Back to Journals » Clinical Interventions in Aging » Volume 10
Bariatric surgery in elderly patients: a systematic review
Authors Giordano S, Victorzon M
Received 16 June 2015
Accepted for publication 18 September 2015
Published 13 October 2015 Volume 2015:10 Pages 1627—1635
DOI https://doi.org/10.2147/CIA.S70313
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Walker
Salvatore Giordano,1 Mikael Victorzon2,3
1Department of Plastic and General Surgery, Turku University Hospital, Turku, 2Department of Gastrointestinal Surgery, Vaasa Central Hospital, Vaasa, 3University of Turku, Turku, Finland
Abstract: Controversy exists regarding the effectiveness and safety of bariatric/metabolic surgery in elderly patients. We performed a systematic review on this issue in patients aged 60 years or older. MEDLINE, Cochrane Library, Embase, Scopus, and Google Scholar were searched until August 2015 for studies on outcomes of bariatric surgery in elderly patients. The results were expressed as pooled proportions (%) with 95% confidence intervals. Heterogeneity across the studies was evaluated by the I2 test, and a random-effects model was used. Twenty-six articles encompassing 8,149 patients were pertinent with this issue and included data on bariatric surgery outcomes in elderly population. Fourteen patients died during the 30-day postoperative period, with a pooled mortality of 0.01%. Pooled overall complication rate was 14.7%. At 1-year follow-up, pooled mean excess weight loss was 53.77%, pooled diabetes resolution was 54.5%, and pooled hypertension resolution was 42.5%, while pooled lipid disorder resolution was 41.2%. Outcomes and complication rates of bariatric surgery in patients older than 60 years are comparable to those in a younger population, independent of the type of procedure performed. Patients should not be denied bariatric surgery because of their age alone.
Keywords: morbid obesity, bariatric surgery, elderly, gastric bypass, weight loss, laparoscopy
Introduction
Life expectancy has been steadily increasing regardless of sex and ethnic background in the USA.1 In Finland, life expectancy of a 60-year-old woman in 2008 was 24.3 years, whereas for a man of the same age, it was 22.8 years.2
Obesity is known to decrease the quality of life as well as life expectancy,3 and bariatric/metabolic surgery is the most effective treatment for morbid obesity.4 The efficacy of bariatric procedures in the induction and maintenance of weight loss is largely superior to that obtainable by current medical therapies.4 Surgery results in greater weight loss and improvement in weight-associated comorbidities compared with nonsurgical interventions, regardless of the type of procedure used.4
Several studies have compared weight loss outcomes between different types of bariatric surgeries,5 or different techniques of the same procedure,6 whereas others have analyzed different preoperative predictors, with controversial results.7–11 Only few studies have aimed at analyzing the effects of age on weight loss in a sufficiently large cohort of patients undergoing the same bariatric operation, and long-term follow-up data are often lacking.
There is some evidence that elderly patients lose less weight and benefit less from bariatric surgery than younger patients.12,13 However, controversy exists regarding the indications and outcomes of bariatric/metabolic surgery in elderly patients. In some studies, younger bariatric patients have better comorbidity, mortality, and weight loss outcomes12,13 compared to older patients. Surgical indications for elderly patients should be carefully considered,12 although weight loss and reduction in comorbidities and mortality of patients older than 55 years might be comparable to the general bariatric surgery population.14–16
We performed a systematic review on this issue to summarize the current evidence in patients 60 years or older who have so far been considered high-risk patients.
Methods
A literature search was performed through MEDLINE, Cochrane Library, Embase, Scopus, and Google Scholar for any study written in English on bariatric and metabolic surgery in elderly patients. We applied Boolean searches to above-mentioned databases using the following search terms: morbid obesity, bariatric surgery, metabolic surgery, gastric bypass, sleeve gastrectomy, adjustable gastric banding, biliopancreatic diversion, duodenal switch, elderly, over 55/60 years, advanced age, and old.
The search was performed in August 2015, aiming at those studies showing outcomes of bariatric/metabolic surgery in patients aged 60 years or older. In addition, the reference lists of all relevant articles were searched. Only full-length articles written in English were considered for this systematic review.
