Back to Journals » Open Access Journal of Sports Medicine » Volume 8
Association between sensory function and hop performance and self-reported outcomes in patients with anterior cruciate ligament injury
Authors Cronström A , Roos EM , Ageberg E
Received 18 August 2016
Accepted for publication 29 November 2016
Published 19 January 2017 Volume 2017:8 Pages 1—8
DOI https://doi.org/10.2147/OAJSM.S120058
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Andreas Imhoff

Anna Cronström,1 Ewa M Roos,2 Eva Ageberg1
1Department of Health Sciences, Lund University, Lund, Sweden; 2Research Unit for Musculoskeletal Function and Physiotherapy, Department of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense, Denmark
Background: In patients with anterior cruciate ligament (ACL) deficiency (ACLD) or reconstruction (ACLR), sensory deficits are commonly assessed as knee kinesthesia using time-consuming laboratory equipment. Portable equipment such as that used for evaluation of vibration sense would be preferable. In contrast to kinesthesia, vibration sense is not well studied in these patients.
Objectives: 1) To study the association between kinesthesia and vibration sense to investigate if one sensory measurement can replace the other; and 2) to determine the clinical relevance by investigating associations between the sensory measurements and functional performance and patient-reported outcomes in patients with ACLD or ACLR.
Methods: Twenty patients with ACLD and 33 patients with ACLR were assessed with knee kinesthesia, vibration sense, the one-leg hop test for distance, as well as the Knee injury and Osteoarthritis Outcome Score (KOOS) and the Tegner Activity Scale.
Results: There were no significant correlations between kinesthesia and vibration sense (r= –0.267, p>0.269) or between the sensory measures and hop performance (r= –0.351, p>0.199). In patients with ACLD, worse knee kinesthesia was associated with worse scores on KOOS subscales pain (r= –0.464, p=0.046) and activities of daily living (r= –0.491, p=0.033), and worse vibration sense was associated with worse scores on KOOS subscale quality of life (r= –0.469, p=0.037) and worse knee confidence (item Q3 from subscale quality of life) (rs=0.436, p=0.054). In patients with ACLR, worse vibration sense was associated with worse scores on KOOS subscales pain (r= –0.402, p=0.020) and activities of daily living (r= –0.385, p=0.027).
Conclusion: Kinesthesia and vibration sense cannot be used interchangeably as measures of sensory function in patients with ACLD or ACLR. Both sensory measurements were weakly related to hop performance. Adequate sensory function appears to have importance for perceived function in patients with ACLD or ACLR and may therefore be a factor that needs to be addressed in rehabilitation programs for these patients.
Keywords: knee injury, proprioception, sensory function, functional performance, patient reported outcomes
Background
Proprioception sense is often impaired in patients with anterior cruciate ligament (ACL) deficiency (ACLD) or reconstruction (ACLR).1 Proprioceptive deficits are commonly assessed by joint position sense (JPS) or the ability to detect movement at the knee (kinesthesia).2,3 Both kinesthesia and JPS are measured with laboratory equipment, limiting the possibility of using the tools at various sites. A clinically feasible alternative to this laboratory equipment could facilitate and enhance the assessment of sensory function in clinical settings.
