected adults was significantly and negatively correlated with a number of S. mansoni eggs per gram of stool (Spearman’s rho correlation coefficient r= −0.394; p <0.001) (Figure 2D).
Discussion
In our study, 40 (40.0%), 24 (24.0%) and 36 (36.0%) S. mansoni-infected adults were light, moderate and heavy intensity of infection, respectively. This is in line with the study conducted in South Omo Zone, Ethiopia regarding the heavy intensity of infection (40.0%).21 Our prevalence of heavy infection was higher than the prevalence reported from North-Western Tanzania and central Kenya, which was 9.7% and 20.6% respectively. Additionally, the prevalence of light infection reported in our study was lower than the ones seen in North-Western Tanzania and central Kenya, that were 75.0% and 47.7%, respectively.22,23 These differences may be due to the fact that other studies are community-based studies, while our study was institutional-based study.
Our finding showed that PT, INR, and APTT were significantly higher in S. mansoni-infected subjects than in negative controls (p < 0.001). This finding is concordant with studies set in China,24 Brazil16,25 and Egypt26–28 that found statistically significant prolonged PT, INR and/or APTT in S. mansoni-infected adults comparing to healthy controls. However, our findings were discordant with a study done in Sudan which did not find a significant difference in PT value between S. mansoni-infected adults and healthy controls (p >0.05).29 This variation may be due to the difference in study participants, the intensity of infection and the use of a small sample size in Sudanese study. Different factors including Schistosomiasis associated periportal were the possible reason for the occurrence of coagulation system abnormality in S. mansoni-infected individuals.14,30
This study revealed that the platelet count had significantly decreased in S. mansoni-infected adults compared to healthy controls (p < 0.001). This is in agreement with researches conducted in Brazil,16,25,31,32 in China,24 and Egypt26,27 which found significantly low platelet count in schistosomiasis patients compared to the healthy controls. Thrombocytopenia in schistosomiasis patients may occur because of splenic retention due to poor portal blood drainage, or platelets are trapped in the sinusoidal spaces of the fibrotic liver.33
Interestingly, our findings showed that there was a statistically significant difference in the median of PT, INR, and APTT among healthy controls, light, moderate and heavy infected groups. The heavy infection group recorded a significantly higher median score of PT, INR, and APTT than the healthy controls and light infection group. In schistosomiasis, eggs are the cause of pathology, which results chronic inflammation that leads to tissue fibrosis and chronic morbidity of schistosomiasis.34 Different researches concluded that the spectrum of clinical manifestations, disease progression, organ-specific clinical symptoms and complications in schistosomiasis often positively correlate and mainly depends on the intensity of infection, as indicated by excreted egg counts.34–36
In heavy infections, continuous granuloma formation and fibrosis together with elevated portal pressure lead to the development of hepatosplenomegaly, which causes liver function imbalance. The more severe disease is usually associated with heavy intensity infections.34,35 This might be the possible reason for the higher median score and prolonged value of PT, INR, and APTT in heavily infected adults.
In the current study, we found that platelet count was significantly different among the healthy controls, light, moderate and heavy intensity of infection groups (p = 0.001). The heavily infected group recorded a significantly lower median score of platelet count than the healthy controls and light infection group. The result of this finding was supported by a study conducted in Brazil, which found schistosomiasis patients had lower platelet count when the severity of disease increases.31 As the disease progresses, there may be massive hepatosplenomegaly associated with anemia, thrombocytopenia and coagulation disorder,15,30 which results in the occurrence of lower platelet count when the severity of S. mansoni infection increases.
These findings were confirmed by Spearman’s rank order correlation test, where the number of S. mansoni EPG of stool had a positive correlation with basic coagulation profiles (PT, INR, and APTT) and a negative correlation with platelet count (p <0.05) of S. mansoni-infected adults. The possible scientific reason for this correlation was due to schistosomiasis disease progression and complications, which often positively correlate with the intensity of the infection, as indicated by excreted egg counts.34–36
Adult S. mansoni and its eggs induce alteration in endothelial function or cause endothelial damage and disturbing blood flow, which plays a role in the activation of blood coagulation. Besides, schistosomes have many electronegative charges on their tegument that could potentially activate platelets and coagulation cascade, leading to hypercoagulation. Schistosomiasis patients had elevated levels of coagulation activation markers and observation of extensive fibrin deposition over hepatic egg granulomas, which indicates the persistent activation of the coagulation system and thrombin generation throughout the advanced stage of the disease. Therefore, increased consumption of coagulation factors and decreased hepatic synthesis of these factors due to liver abnormality were the possible reason for the occurrence of prolonged PT, INR and APTT in S. mansoni-infected adults.14,30
Limitations of the Study
In this study, only basic coagulation parameters such as PT, APTT, INR, and platelet count were measured to assess coagulation profiles and platelet count. The study did not include ultrasound examination, so it has a limitation in assessing the state of the liver of infected patients.
Conclusions
In the present study coagulation abnormality was higher in S. mansoni-infected adults than healthy controls. Prolonged PT, APTT, INR, and low platelet count were found in S. mansoni-infected adults. The intensity of S. mansoni infection had a positive correlation with basic coagulation profiles (PT, INR, and APTT) and a negative correlation with platelet count.