A cutoff at 60 years of age was chosen, although the age of 55 has been commonly used to define older age in the bariatric literature.14–16 It was considered an appropriate cutoff for the purposes of this study, as the age of 55 is low in the non-bariatric surgery literature. Data were retrieved only from the articles, and no attempt was made to get missing data from the authors. We retrieved data on study size, type of intervention, excess weight loss (EWL) percentage, outcomes at 1-year follow-up, 30-day mortality, and diabetes, hypertension, and lipid disease resolution percentages at the minimum of 1-year follow-up.
Statistical analysis was performed using the freely downloadable software Open Meta-Analyst.17 The results were expressed as pooled proportions (%) with 95% confidence intervals (CIs). Heterogeneity across the studies was evaluated using the I2 test. Because heterogeneity was anticipated among the observational studies, the evaluation was made a priori by using a random-effects model (DerSimonian–Laird).
We followed the Preferred Reporting Items for Systematic and Meta-analysis statement for reporting this systematic review,18 and the language of the articles was defined as reported in MEDLINE.
Results
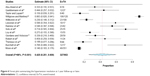
The literature search yielded 7,625 articles, 26 of which16,19–43 were pertinent to our study, and sources of reported outcomes of bariatric surgery in patients 60 years or older (Table 1). The literature search flowchart is shown in Figure 1. Different types of bariatric surgery procedures were involved. The analysis encompassed a total of 8,149 patients. Fourteen patients died during the 30-day postoperative period, with an untransformed proportion of 0.01% (95% CI 0.01–0.02; Figure 2). Pooled overall complication rate was 14.7% (95% CI 11.0–18.3; Figure 3), ranging from 1.33%39 to 47%.33
  | Figure 1 Flowchart summarizing literature search results. |
  | Figure 2 Forest plot summarizing the 30-day mortality. |
  | Figure 3 Forest plot summarizing the overall complications occurred. |
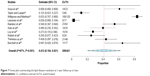
Pooled mean EWL% was 53.77% (95% CI 48.42–59.13; Figure 4), including 15 studies.
  | Figure 4 Forest plot summarizing the EWL% at 1-year follow-up or later. |
Seventeen studies showed results on diabetes resolution, ranging from 33%42 to 83%,33,40 with a pooled mean of 54.5% (95% CI 39.1–69.1; Figure 5).
  | Figure 5 Forest plot summarizing the diabetes resolution at 1-year follow-up or later. |
Similarly, 14 studies reported data on hypertension resolution, ranging from 14%43 to 88%,28 with a pooled mean of 42.5% (95% CI 25.1–60.0; Figure 6), while ten studies reported results on lipid disease resolution, ranging from 2.8%33 to 83%,28 with a pooled mean of 41.2% (95% CI 19.4–63.1; Figure 7).
  | Figure 6 Forest plot summarizing the hypertension resolution at 1-year follow-up or later. |
  | Figure 7 Forest plot summarizing the lipid disease resolution at 1-year follow-up or later. |
Discussion
This systematic review involving 8,149 patients provides a compelling insight into the value of bariatric surgery in patients 60 years or older. Our pooled analysis showed an overall low mortality and an acceptable complication rate (0.01% and 14.7%, respectively), while pooled EWL% was successful (53.77%; Figure 4) at 1-year follow-up in this population that has been considered high risk.
The prevalence of obesity among populations 60 years or older is likely to increase as the baby boomer generation continues to age. Thus, the number of elderly patients undergoing bariatric surgery is increasing.
Recent large studies have showed that body mass index and age are strong risk predictors for 30-day mortality in Laparoscopic Roux-en-Y Gastric Bypass (LRYGB) patients,44–46 demonstrating even a linear relationship between increasing body mass index and increasing age with mortality risk.45 However, the number of bariatric surgery procedures performed in elderly patients has been growing significantly during the past decade,39 with >10% of patients older than 60 years in the USA. Indeed, this patient volume increase has coincided with a reduction in mortality and perioperative morbidity.39
A large multicenter study demonstrated that older age predicts prolonged length of hospital stay but not major events following bariatric surgery, although a statistically nonsignificant trend toward predicting mortality was detected.46 More recently, Spaniolas et al47 demonstrated that in elderly population, sleeve gastrectomy is not associated with significantly different 30-day outcomes compared to LRYGB, and both procedures showed acceptably low morbidity and mortality rates.