Proprioceptive impairment is suggested to be due to loss of the mechanoreceptors situated in the ACL that are responsible for proprioceptive information to the central nervous system. Afferent signals from these receptors are also proposed to play an important role in muscle stiffness control, thereby contributing to dynamic joint stability.4 This is reflected by an observed association between proprioceptive deficiency and perceived instability of the knee (give-way episodes),5 poorer hop performance,6 and poorer balance7 in patients with ACLD. The clinical relevance of proprioceptive acuity in patients with ACLR is, however, not well established. Previous research suggests a correlation between worse proprioception and lower activity level in patients with ACLR,8 no relation between proprioception and balance,9 and contradictive evidence for the association between proprioception and quadriceps function.10,11
Recently, there has been an increased interest in vibration sense as a measure of sensory function in patients with knee injury at high risk of osteoarthritis (OA).12–14 Deficiencies in both proprioception sense15,16 and vibration sense in the affected and adjacent joints were observed in patients with knee OA.12 Moreover, an association was found between poorer vibration sense at the knee and worse performance of the number of knee bendings in 30 seconds in middle-aged patients with meniscectomy17 and between both poorer vibration sense and worse kinesthesia, as well as worse movement quality of the knee during stair descending and drop jump in patients with ACLD or ACLR.14 In these studies, vibration sense was measured by the vibration perception threshold (VPT) with a portable instrument.12,18,19
Vibration sense has previously been suggested to be a component of proprioception,20 and so a covariance between these sensory measures may exist. Tactile sense, like vibration sense, arises from receptors partly shared with those responsible for proprioception, such as the Pancinian corpuscles, and uses the same pathways to the brainstem.21 Because vibration sense is measured with portable equipment is quite easy to use and is a less time-consuming assessment than kinesthesia, it would be a more suitable instrument for assessing sensory function in large-scale studies and in the clinical setting. There are numerous studies on kinesthesia in subjects with ACLD or ACLR,22 but vibration sense is poorly studied in these patients.13,14
The aim of this study was to assess the association between kinesthesia and vibration sense in subjects with ACLD or ACLR, respectively. A sufficiently high correlation between these measurements would suggest that one measurement could replace the other. To determine the clinical relevance, the association between sensory function and functional performance and patient-reported outcomes were assessed. We hypothesized that worse sensory function would be moderately associated with worse hop performance and worse self-reported outcomes in both patients with ACLD and in those with ACLR.
Methods
Subjects
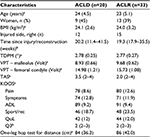
As a sample of convenience, 33 patients with ACLR (mean age 24 years, range 18–35 years, women n=13) and 20 patients with ACLD treated without reconstruction (mean age 23 years, range 18–35 years, women n=9) were included (Table 1). Inclusion criteria were the following: arthroscopically or MRI-verified complete ACL injury, with or without ACL reconstruction, currently being treated with rehabilitation, and self-reported functional limitations (determined as at least moderate knee-related problems in at least two of four questions [SP3 (jumping), SP4 (twisting/pivoting), Q3 (knee confidence), Q4 (difficulty with knee in general)] from the knee injury and osteoarthritis outcome score (KOOS) subscales sport and recreation function and quality of life [QOL]).23 Patients who used crutches and those with other injuries affecting lower extremity function were excluded. The patients were recruited at physical therapy clinics where they all took part in neuromuscular training. Thirty-nine of the 53 patients were included in previous reports.13,24 The study was approved by the Research Ethics committee of Lund University (LU 107/2007), and all subjects gave their written informed consent.
Assessment
All participants were assessed with both measures of sensory function and the KOOS and the Tegner activity scale (TAS). Thirty-nine of the patients24 also performed the one-leg hop test (OLH) for distance for assessment of functional performance. Measurements from the injured leg were used. (The images provided illustrate the methods used. The persons in the pictures were not included in the data collection, but they gave their written consent to publish the images).
Knee kinesthesia
Kinesthesia was measured by the threshold to detection of passive motion (TDPM) on a specially designed platform as described previously3 (Figure 1). The platform is mounted inside a steel frame and has an electric motor with a wire mounted at one end. The subject lay on the platform in a lateral position with the lower leg in a plastic splint. The splint is attached to a sled and connected to the wire, which can make the splint move the knee in either flexion or extension. The analog scale at the end of the platform registers movements in increments of 0.25 degrees. The subjects were told to close their eyes and indicate by raising their hand when any movement in the knee was felt. TDPM was measured toward extension (TE) and toward flexion (TF) from a 20-degree starting position, (TE20 and TF20, respectively). The median value of three consecutive measurements of TE20 and TF20, respectively, was determined. An index value created from the sum of TE20 and TF20 was used for statistical analysis. A higher value indicates worse kinesthetic acuity. Moderate reliability (intraclass correlation coefficient [ICC] =0.63–0.70) has previously been reported for this device.3
