Back to Journals » Journal of Blood Medicine » Volume 13
Association of ABO and Rhesus Blood Types with Transfusion-Transmitted Infections (TTIs) Among Apparently Healthy Blood Donors at Bahir Dar Blood Bank, Bahir Dar, North West, Ethiopia: A Retrospective Cross-Sectional Study
Authors Legese B , Shiferaw M, Tamir W, Eyayu T , Damtie S , Berhan A , Getie B , Abebaw A , Solomon Y
Received 19 May 2022
Accepted for publication 29 September 2022
Published 7 October 2022 Volume 2022:13 Pages 581—587
DOI https://doi.org/10.2147/JBM.S374851
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Biruk Legese,1 Mikru Shiferaw,2 Workineh Tamir,3 Tahir Eyayu,1 Shewaneh Damtie,1 Ayenew Berhan,1 Birhanu Getie,1 Aynework Abebaw,1 Yenealem Solomon1
1Department of Medical Laboratory Sciences, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 2Bahir Dar Blood Bank Service, Amhara Regional State Health Bureau, Bahir Dar, Ethiopia; 3Department of Medical Laboratory, College of Health Sciences, Injibara University, Injibara, Ethiopia
Correspondence: Biruk Legese, Email [email protected]
Background: Besides their clinical significance in blood transfusion medicine, ABO and Rh blood group antigens were found to be associated with many non-infectious and infectious diseases. This investigation aimed to assess the association of ABO and Rh blood group antigens with transfusion transmissible infections (TTIs).
Methods and Materials: A cross-sectional retrospective investigation was conducted on 27,027 blood donors at Bahir Dar blood bank, from March 24/2019 to October 21/2021. The blood sample was collected from each blood donor and tested for TTI markers (HBV, HCV, HIV, and syphilis), with ELISA, and ABO and Rh blood grouping was performed. Descriptive analysis was done for sociodemographic data, and a chi-square test was used to show the association between the ABO and Rh blood groups with TTI markers, and a P-value < 0.05 was considered statistically significant.
Results: From 27,027 study participants, 18,911 (70%) were males, with a mean age of 25.2 years, and 49.4% of the blood donors were students. The overall TTI prevalence was 5.43%, of which 2.8% was HBV, 1.5% was syphilis, 0.8% was HIV, and 0.3% was HCV. Blood group O (41.4%) was the most common blood group followed by, A (29.6%), B (23.6%), and AB (5.4%). Ninety-one point seven percent of the blood donors were Rh (D) positive. All TTI markers (HBV: p = 0.62, HIV: p = 0.77, HCV: p = 0.52, and syphilis: p = 0. 0.94) showed no significant association with ABO blood group. Rh blood type also showed no association with all TTI markers.
Conclusion: The prevalence of TTI markers was not significantly associated with ABO and Rh blood groups.
Keywords: ABO and Rh blood groups, blood donors, transfusion transmissible infections
Introduction
The surface of red blood cells (RBCs) contains different blood group antigens made up of polysaccharides and proteins. Along with their expression on red blood cells, ABO blood group antigens are also found on other cells and tissues like epithelium, sensory neurons, platelets, the vascular endothelium, breast ductal and lobular cells, and some malignant cells.1 Among the blood group antigens identified, ABO and Rhesus (Rh) are the most widely studied. Besides their clinical significance in the blood transfusion and compatibility, ABO and Rh blood group antigens were found to be associated with many non-infectious and infectious diseases.2,3 Several studies revealed these blood group antigens were associated with diabetes mellitus, hypertension, gastric cancer, duodenal ulcer, breast cancer, malaria, and helicobacter pylori infection.2,4,5 Some other studies also reported that ABO and Rh blood group antigens were associated with transfusion-transmitted infections (TTIs), which include Hepatitis B virus (HBV), human immunodeficiency virus (HIV), Hepatitis C virus (HCV), and syphilis.2,6,7
Nowadays, the prevalence of TTI is increasing, especially in the developing world. This high prevalence of TTI incurs increased morbidity, mortality, and compromises the quality of life of the world’s population. The acquisition of TTIs has become a vital obstacle, worthy of investigation, to maintain both the health and safety of human life.8
In Malawi, the prevalence of HBV, HCV, HIV, Syphilis was 3.6%, 1%, 1.9%, 2.6%, respectively, in 2015.9 A study conducted in Angola also reported even a higher TTI prevalence in which HBV (8.4%) infection covered a larger proportion, followed by syphilis (4.4%), HCV (3%) and HIV (2.1%).9,10 In Eritrea, the prevalence of HIV, HBV, HCV and Syphilis was 0.8%, 5%, 0.7% and 7.2%, respectively, and in Ethiopia, the overall prevalence of TTI was 6% (HBV = 3.9%, HCV = 0.6%, HIV = 0.5% and syphilis = 1.2%) in 2019.11,12
Considering this high prevalence, the World Health Organization (WHO) recommended that, the blood and blood products collected for transfusion should be screened for HIV, HBV, HCV, and syphilis as a minimum requirement.13 Additionally, strict pre-donation screening and deferral of blood donors with high-risk behaviors is required to ensure safe blood and blood product.