Older patients might lose less weight because of impaired metabolic capacity and greater presence of sarcopenia compared to younger patients. They have suffered from associated comorbidities longer, which might have an influence in their baseline physical condition.13
Energy requirements normally decrease with age48 with a lower lipolytic capacity,49 especially after sympathetic stimulation.50 This might explain the increased adipose tissue deposition in older subjects. Reduced lipolytic activity has been described in obese, postmenopausal women subjected to a hypocaloric diet.51 These findings suggest that older obese women have a decreased capacity to use energy through the mobilization of lipids from fat stores, and this could also induce a larger caloric intake after surgery. This fact has recently been demonstrated measuring the short-term weight loss in women 20–45 years versus 55–65 years of age following bariatric surgery. The weight loss was significantly higher in younger women but not in men, indicating a role played by estrogens.52 On the other hand, a greater reduction in energy intake after LRYGB has been detected in younger patients.53
Total body energy expenditure begins to decline from the age of 40 years,54 and this age-dependent decrease is apparently due to a reduction in physical activity.55 The more sedentary lifestyle seems to be one reason for lower weight loss in patients older than 55 years.56 Younger patients may have more active lifestyles with better exercise tolerance, and it is well known that successful long-term weight maintenance is associated with a physically active lifestyle.57
As mentioned, the age of candidates for surgery is increasing.58 There is a detrimental impact of age on wound healing in all tissues. Aging intrinsically and extrinsically impacts the skin, leading to atrophy, progressive loss of function, increased vulnerability to the environment, and decreased homeostatic capability.59 At the microscopic level, there are decreased levels of growth factors, and diminished cell proliferation and migration. Diminished extracellular matrix slows wound healing.59 These factors together with higher comorbidity prevalence in elderly patients may explain the higher complication rates.
However, three recent reviews on this topic show a good weight loss efficacy in elderly with acceptable risks.14,60,61 We performed a pooled analysis in order to quantify those risks and show the achieved results.
Although outcomes might be worse than in younger patients,12,13 our pooled analysis demonstrated a significant EWL, and an overall improvement in the most common obesity-related comorbidities in patients ≥60 years (Figures 4–7). We concluded that elderly patients do benefit from bariatric surgery with acceptable rates of morbidity and mortality, which might justify taking a higher perioperative risk. In a recent statement, the Italian Society for Bariatric and Metabolic Surgery has extended the indications for bariatric surgery for morbidly obese patients up to 70 years of age.62
Age alone should not be an absolute contraindication for bariatric surgery. Indications should be carefully evaluated in the light of routine preoperative tests and discussed with the patients knowing that there are some risks, and that the results might not be as good as they might expect.
The current study has several limitations and potential bias influencing these findings.
There was a paucity of well-reported studies, and there were differences in what was considered elderly population, with discrepancies in lower age limit varying from 50 to 70 years. Most of the studies contained <100 patients. Furthermore, the reporting of confidence measures was poor, introducing further inaccuracy in our calculations. We did not attempt to show pooled results from different bariatric procedures as data were mostly unavailable, and the main aim of this review was to give a compelling picture of bariatric surgery in a population of 60 years or older.
The types of complications were mostly not classified. Only one study adopted the Clavien–Dindo Classification.16 Thus, we pooled together all major and minor complications in order to show the overall complication rate (Figure 3). Follow-up time and adherence were different among the studies, and the comorbidity resolution rates were measured at the last follow-up control. We did not attempt to analyze other conditions such as obstructive sleep apnea, joint disease, gastroesophageal reflux, depression, and asthma because of the paucity of reported data.
Conclusion
This systematic review supports the use of bariatric surgery in elderly patients. Older patients should not be denied an operation only because of their age. However, elderly patients should be carefully counseled about the slightly increased risks and the possibility of less satisfactory outcomes.