  | Figure 1 Kinesthesia testing device. |
VPT
VPT was measured with a biothesiometer (Bio-Medical Instrument, Newbury, OH, USA)25,26 according to the manufacturers manual, and based on the protocol of our previous study27 (Figure 2). The application button on the biothesiometer was held in such way that the weight of the machine provided the application button with a standard pressure. The vibrator was held to the subject’s most prominent point of the medial malleolus and the medial femoral condyle. The subjects were in a supine position with closed eyes and were told to indicate by raising their hand when any sensation of vibration was felt. The amplitude was increased in increments of 1 volt per second and the measure (Volt) when the subject first felt any sensation of vibration was noted as the VPT. The mean of two subsequent measurements was calculated as described.27 A higher value indicates worse vibration sense. High reliability (ICC =0.96–0.99) for the biothesiometer has been reported.12
  | Figure 2 Vibration sense assessed with the biothesiometer. |
OLH test for distance
The subjects performed an OLH test for distance with the arms free as described previously.28 All subjects wore shoes and had one try of the test prior to the actual assessment. The subjects stood on one leg with the arms freely hanging and were then asked to jump as far as possible, landing on the same foot and remaining in the landing position for 2–3 seconds. The distance from the toe in the take-off position to the heel in the landing position was measured in centimeters. If the subject improved more than 10 cm between the second and third hop, additional hops were performed until an increase of less than 10 cm was measured. The mean value of three consecutive measures was then calculated and used for statistical analysis. A longer distance indicates better performance. High reliability (ICC =0.95) has been reported for the OLH test for distance in subjects with an ACL deficient knee.29
Patient-reported questionnaires
Two different patient-reported questionnaires were used. The KOOS was used to assess patients’ perceived knee symptoms and related problems. The KOOS is a patient-reported questionnaire consisting of five subscales: pain, other symptoms, function in daily living (ADL), function in sport and recreation, and knee-related QOL. The questionnaire includes 42 questions, with each question is scored from 0 to 4. The score from each subscale is normalized, with 0 indicating extreme problems and 100 indicating no problems.23 The five subscales were used in the analysis on the relation between sensory function and patient-reported function. In addition, the single item Q3 from the subscale QoL (“How much are you troubled with lack of confidence in your knee?”) was used to specifically assess the association between perceived knee confidence and sensory function. The KOOS has high reliability (ICC =0.84–0.89) and has been validated for the ACL population.30
The TAS was used to measure the patients’ activity level. The TAS is an ordinal scale from 0 to 10, where 0 indicates sick leave or disability pension because of knee problems and 10 indicates participation in competitive sports such as soccer on an elite level.31
Statistics
Data were checked for normality by visual observation of histogram and the Kolmogorov–Smirnov Test. All data met the assumptions of normality. Pearson’s correlation coefficient (r) was calculated for all correlations, except for the TAS and Q3 where the Spearman’s rank correlation coefficient (rs) was used. We used a correlation coefficient of 0.75 or above to suggest that a vibration sense measure could replace the assessment of knee kinesthesia. Pearson’s correlation coefficient and the independent t-test were used as appropriate to evaluate any possible associations between demographics and sensory function. p-values less than or equal to 0.05 were considered statistically significant.
Results
Demographic data for patients with ACLD and ACLR are reported in Table 1. There were no associations between gender, time since injury, or time since reconstruction and kinesthesia or vibration sense (p≥0.138).
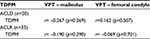
The correlation coefficients between kinesthesia and vibration sense were lower than r=0.267 (p>0.269) for both ACLR and ACLD (Table 2).
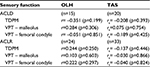
The correlation coefficients between TDPM and the OLH test were r≤–0.351 (p>0.199) and r≤0.284 (p>0.297) between VPT and the OLH test (Table 3).
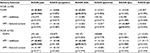
In patients with ACLD, worse TDPM was associated with worse scores on the KOOS subscales pain (r= –0.464, p=0.046) and ADL (r= –0.491, p=0.33). Also, worse VPT at the femoral condyle was associated with worse score on the KOOS subscale QoL (r= –0.469, p=0.037) and worse score on item Q3 (rs=0.436, p=0.054). In patients with ACLR, worse VPT at the malleolus was associated with worse scores on the KOOS subscales pain (r= –0.402, p=0.020) and ADL (r= –0.385, p=0.027). No significant associations were found between sensory function and the other KOOS subscales or the TAS in the two patient groups (Tables 3 and 4).
Discussion
The lack of correlation between TDPM and VPT indicate that these measures assess different aspects of sensory function in subjects with ACLD or ACLR and can, therefore, not be used interchangeably. We found no association between the sensory measures and the OLH, suggesting that kinesthesia and vibration sense may be of little importance for hop performance in these individuals. Worse TDPM and VPT were, however, associated with worse scores on several KOOS subscales in both ACLD and ACLR patients, suggesting both sensory measures to be of relevance for patients’ perceived function.