The route of transmission of TTIs is principally through blood and blood products, sharing of needles to inject drugs, needle stick injury, and sexual contact. After their entrance into the host different factors like immune status of the host, load of the infectious agent, and route of transmission contributed to the development of an active infection. In addition to these factors, several studies also disclosed that ABO and Rh blood group antigens were associated with the development of active infection.14,15 The probable pathogenesis for the link between blood group antigens and disease susceptibility is that many organisms may bind to polysaccharides on the cell surface, but soluble blood group antigens may block this binding. On the other hand, different ABO antigens can prevent the species carrying it from being threatened by a pathogen using a given carbohydrate as a receptor. On the other saying, the ABO polymorphism leads to a polymorphic production of anti-A and anti-B natural antibodies, which potentially protect individuals from several infectious agents expressing A and B antigens.16
Several studies were conducted to show the possible link between ABO and Rh blood groups with TTI. For instance, in a study conducted by Tyagi et al, blood group A negative was associated with an increased risk of contracting HIV and HBV infection, while blood group B negative with syphilis.15 Another study also found maximum TTI sero-reactivity among B blood group donors (2.21%) followed by blood group A donors (2.16%), O donors (1.57%), and AB donors (1.17%), but was not statistically significant.17 In a study conducted in Gabon, no significant association was obtained between the prevalence of HIV, HCV, and syphilis and the ABO and Rh blood groups. However, HBV sero-prevalence was twice as high among non-O blood group donors compared with blood group O donors.7 A systematic review and meta-analysis study by Jing et al, indicated that blood group B was associated with a lower risk of HBV infection.14
Despite the presence of several studies on this project, the findings were not consistent, and as to our understanding, there was no such study conducted in Ethiopia. The lack of such information has initiated us to conduct this investigation. The main objective of this study was to assess the association between transfusion-transmitted infections and the ABO and Rh blood groups. The information obtained will be used by the governmental agencies to set firm blood donor selection criteria, and blood banks to pay attention when they enrolled their blood donors.
Methods and Materials
A cross-sectional retrospective investigation was conducted on 27,027 blood donors at Bahir Dar blood bank from March 24/2019 to October 21/2021. Bahir Dar blood bank is located in the capital city of Amhara regional state Bahir Dar, Ethiopia. Bahir Dar is found in northwest Ethiopia 565 km away from Addis Ababa, the capital city of Ethiopia.
All blood donors, included in our analysis, were voluntary non-remunerated blood donors. Five milliliters of blood samples were collected from all blood donors, from which tests for TTI markers (HBV, HCV, HIV, and syphilis) and ABO and Rh blood grouping were performed. The serum sample from each blood donor was tested with an enzyme-linked immunosorbent assay (ELISA). HBV surface antigen (HBsAg) and anti HCV antibody (anti-HCV) were tested with third-generation ELISA (wantai, Beijing Wantai Biological Pharmacy, China), HIV 1 and 2 antibodies and antigens were tested with fourth-generation ELISA (Microlisa, J. Mitra and Co. Pvc. Ltd, India), and anti-Treponema pallidum antibodies were tested with DIALAB Syphilis IgG/IgM ELISA (Dia lab, Austria).