Acknowledgment
We thank Jaana Elberkennou, MD, MA, for her kind revision of the English language.
Disclosure
The authors have no conflicts of interests to declare.
References
Arias E. United States life tables, 2010. Natl Vital Stat Rep. 2014;63:1–63. | ||
Statistics Finland. Available from: http://pxweb2.stat.fi/database/statfin/vrm/kuol/kuol_fi.asp. Accessed June 7, 2015. | ||
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82. | ||
Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:CD003641. | ||
Angrisani L, Cutolo PP, Formisano G, Nosso G, Vitolo G. Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 10-year results of a prospective, randomized trial. Surg Obes Relat Dis. 2013;9(3):405–413. | ||
Stefanidis D, Kuwada TS, Gersin KS. The importance of the length of the limbs for gastric bypass patients – an evidence-based review. Obes Surg. 2011;21(1):119–124. | ||
Lutfi R, Torquati A, Sekhar N, Richards WO. Predictors of success after laparoscopic gastric bypass: a multivariate analysis of socioeconomic factors. Surg Endosc. 2006;20(6):864–867. | ||
Nguyen NT, Rivers R, Wolfe BM. Factors associated with operative outcomes in laparoscopic gastric bypass. J Am Coll Surg. 2003;197(4):548–555. | ||
Melton GB, Steele KE, Schweitzer MA, Lidor AO, Magnuson TH. Suboptimal weight loss after gastric bypass surgery: correlation of demographics, comorbidities, and insurance status with outcomes. J Gastrointest Surg. 2008;12(2):250–255. | ||
Harvin G, DeLegge M, Garrow DA. The impact of race on weight loss after Roux-en-Y gastric bypass surgery. Obes Surg. 2008;18(1):39–42. | ||
Desai MM, Zhang P, Hennessy CH. Surveillance for morbidity and mortality among older adults – United States, 1995–1996. MMWR CDC Surveill Summ. 1999;48(8):7–25. | ||
Scozzari G, Passera R, Benvenga R, Toppino M, Morino M. Age as a long-term prognostic factor in bariatric surgery. Ann Surg. 2012;256(5):724–728. | ||
Contreras JE, Santander C, Court I, Bravo J. Correlation between age and weight loss after bariatric surgery. Obes Surg. 2013;23(8):1286–1289. | ||
Lynch J, Belgaumkar A. Bariatric surgery is effective and safe in patients over 55: a systematic review and meta-analysis. Obes Surg. 2012;22(9):1507–1516. | ||
Frutos MD, Luján J, Hernández Q, Valero G, Parrilla P. Results of laparoscopic gastric bypass in patients > or =55 years old. Obes Surg. 2006;16(4):461–464. | ||
Giordano S, Victorzon M. Laparoscopic Roux-en-Y gastric bypass is effective and safe in over 55-year-old patients: a comparative analysis. World J Surg. 2014;38(5):1121–1126. | ||
Brodley CE, Lau J, Schmid CH, et al. Open Meta-Analyst. 2014. Available from: http://tuftscaes.org/open_meta/ | ||
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. | ||
Abu-Abeid S, Keidar A, Szold A. Resolution of chronic medical conditions after laparoscopic adjustable silicone gastric banding for the treatment of morbid obesity in the elderly. Surg Endosc. 2001;15(2):132–134. | ||
Sosa JL, Pombo H, Pallavicini H, Ruiz-Rodriguez M. Laparoscopic gastric bypass beyond age 60. Obes Surg. 2004;14(10):1398–1401. | ||
Quebbemann B, Engstrom D, Siegfried T, Garner K, Dallal R. Bariatric surgery in patients older than 65 years is safe and effective. Surg Obes Relat Dis. 2005;1(4):389–392. | ||
St Peter SD, Craft RO, Tiede JL, Swain JM. Impact of advanced age on weight loss and health benefits after laparoscopic gastric bypass. Arch Surg. 2005;140(2):165–168. | ||
