Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Atypical Linear Atrophoderma of Moulin Complicated with Elevated Immunoglobulin M: A Case Report
Received 24 November 2022
Accepted for publication 5 January 2023
Published 21 January 2023 Volume 2023:16 Pages 193—196
DOI https://doi.org/10.2147/CCID.S398441
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Chenyu Tang,1 Ping Wang2
1Department of Dermatology, Hangzhou Third People’s Hospital, Zhejiang Chinese Medical University, Hangzhou, People’s Republic of China; 2Department of Dermatology, Hangzhou Third People’s Hospital; Affiliated Hangzhou Dermatology Hospital of Zhejiang University School of Medicine, Hangzhou, People’s Republic of China
Correspondence: Ping Wang, Department of Dermatology, Hangzhou Third People’s Hospital; Affiliated Hangzhou Dermatology Hospital of Zhejiang University School of Medicine, Westlake Ave 38, Hangzhou, People’s Republic of China, Tel +8613588812862, Email [email protected]
Abstract: Linear atrophoderma of Moulin (LAM) is a rare acquired skin disease. Clinically, LAM is characterized by hyperpigmented and atrophic unilateral band-like or linear dermatoses of variable size following the Blaschko lines. The lesions do not present induration or sclerosis. Its course is asymptomatic without systemic involvement or progression. The etiology of LAM is still unclear. Based on the characteristics of its skin lesions distributed along the Blaschko lines, some scholars speculate that its pathogenesis may be related to chromosome mosaicism. We hereby present a case report of LAM in a 29-year-old Chinese female who had persistent brown patches distributed along the Blaschko lines on the left lower back, buttocks, and lower limbs with positive antinuclear antibody (ANA, 1:320, nucleolar type) and elevated immunoglobulin M (3.47 g/L). Including this case, a total of 6 LAM cases have been reported to have abnormal serum immunological markers.
Keywords: linear atrophoderma of Moulin, atrophy, Blaschko lines
Introduction
LAM was first reported by Moulin in 1992. LAM is a rare acquired skin disease. López et al proposed the following diagnostic criteria for LAM:2 (1) onset from infancy to adolescence; (2) development of hyperpigmented, slightly atrophic, unilateral lesions following the Blaschko lines on the trunk or extremities; (3) lack of previous inflammation and subsequent absence of scleroderma; (4) stable and nonprogressive clinical course with no pattern of remission; and (5) histologic findings showing hyperpigmentation of the epidermis’ basal layer and normal dermis with unaffected connective tissue and elastic fibers. LAM is a self-limiting disease, and there is no standard treatment. Here, we report a case of atypical LAM that exhibited an inflammatory stage on histopathology accompanied by positive ANA and elevated IgM.
Case Presentation
The patient was a 29-year-old female treated at Hangzhou Third People’s Hospital on October 04, 2021. The patient complained that the lesions initially involved the left waist and abdomen without obvious inducement 16 years ago, and the light brown patches gradually expanded to the left buttocks and lower limbs with no obvious discomfort but a heavy psychological burden. During this period, there was no other development of the lesions, such as sclerosis, and she did not accept medical treatment. The patient had been in good health and denied a similar medical and genetic history in her family.
Systematic physical examination showed no abnormalities. The patient was previously healthy, and no hematological or immunodeficiency diseases were noted. Dermatological examination showed that there were banded brown patches distributed along the Blaschko lines on the left lower back, buttocks, and lower limbs, which were partially fused. The skin was not hard, the boundary was not clear, and the skin surface was smooth with mild atrophy when palpated (Figure 1). Laboratory tests showed positive antinuclear antibody (ANA, 1:320, nucleolar type) and elevated immunoglobulin M (3.47 g/L). Other laboratory test results were normal.
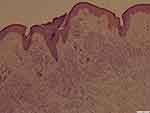
The lesion on the left lower extremity was removed for pathological biopsy, which showed that the epidermal mutation disappeared, the pigment particles in the basal layer were obvious, numerous lymphocytes infiltrated the dermis, and the elastic fibers and collagen fibers stained normally (Figure 2).
Based on the clinical manifestations and investigation findings, this patient was diagnosed with linear atrophoderma of Moulin. The patient did not show significant improvement after four months of treatment with oral administration of snow glucoside tablets and topical snow glucoside ointment.
Discussion
Combined with previous reports, we believe that the following diagnostic criteria can be added: (1) the disease can occur in middle age, (2) skin lesions can appear on the neck and head and are distributed along the Blaschko lines,3–5 and (3) histopathology can show inflammation and collagen alterations.1 In addition, there have been some reports of atypical LAM, which manifests as erythematous plaques, telangiectasias, and dissemination to the trunk and extremities.6
LAM needs to be differentiated from progressive idiopathic atrophy (PIA) and linear scleroderma.7 The skin lesions of PIA are similar to those of LAM, manifesting as pigmented atrophic patches but not along the Blaschko lines. While some scholars believe that LAM is a special type of PIA,8 linear scleroderma usually has skin inflammation and skin sclerosis accompanied by joint contracture and muscle weakness.9
Compared with the reported LAM cases, this case involved a large area, approximately 27% of the total skin area. The skin lesions were numerous and densely distributed, showing obvious unilateral distribution, which had a great impact on aesthetics and placed a heavy psychological burden on the patient. The authors hypothesized that the larger extent of involvement might be related to abnormal serum immunological markers. Whether this correlation exists still needs further study and discussion.