Forward and reverse ABO grouping was performed by slide method with commercially available antisera (anti-A and anti-B) (Mediclone, Mediclone Biotech, India) and by using 5% A and B cell suspension prepared at home, respectively. Rh typing was performed by test tube method with anti-D reagents, and Coombs test was performed to detect weak D antigen (Mediclone, Mediclone Biotech, India).
All donors’ data including relevant socio-demographic, TTI marker result, ABO and Rh blood type were registered on the computerized blood donor data management system. Ethical clearance was secured from research ethics committee of Injibara University College of Health Sciences with reference number HSc-350. The data were collected after getting a seal of approval from Bahir Dar blood bank. The data were checked for completeness, and transferred to SPSS version 23 for further analysis.
Descriptive analysis was done for sociodemographic data, and a chi-square test was used to show the correlation between the ABO and Rh blood groups with TTI markers, and a P-value <0.05 was considered statistically significant. Bonferroni post hoc test was performed to detect which cells from the contingency table were significantly different.
The data were collected after getting acquiescence from the blood bank, and we used only donor ABO and Rh blood group, age, sex, and occupation based on the code given at the blood bank. Other than these we did not use other voluntary blood donor data like name and phone number. All the data were secured, protected, and accessible only to the investigators.
Results
Of 27,027 study participants, 70% were males, and 58.5% were within 18–24 years age range (Table 1). The minimum and maximum ages were 18 and 67 years, with a mean age of 25.2 years, and 49.4% of the blood donors were students (Table 2). Blood group O (41.4%) was the most prevalent blood group followed by A (29.6%), B (23.6%), and AB (5.4%). Ninety-one point-seven percent of the blood donors were Rh (D) positive (Table 3). Of 27,027 blood donors, 1469 (5.4%) were positive at least for one of the TTI markers, from which HBV accounts 2.8% (767), syphilis 1.5% (402), HIV 0.8% (207) and HCV 0.3% (93) (Table 4).
 |
Table 1 Age and Sex Distribution of Study Participants |
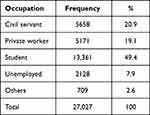 |
Table 2 Occupational Distribution of Study Participants |
 |
Table 3 ABO and Rh Blood Group Distribution of Study Participants |
 |
Table 4 Association of ABO and Rh Blood Group with TTI Markers |
Association of ABO and Rh Blood Group with TTI Markers
In this study, out of the 767 HBV positive cases, O (41.6%) was the most frequent blood group followed by A (29%), B (23%), and AB (6.4%). Among 207 HIV positive cases, blood group O (42.5%) blood donors were the most predominant succeeded by blood group A (27.5%), B (25.6%), and AB (4.4%). Of 93 HCV positive individuals, those with blood group O (46.2) were predominant followed by A (31.2%), B (17.2%), and AB (5.4%), and among 402 Syphilis reactive donors O (42.3%) blood group was predominant, followed by A (28.4), B (24.1%), AB (5.2%) blood group individuals. In HBV, syphilis, HIV, and HCV reactive case, 9.1%, 6.9%, 7.7%, and 11.8%, respectively, were Rh-negative (Table %).
Even though it was not statistically significant (X2 = 1.78, p = 0.62), this study revealed the highest prevalence of HBV case in blood group AB. Blood groups B and O were found to have equally higher prevalence of HIV (X2 = 1.12, p = 0.77). Relatively higher prevalence of HCV was seen in A and O blood groups (X2 = 2.24, p = 0.52), but B and O blood groups were considered as having equally higher prevalence of syphilis (X2 = 0.37, p = 0.94). Higher prevalence of HBV and HCV were seen among Rh-negative blood donors, while HIV and syphilis positivity rate was higher among Rh-positive blood group donors (Table 4).