Hazzan D, Chin EH, Steinhagen E, et al. Laparoscopic bariatric surgery can be safe for treatment of morbid obesity in patients older than 60 years. Surg Obes Relat Dis. 2006;2(6):613–616. | ||
Taylor CJ, Layani L. Laparoscopic adjustable gastric banding in patients > or =60 years old: is it worthwhile? Obes Surg. 2006;16(12):1579–1583. | ||
Trieu HT, Gonzalvo JP, Szomstein S, Rosenthal R. Safety and outcomes of laparoscopic gastric bypass surgery in patients 60 years of age and older. Surg Obes Relat Dis. 2007;3(3):383–386. | ||
Busetto L, Angrisani L, Basso N, et al; Italian Group for Lap-Band. Safety and efficacy of laparoscopic adjustable gastric banding in the elderly. Obesity (Silver Spring). 2008;16(2):334–338. | ||
Mittermair RP, Aigner F, Obermüller S. Results and complications after Swedish adjustable gastric banding in older patients. Obes Surg. 2008;18(12):1558–1562. | ||
Wittgrove AC, Martinez T. Laparoscopic gastric bypass in patients 60 years and older: early postoperative morbidity and resolution of comorbidities. Obes Surg. 2009;19(11):1472–1476. | ||
Wool D, Bellatorre N, Wren S, Eisenberg D. Male patients above age 60 have as good outcomes as male patients 50–59 years old at 1-year follow-up after bariatric surgery. Obes Surg. 2009;19(1):18–21. | ||
O’Keefe KL, Kemmeter PR, Kemmeter KD. Bariatric surgery outcomes in patients aged 65 years and older at an American Society for Metabolic and Bariatric Surgery Center of Excellence. Obes Surg. 2010;20(9):1199–1205. | ||
Willkomm CM, Fisher TL, Barnes GS, Kennedy CI, Kuhn JA. Surgical weight loss >65 years old: is it worth the risk? Surg Obes Relat Dis. 2010;6(5):491–496. | ||
Clough A, Layani L, Shah A, Wheatley L, Taylor C. Laparoscopic gastric banding in over 60s. Obes Surg. 2011;21(1):10–17. | ||
Leivonen MK, Juuti A, Jaser N, Mustonen H. Laparoscopic sleeve gastrectomy in patients over 59 years: early recovery and 12-month follow-up. Obes Surg. 2011;21(8):1180–1187. | ||
Ramirez A, Roy M, Hidalgo JE, Szomstein S, Rosenthal RJ. Outcomes of bariatric surgery in patients >70 years old. Surg Obes Relat Dis. 2012;8(4):458–462. | ||
Soto FC, Gari V, de la Garza JR, Szomstein S, Rosenthal RJ. Sleeve gastrectomy in the elderly: a safe and effective procedure with minimal morbidity and mortality. Obes Surg. 2013;23(9):1445–1449. | ||
Loy JJ, Youn HA, Schwack B, Kurian MS, Fielding GA, Ren-Fielding CJ. Safety and efficacy of laparoscopic adjustable gastric banding in patients aged seventy and older. Surg Obes Relat Dis. 2014;10(2):284–289. | ||
Robert M, Pasquer A, Espalieu P, Laville M, Gouillat C, Disse E. Gastric bypass for obesity in the elderly: is it as appropriate as for young and middle-aged populations? Obes Surg. 2014;24(10):1662–1669. | ||
Thereaux J, Poitou C, Barsamian C, Oppert JM, Czernichow S, Bouillot JL. Midterm outcomes of gastric bypass for elderly (aged ≥60 yr) patients: a comparative study. Surg Obes Relat Dis. 2015;11(4):836–841. | ||
Gebhart A, Young MT, Nguyen NT. Bariatric surgery in the elderly: 2009–2013. Surg Obes Relat Dis. 2015;11(2):393–398. | ||
Burchett MA, McKenna DT, Selzer DJ, Choi JH, Mattar SG. Laparoscopic sleeve gastrectomy is safe and effective in elderly patients: a comparative analysis. Obes Surg. 2015;25(2):222–228. | ||