Association between kinesthesia and vibration sense
One possible reason for the lack of association between TDPM and VPT in the current study may be that vibration sense and proprioception originate from different receptors. Peripheral receptors in joints, muscles, and ligaments (like Golgi organ, free nerve endings, as well as Pacinian corpuscles and Ruffini endings) provide the cerebral cortex with proprioceptive information via the dorsolateral pathway.4 Information regarding sense of vibration rise from four different receptors – Pacinian corpuscles, Meissner’s corpuscles, Merkel’s disks, and Ruffini endings – situated in the deeper layer of the skin, between the muscles, and in the periosteum. Although proprioception sense and vibration sense utilize the same pathways in the dorsal column, they arise from different receptors situated in different areas around the knee joints.21 The results of the present study indicate that TDPM and VPT measure different aspects of sensory function and that they cannot be used interchangeably in patients with ACLD or ACLR.
Our results are in line with the results of studies done in people with ankle sprain and in healthy adults,32–34 reporting low correlations between different measures of proprioception, ie, JPS, kinesthesia, and velocity discrimination. The results from these studies,32–34 and from the present study, highlight the difficulty in using a single outcome for assessing sensory deficiency. Further investigations may reveal whether an association between TDPM and VPT exists in other populations with more severe disease, such as patients with established OA, where both vibratory and proprioceptive deficiencies are known to be present.12,15,16
Association between sensory measures and functional performance
Sensory function was reported to be associated with the execution of functional performance tasks in patients with ACLD or OA.6,7,14,18 For example, in one study, an association between worse kinesthesia and poorer balance was found in women with ACLD,7 while in another study, it was reported that patients with ACLD or ACLR performed functional tasks such as drop jump and stair descending with worse knee movement quality if they had worse VPT or TDPM.14 In the current study, we found low correlations between sensory function and the OLH test (r≤0.35, p>0.2). The result for kinesthesia is in line with results from a recent review where, in general, low-to-moderate correlations between proprioception and hop tests (r= –0.11 to 0.56) were reported.22 In line with this, our results indicate that VPT also seems to be of little importance for the execution of the OLH in these patients. Taken together, the findings from previous studies and the present study suggest that sensory function is not a major contributor for hop performance in young adults with ACLD or ACLR.
Association between the sensory measures and patient-reported outcomes
In the current study, worse sensory function was moderately associated with worse scores on the KOOS subscales pain, ADL, and QoL in patients with ACLD (r= ≥0.464), and with worse Pain and ADL scores in those with ACLR (r= ≥0.385). Our results are inconsistent with findings reported in a previous review where at most, low correlations were observed between proprioception (measured by TDPM or active knee rotation movements) and patient-reported outcomes assessed using scales such as the Cincinatti knee scale, international knee documentation committee, and/or KOOS in patients with ACLD or ACLR.22 In the study where the KOOS was used, no or low correlations were noted between TDPM and the KOOS subscales.35 The patients in that study were assessed on average 2 years after ACLR,35 while the patients in our study were assessed less than 6 months after ACLD/ACLR while they still had rehabilitation treatment. The patients in the study by Risberg et al35 also reported better KOOS scores than the patients in the current study, and with several KOOS subscale scores being close to that of a noninjured population. This could imply that sensory function is one aspect that needs to be addressed in rehabilitation treatment, while sensory function may be of less importance the longer the time has passed since injury/surgery and rehabilitation. Further studies are needed to confirm this assumption.
In line with several other studies,22 we found no relation between proprioception and the TAS in patients with ACLD. Our findings indicate that this applies also to patients with ACLR. In another study, worse proprioception, assessed by an active knee rotation movement, was associated with lower activity assessed with the Sport Activity Rating Scale in patients with ACLR.8 The activity rating scale measures the frequency of participation in knee-demanding activities, while the TAS measures the level of activity. Thus, different aspects of activity (frequency vs level) are likely captured in these two questionnaires, which may be one reason for the difference in the result between the study by Muaidi et al8 and previous studies, including ours. Another explanation may be the differences in proprioceptive measurements, ie, knee flexion–extension in our study and in previous studies22 versus knee rotation.8
We observed some differences in the associations between sensory function and KOOS in the patients with ACLD and ACLR. Worse TDPM and worse VPT at the femoral condyle were associated with worse KOOS subscales in patients with ACLD, whereas worse VPT at the malleolus was associated with worse KOOS subscales in those with ACLR. In a recent meta-analysis, it was reported that patients with ACLD have worse proprioception than those with ACLR.1 Possible reasons for the differences between ACLR and ACLD in the contribution of the sensory measures for perceived function remain unknown as neither the present study nor previous studies1 have included patients that were randomized to surgical or nonsurgical treatment. However, one can speculate whether treatment with or without reconstructive surgery may lead to different compensatory strategies in the sensorimotor system. Further studies are needed to investigate this. Our results suggest that both vibratory and proprioceptive acuity is important for perceived function, such as pain and quality of life, in patients with ACL injury, implying that sensory function needs to be addressed in rehabilitation training.