Discussion
The relationship between ABO and Rh blood groups and numerous diseases has been investigated extensively by different scholars. The current study was conducted to show the association between TTIs (HBV, HCV, HIV, and syphilis) and ABO and Rh blood group antigens. On the current topic, several studies have been conducted, some of them reported a link between ABO and Rh blood types and TTIs,2,14 while others testified no significant association.17,18 In the current study the TTI prevalence was 5.4%, with HBV (2.8%) being the most prevalent, followed by Syphilis (1.5%), HIV (0.8%) and HCV (0.3%). Our finding was comparable with the output of studies conducted by Shiferaw et al,11 Biadgo et al19 and Arif et al6 but relatively lower than the prevalence reported by Peliganga et al10 and higher than that of Prakash et al17 and Hroob et al.8 The observed difference in the prevalence of TTI markers may be due to differences in lifestyle and economic status of the study participants.
In this study, even though it was not significant (p=0.62), the highest prevalence of HBV was found in blood group AB, whereas the lowest positivity rate was in blood groups A and B. Similarly, studies conducted by Prakash et al17 and Sreedhar Babu et al18 revealed no association between TTI markers and ABO blood groups. However, a study carried out by Liu et al2 revealed the presence of a significant association between ABO blood group and the risk of TTI, in which blood group O was associated with an increased HBV infection rate. In the current investigation, blood groups B and O were found to have the highest prevalence of HIV and syphilis, but the association was not statistically significant. This finding was in concordance with a study conducted by Ngassaki-Yoka et al,7 which detected no association between ABO blood group and TTIs. Even though it was not significant, a comparatively higher frequency of HCV positivity was seen among A and O blood group donors. This discrepancy might be caused by characteristics of the study participants and the differences in blood type frequency distribution in different ethnic groups.2
This study also testified that Rh (D) type was not associated with all TTI markers’ positivity rate. In line with our finding, investigations done by Bharadva et al20 and Sreedhar Babu et al18 found no association, but the existence of a significant association was reported by Liu et al,2 in which Rh-D-positive participants were at higher risk of HBV infection.
Conclusion and Recommendation
The main aim of this research work was to show the prevalence of TTI (HBV, HCV, HIV, and syphilis) and its association with ABO and Rh blood groups. According to our findings, the prevalence of TTI was not significantly associated with ABO and Rh blood group phenotypes.
Data Sharing Statement
All relevant data are included in this document.
Ethical Considerations
Ethical clearance was obtained from research ethics committee of Injibara University College of Health Sciences with reference number HSc-350. A permission letter was obtained from Bahir Dar blood bank. Since it was a retrospective analysis, written informed consent was not obtained from each study participant. To safeguard confidentiality, all blood donor data were collected after removing all personal identifiers by the blood bank data manager.
Consent for Publication
Consent for publication of this work was found from Bahir Dar blood bank.
Acknowledgment
Authors’ deepest gratitude goes to Bahir Dar blood bank staff for their cooperation during the data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors have declared that no competing interests exist.
References
1. Gylmiyarova FN, Ryskina E, Kolotyeva N, Kuzmicheva V, Gusyakova O. ABO blood group antigens as a model of studying protein-protein interactions. In: Blood Groups. IntechOpen; 2018.
2. Liu J, Zhang S, Liu M, Wang Q, Shen H, Zhang Y. Distribution of ABO/Rh blood groups and their association with hepatitis B virus infection in 3.8 million Chinese adults: a population‐based cross‐sectional study. J Viral Hepat. 2018;25(4):401–411. doi:10.1111/jvh.12829
3. Legese B, Abebe M, Fasil A. Association of ABO and Rh blood group phenotypes with type 2 diabetes mellitus at Felege Hiwot comprehensive Referral Hospital Bahir Dar, Northwest Ethiopia. Int J Chron Dis. 2020;2020. doi:10.1155/2020/2535843
4. Anstee DJ. The relationship between blood groups and disease. Blood. 2010;115(23):4635–4643.
5. Meo S, Rouq F, Suraya F, Zaidi S. Association of ABO and Rh blood groups with type 2 diabetes mellitus. Eur Rev Med Pharmacol Sci. 2016;20(2):237–242.