Qin C, Luo B, Aggarwal A, De Oliveira G, Kim JY. Advanced age as an independent predictor of perioperative risk after laparoscopic sleeve gastrectomy (LSG). Obes Surg. 2015;25(3):406–412. | ||
Daigle CR, Andalib A, Corcelles R, Cetin D, Schauer PR, Brethauer SA. Bariatric and metabolic outcomes in the superobese elderly. Surg Obes Relat Dis. Epub 2015. | ||
Moon RC, Kreimer F, Teixeira AF, Campos JM, Ferraz A, Jawad MA. Morbidity rates and weight loss after Roux-en-Y gastric bypass, sleeve gastrectomy, and adjustable gastric banding in patients older than 60 years old: which procedure to choose? Obes Surg. Epub 2015 Jul 29. | ||
DeMaria EJ, Portenier D, Wolfe L. Obesity surgery mortality risk score: proposal for a clinically useful score to predict mortality risk in patients undergoing gastric bypass. Surg Obes Relat Dis. 2007;3(2):134–140. | ||
Benotti P, Wood GC, Winegar DA, et al. Risk factors associated with mortality after Roux-en-Y gastric bypass surgery. Ann Surg. 2014;259(1):123–130. | ||
Dorman RB, Abraham AA, Al-Refaie WB, Parsons HM, Ikramuddin S, Habermann EB. Bariatric surgery outcomes in the elderly: an ACS NSQIP study. J Gastrointest Surg. 2012;16(1):35–44. | ||
Spaniolas K, Trus TL, Adrales GL, Quigley MT, Pories WJ, Laycock WS. Early morbidity and mortality of laparoscopic sleeve gastrectomy and gastric bypass in the elderly: a NSQIP analysis. Surg Obes Relat Dis. 2014;10(4):584–588. | ||
Rand CS, Macgregor AM. Age, obesity surgery, and weight loss. Obes Surg. 1991;1(1):47–49. | ||
Toth MJ, Tchernof A. Lipid metabolism in elderly. Eur J Clin Nutr. 2000;54:S121–S125. | ||
Blaak EE, van Baak MA, Saris WH. Beta-adrenergically stimulated fat oxidation is diminished in middle-aged compared to young subjects. J Clin Endocrinol Metab. 1999;84(10):3764–3769. | ||
Nicklas BJ, Rogus EM, Goldberg AP. Exercise blunts declines in lipolysis and fat oxidation after dietary-induced weight loss in obese older women. Am J Physiol. 1997;273(1 pt 1):E149–E155. | ||
Ochner CN, Teixeira J, Geary N, Asarian L. Greater short-term weight loss in women 20–45 versus 55–65 years of age following bariatric surgery. Obes Surg. 2013;23(10):1650–1654. | ||
Bobbioni-Harsch E, Huber O, Morel P, et al. Factors influencing energy intake and body weight loss after gastric bypass. Eur J Clin Nutr. 2002;56(6):551–556. | ||
Manini TM. Energy expenditure and aging. Ageing Res Rev. 2010;9(1):1–11. | ||
Lührmann PM, Bender R, Edelmann-Schäfer B, Neuhäuser-Berthold M. Longitudinal changes in energy expenditure in an elderly German population: a 12-year follow-up. Eur J Clin Nutr. 2009;63(8):986–992. | ||
Ma Y, Pagoto SL, Olendzki BC, et al. Predictors of weight status following laparoscopic gastric bypass. Obes Surg. 2006;16(9):1227–1231. | ||
Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6(1):67–85. | ||
Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–908. | ||
Gosain A, DiPietro LA. Aging and wound healing. World J Surg. 2004;28(3):321–326. | ||
Caceres BA. Policy implications of a literature review of bariatric surgery in older adults. J Gerontol Nurs. 2014;40(9):14–19. | ||
Caceres BA, Moskowitz D, O’Connell T. A review of the safety and efficacy of bariatric surgery in adults over the age of 60: 2002–2013. J Am Assoc Nurse Pract. 2015;27(7):403–410. | ||
SICOB. Available from: http://www.sicob.org/00_materiali/attivita/statement_anziani.pdf. Accessed September 3, 2015. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