Abbreviations
APTT, Activated Partial Thromboplastin Time; EPG, Eggs per Gram; HBsAg, Hepatitis B Surface Antigen; HCV, Hepatitis C Virus; HIV, Human Immunodeficiency Virus; HSS, Hepatosplenic Schistosomiasis; INR, International Normalization Ratio; IQR, Interquartile Range; OPD, Out Patient Department; PT, Prothrombin Time; VCT, Voluntary Counseling and Testing.
Data Sharing Statement
The authors confirmed that all the data for this manuscript are available; if someone wants to request the data they can contact the corresponding author.
Ethics and Consent Statement
The study was approved by the School of Biomedical and Laboratory Sciences Research and Ethical Review Committee (reference no. SBMLS/2123/11). A letter of support was secured from woreda health office and permission letter was obtained from the clinical director of the hospital. Written informed written consent was taken from the study participants. Any individuals who were positive for different infections and had coagulation abnormality were linked to the responsible body in Sanja Primary Hospital for treatment. This study was conducted in accordance with the declaration of Helsinki.
Acknowledgment
We acknowledge the study participants, our colleagues and all staff members of Sanja Primary Hospital.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Gryseels B, Polman K, Clerinx J, Kestens L. Human schistosomiasis. Lancet. 2006;368(9541):1106–1118. doi:10.1016/S0140-6736(06)69440-3
2. Hotez PJ, Fenwick A. Schistosomiasis in Africa: an emerging tragedy in our new global health decade. PLoS Negl Trop Dis. 2009;3(9):e485. doi:10.1371/journal.pntd.0000485
3. Olveda DU, Li Y, Olveda RM, et al. Bilharzia: pathology, diagnosis, management and control. Trop Med Surg. 2013;1(4):135. doi:10.4172/2329-9088.1000135
4. Assegu D, Shimelis T. Prevalence of Schistosoma mansoni infection in Ethiopia: a systematic review and meta-analysis. BioRxiv. 2019;610113.
5. Ogedegbe HO. An overview of hemostasis. Lab Med. 2002;33(12):948–953. doi:10.1309/50UQ-GUPF-W6XW-1X7B
6. Palta S, Saroa R, Palta A. Overview of the coagulation system. Indian J Anaesth. 2014;58(5):515–523. doi:10.4103/0019-5049.144643
7. Hou Y, Carrim N, Wang Y, Gallant RC, Marshall A, Ni H. Platelets in hemostasis and thrombosis: novel mechanisms of fibrinogen-independent platelet aggregation and fibronectin-mediated protein wave of hemostasis. J Biomed Res. 2015;29(6):437–444.
8. Da’dara AA, Skelly PJ. Schistosomes versus platelets. Thromb Res. 2014;134(6):1176–1181. doi:10.1016/j.thromres.2014.09.032
9. Bhardwaj R, Skelly PJ. Purinergic signaling and immune modulation at the schistosome surface? Trends Parasitol. 2009;25(6):256–260. doi:10.1016/j.pt.2009.03.004
10. Da’dara AA, Bhardwaj R, Skelly PJ. Schistosome apyrase SmATPDase1, but not SmATPDase2, hydrolyses exogenous ATP and ADP. Purinergic Signal. 2014;10(4):573–580. doi:10.1007/s11302-014-9416-5
11. Elzoheiry M, Da’dara AA, El-Beshbishi SN, Skelly PJ. The essential ectoenzyme SmNPP5 from the human intravascular parasite schistosoma mansoni is an ADPase and a potent inhibitor of platelet aggregation. Thromb Haemost. 2018;118(06):979–989. doi:10.1055/s-0038-1641715
12. Da’dara A, Skelly PJ. Manipulation of vascular function by blood flukes? Blood Rev. 2011;25(4):175–179. doi:10.1016/j.blre.2011.04.002
13. Lin Y-L, He S. Sm22. 6 antigen is an inhibitor to human thrombin. Mol Biochem Parasitol. 2006;147(1):95–100. doi:10.1016/j.molbiopara.2006.01.012
14. Tanabe M. Haemostatic abnormalities in hepatosplenic schistosomiasis mansoni. Parasitol Int. 2003;52(4):351–359. doi:10.1016/S1383-5769(03)00051-5
15. Roberts DJ. Hematologic changes associated with specific infections in the tropics. Hematol Oncol Clin. 2016;30(2):395–415. doi:10.1016/j.hoc.2015.11.007
16. Leite LAC, Pimenta Filho AA, da Fonseca CSM, et al. Hemostatic dysfunction is increased in patients with hepatosplenic schistosomiasis mansoni and advanced periportal fibrosis. PLoS Negl Trop Dis. 2013;7(7):e2314. doi:10.1371/journal.pntd.0002314
17. Correia MC, Domingues AL, Lacerda HR, et al. Platelet function and the von Willebrand factor antigen in the hepatosplenic form of schistosomiasis mansoni. Trans R Soc Trop Med Hyg. 2009;103(10):1053–1058. doi:10.1016/j.trstmh.2008.11.017
18. CAC. Summary and statistical report of the 2007 population and housing census Addis Ababa. Population and Housing Census Commission; 2008:57–60.