6. Arif SH, Saeed N, Alam K. Association of ABO and Rh blood group with transfusion transmitted infections (TTI) among blood donors in north India. J Blood Disord Transfus. 2019;10(4):271–275.
7. Ngassaki-Yoka C-D, Ndong JMN, Bisseye C. ABO, rhesus blood groups and transfusion-transmitted infections among blood donors in Gabon. Sud J Med Sci. 2018;13(1):12–21. doi:10.18502/sjms.v13i1.1685
8. Hroob AMA, Saghir SA, Almaiman AA, et al. Prevalence and association of transfusion transmitted infections with ABO and Rh blood groups among blood donors at the national blood bank, Amman, Jordan. Medicina. 2020;56(12):701. doi:10.3390/medicina56120701
9. M’baya B. Seroprevalence and trends in transfusion transmissible infections among voluntary non-remunerated blood donors at the Malawi Blood Transfusion Service – a time trend study. Malawi Med J. 2019;31(2):118–125. doi:10.4314/mmj.v31i2.3
10. Peliganga LB, Mello VM, de Sousa PSF, et al. Transfusion transmissible infections in blood donors in the Province of Bié, Angola, during a 15-year follow-up, imply the need for pathogen reduction technologies. Pathogens. 2021;10(12):1633. doi:10.3390/pathogens10121633
11. Shiferaw E, Tadilo W, Melkie I, Shiferaw M, Chemin I. Sero-prevalence and trends of transfusion-transmissible infections among blood donors at Bahir Dar district blood bank, northwest Ethiopia: a four year retrospective study. PLoS One. 2019;14(4):e0214755. doi:10.1371/journal.pone.0214755
12. Keleta YT, Achila OO, Haile AW, et al. Seroprevalence of transfusion transmitted infections among blood donors in Gash Barka Zonal Blood Transfusion Center, Barentu, Eritrea, 2014 through 2017. BMC Hematol. 2019;19(1):1–9. doi:10.1186/s12878-019-0136-5
13. World Health Organization. Blood safety and availability; 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability.
14. Jing W, Zhao S, Liu J, Liu M. ABO blood groups and hepatitis B virus infection: a systematic review and meta-analysis. BMJ Open. 2020;10(1):e034114. doi:10.1136/bmjopen-2019-034114
15. Tyagi S, Tyagi A. Possible correlation of transfusion transmitted diseases with Rh type and ABO blood group system. J Clin Diagn Res. 2013;7(9):1930. doi:10.7860/JCDR/2013/6002.3360
16. Abegaz SB, Erg n S. Human ABO blood groups and their associations with different diseases. Biomed Res Int. 2021;2021:1–9. doi:10.1155/2021/6629060
17. Prakash S, Sahoo D, Mishra D, et al. Association of transfusion transmitted infections with ABO and Rh D blood group system in healthy blood donors: a retrospective analysis. IJCMPH. 2020;7:4444–4448.
18. Kondareddy S, Madithadu A. Association of ABO and Rh blood groups to HBV, HCV infections among blood donors in a blood bank of tertiary care teaching hospital in Southern India: a retrospective study. IJRMS. 2015;3(7):1672–1676.
19. Biadgo B, Shiferaw E, Woldu B, Alene KA, Melku M, Blackard J. Transfusion-transmissible viral infections among blood donors at the North Gondar district blood bank, northwest Ethiopia: a three year retrospective study. PLoS One. 2017;12(7):e0180416. doi:10.1371/journal.pone.0180416
20. Bharadva S, Vachhani J, Dholakiya S. ABO and Rh association to transfusion transmitted infections among healthy blood donors in Jamnagar, Gujarat, India. J Res Med Dent Sci. 2016;4(1):58–62. doi:10.5455/jrmds.20164113
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