Laboratory examination of this case showed positive ANA and elevated IgM and negative anti-dsDNA antibody, anti-SM antibody, anti-SSA antibody, anti-SSB antibody, and anti-RNP antibody, and other immunoglobulins were normal. Yan et al described an LAM patient with positive ANA, ribonucleoprotein, and anti-SM antibodies.1 The pathology reported by some scholars suggested that LAM presented with perivascular lymphocyte infiltrate. The elevated IgM and numerous lymphocyte infiltrations in our case have never been reported before. Based on the absence of inflammatory erythema and blisters in the patient’s initial lesions, as well as the results of pathological biopsy and laboratory examination, we excluded other possible connective tissue diseases, inflammatory diseases, and immunodeficiency diseases, such as scleroderma, lupus erythematosus, blaschkitis and X-linked hyper IgM syndrome. Although an inflammatory stage has been suggested in a few reports, it might no longer remain by the time of clinical evaluation and biopsy. Thus, the inflammatory stage might be a common pathological manifestation of LAM, however, persistent inflammation may be atypical as shown in our case as well as elevated IgM.
It has been reported that oral methotrexate at a dose of 20 mg/week for 6 weeks10 and topical calcipotriol11 could improve the condition. Oral administration of potassium aminobenzoate12 could improve early skin lesions, emphasizing the importance of early clinical detection. When atrophic skin diseases are suspected, skin biopsy should be performed on both normal and diseased skin because atrophic skin diseases usually show very subtle features.13 The clinical course of LAM is stable, and there is generally no risk of progression. Patients can be followed up and tested clinically.
Conclusion
Although it is generally believed that LAM is a dermatosis without changes in the dermis, some reports do show alterations in the dermis. In this case, we found numerous lymphocyte infiltrates in the dermis, which shows the importance of the clinical pathology evolution. We suggest that the inflammatory stage might be common in LAM, while persistent inflammation and elevated IgM is atypical; however, whether there is a correlation between them or whether there is an impact on the development of LAM still needs further follow-up and discussion.
Consent Statements
Written informed consent was provided by the patient to have the case details and any accompanying images published. Institutional approval was not required for this case study.
Acknowledgments
We thank the patient for her permission to publish this information. This work was supported by the Zhejiang Natural Science Foundation of China (LBZ22H160001).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yan W, Wang S, Liu HJ, et al. Linear atrophoderma of Moulin: a disease related to immunity or a kind of connective tissue disease? Australas J Dermatol. 2017;58(3):e126–e8. doi:10.1111/ajd.12514
2. López N, Gallardo M, Mendiola M, Bosch R, Herrera E. Atrofodermia lineal de Moulin: presentación de un caso [A case of linear atrophoderma of Moulin]. Actas Dermosifiliogr. 2008;99(2):165–167. Lithuanian. doi:10.1016/S0001-7310(08)74649-0
3. Cecchi R, Bartoli L, Brunetti L, Pavesi M. Linear atrophoderma of Moulin localized to the neck. Dermatol Online J. 2008;14(6):12. doi:10.5070/D31W2688C0
4. Darung I, Rudra O, Samanta A, Agarwal M, Ghosh A. Linear atrophoderma of moulin over face: an exceedingly rare entity. Indian J Dermatol. 2017;62(2):214–215. doi:10.4103/ijd.IJD_469_16
5. Tukenmez Demirci G, Altunay IK, Mertoglu E, Kucukunal A, Sakız D. Linear atrophoderma of Moulin on the neck. J Dermatol Case Rep. 2011;5(3):47–49. doi:10.3315/jdcr.2011.1074
6. Marín-Hernández E, Suárez-Frías B, Siordia Reyes AG. Hyperpigmented lesions with acquired atrophy following Blaschko lines in a patient with diagnosed with localized scleroderma. Bol Med Hosp Infant Mex. 2021;78(6):621–630. doi:10.24875/BMHIM.20000350
7. Wang WM, Zeng YP. Linear atrophoderma of moulin. JAMA Dermatol. 2020;156(5):581. doi:10.1001/jamadermatol.2020.0320
8. Schepis C, Palazzo R, Lentini M. A teen-ager with linear atrophoderma of Moulin. Dermatol Online J. 2010;16(2):7. doi:10.5070/D386K1K785
9. Yamamoto N, Dejima A, Hasatani K. Linear morphea involving the underlying muscle. Clin Rheumatol. 2021;40(11):4767–4768. doi:10.1007/s10067-021-05789-2
10. Zaouak A, Ghorbel HH, Benmously-Mlika R, et al. A case of linear atrophoderma of Moulin successfully treated with methotrexate. Dermatol Ther. 2014;27(3):153–155. doi:10.1111/dth.12099
11. Wongkietkachorn K, Intarasupht J, Srisuttiyakorn C, Aunhachoke K, Nakakes A, Niumpradit N. Linear atrophoderma of moulin: a case report and review of the literature. Case Rep Dermatol. 2013;5(1):11–14. doi:10.1159/000346747
12. Artola Igarza JL, Sánchez Conejo-Mir J, Corbí Llopis MR, Linares Barrios M, Casals Andreu M, Navarrete Ortega M. Linear atrophoderma of Moulin: treatment with Potaba. Dermatology. 1996;193(4):345–347. doi:10.1159/000246288
13. Tan SK, Tay YK. Linear atrophoderma of Moulin. JAAD Case Rep. 2016;2(1):10–12. doi:10.1016/j.jdcr.2015.10.005
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.