19. VanVoorhis CW, Morgan BL. Understanding power and rules of thumb for determining sample sizes. Tutor Quant Methods Psychol. 2007;3(2):43–50. doi:10.20982/tqmp.03.2.p043
20. Montresor A, Crompton DWT, Hall A, et al. Guidelines for the Evaluation of Soil-Transmitted Helminthiasis and Schistosomiasis at Community Level: A Guide for Managers of Control Programmes. Geneva: World Health Organization; 1998:1–48.
21. Girma M, Agedew E, Gedeamu G, Haftu D, Yohanes T. Prevalence of Schistosoma mansoni infection and associated factors in irrigation workers in Gamo Gofa and South Omo Zone, 2017: a Community based parasitological survey. J Parasitol Vector Biol. 2018;13:17.
22. Masaku J, Mutungi F, Gichuki PM, Okoyo C, Njomo DW, Njenga SM. High prevalence of helminths infection and associated risk factors among adults living in a rural setting, central Kenya: a cross-sectional study. Trop Med Health. 2017;45(1):15. doi:10.1186/s41182-017-0055-8
23. Mazigo HD, Nuwaha F, Dunne DW, et al. Schistosoma mansoni infection and its related morbidity among adults living in selected villages of Mara Region, North-Western Tanzania: a cross-sectional exploratory study. Korean J Parasitol. 2017;55(5):533–540. doi:10.3347/kjp.2017.55.5.533
24. Shun L, Meng Q, Shao-Qian T. Analysis of coagulation related parameters between patients with advanced schistosomiasis cirrhosis and hepatitis B cirrhosis. Chin J Schistosomiasis Control. 2016;29(1):68–71. doi:10.16250/j.32.1374.2016159
25. Leite LAC, Domingues ALC, Lopes EP, et al. Relationship between splenomegaly and hematologic findings in patients with hepatosplenic schistosomiasis. Rev Bras Hematol Hemoter. 2013;35(5):332–336. doi:10.5581/1516-8484.20130098
26. El-Bassiouni N, El AB, Hussein N, et al. The coagulation profile in hepatosplenic schistosomiasis. Blood Coagul Fibrinolysis. 1998;9(2):189–194. doi:10.1097/00001721-199803000-00011
27. El-Bassiouni N, El Bassiouny A, Akl M, El-Khayat H. Fibronectin, platelet factor 4 and beta-thromboglobulin in endemic hepatosplenic schistosomiasis: relation to acute hematemesis. Pathophysiol Haemost Thromb. 1997;27(1):39–48. doi:10.1159/000217432
28. Essawy FM, Bekheet IW, Saleh AF, Madkour ME, Bayoumi EE-DA. Impact of neutrophil apoptosis on haemostatic activation in chronic liver disease patients. Blood Coagul Fibrinolysis. 2008;19(6):535–542. doi:10.1097/MBC.0b013e3283079e15
29. Osman MA. Evaluation of Some Haemostatic Parameter Among Schistosomiasis Parameters in Algleea Village–Shendi. Sudan University of Science and Technology; 2012.
30. Mebius MM, van Genderen PJ, Urbanus RT, Tielens AG, de Groot PG, van Hellemond JJ. Interference with the host haemostatic system by schistosomes. PLoS Pathog. 2013;9(12):e1003781. doi:10.1371/journal.ppat.1003781
31. KÖPKE‐AGUIAR L, dE Leon C, Shigueoka D, Lourenço D, Kouyomdjian M, Borges D. Reticulated platelets and thrombopoietin in schistosomiasis patients. Int J Lab Hematol. 2009;31(1):69–73. doi:10.1111/j.1751-553X.2007.01005.x
32. Drummond SC, Pereira PN, Otoni A, Chaves BA, Antunes CM, Lambertucci JR. Thrombocytopenia as a surrogate marker of hepatosplenic schistosomiasis in endemic areas for Schistosomiasis mansoni. Rev Soc Bras Med Trop. 2014;47(2):218–222. doi:10.1590/0037-8682-0020-2014
33. de Araújo Souza MR, De Toledo CF, Borges DR. Thrombocytemia as a predictor of portal hypertension in schistosomiasis. Dig Dis Sci. 2000;45(10):1964–1970. doi:10.1023/A:1005535808464
34. Burke M, Jones M, Gobert G, Li Y, Ellis M, McManus D. Immunopathogenesis of human schistosomiasis. Parasite Immunol. 2009;31(4):163–176. doi:10.1111/j.1365-3024.2009.01098.x
35. McManus DP, Dunne DW, Sacko M, Utzinger J, Vennervald BJ, Zhou X-N. Schistosomiasis. Nat Rev Dis Primers. 2018;4(1):13. doi:10.1038/s41572-018-0013-8
36. Weerakoon KG, Gobert GN, Cai P, McManus DP. Advances in the diagnosis of human schistosomiasis. Clin Microbiol Rev. 2015;28(4):939–967. doi:10.1128/CMR.00137-14
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