Limitations
Some limitations of this study should be recognized. This study had a cross-sectional design and we are, therefore, unable to draw any conclusions regarding causal relationships. Furthermore, because this was an exploratory study, we did not correct for multiple comparisons. Therefore, further studies are needed to confirm our results.
Conclusion
The lack of correlation between kinesthesia and vibration sense in patients with ACLD or ACLR indicate that these measurements assess different aspects of sensory function, and that they can, therefore, not be used interchangeably. Both kinesthesia and vibration sense appear to be of importance for perceived function, but seem to only be weakly associated with hop performance and activity level in patients with ACL injury.
Author contributions
AC contributed to the design of the study, was responsible for analysis and interpretation of data, and was in charge of drafting and writing the manuscript. ER contributed to the conception and design of the study, contributed to interpretation of data and critically revised this paper. EA contributed to the conception and design of the study, was responsible for acquisition of data, contributed in analysis and interpretation of data, contributed in drafting and writing the manuscript, and provided feedback on drafts of this paper. All authors read and approved the final manuscript and agreed to be accountable for all aspects of the work.
Acknowledgment
Grant supporters: The Swedish Research Council (2009-1447), the Crafoord Foundation, Skåne Regional Council, the Swedish Rheumatism Association, and the Faculty of Medicine, Lund University.
Disclosure
The authors report no conflicts of interest in this work.
References
Relph N, Herrington L, Tyson S. The effects of ACL injury on knee proprioception: a meta-analysis. Physiotherapy. 2014;100(3):187–195. | ||
Fridén T, Roberts D, Ageberg E, Walden M, Zätterström R. Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther. 2001;31(10):567–576. | ||
Ageberg E, Flenhagen J, Ljung J. Test-retest reliability of knee kinesthesia in healthy adults. BMC Musculoskelet Disord. 2007;8:57. | ||
Riemann BL, Lephart SM. The sensorimotor system, part II: the role of proprioception in motor control and functional joint stability. J Athl Train. 2002;37(1):80–84. | ||
Roberts D, Fridén T, Zätterström R, Lindstrand A, Moritz U. Proprioception in people with anterior cruciate ligament-deficient knees: comparison of symptomatic and asymptomatic patients. J Orthop Sports Phys Ther. 1999;29(10):587–594. | ||
Roberts D, Ageberg E, Andersson G, Fridén T. Clinical measurements of proprioception, muscle strength and laxity in relation to function in the ACL-injured knee. Knee Surg Sports Traumatol Arthrosc. 2007;15(1):9–16. | ||
Ageberg E, Roberts D, Holmstrom E, Fridén T. Balance in single-limb stance in patients with anterior cruciate ligament injury: relation to knee laxity, proprioception, muscle strength, and subjective function. Am J Sports Med. 2005;33(10):1527–1535. | ||
Muaidi QI, Nicholson LL, Refshauge KM, Adams RD, Roe JP. Effect of anterior cruciate ligament injury and reconstruction on proprioceptive acuity of knee rotation in the transverse plane. Am J Sports Med. 2009;37(8):1618–1626. | ||
Birmingham TB, Kramer JF, Kirkley A, Inglis JT, Spaulding SJ, Vandervoort AA. Knee bracing after ACL reconstruction: effects on postural control and proprioception. Med Sci Sports Exerc. 2001;33(8):1253–1258. | ||
Zhou MW, Gu L, Chen YP, et al. Factors affecting proprioceptive recovery after anterior cruciate ligament reconstruction. Chin Med J. 2008;121(22):2224–2228. | ||
Co FH, Skinner HB, Cannon WD. Effect of reconstruction of the anterior cruciate ligament on proprioception of the knee and the heel strike transient. J Orthop Res. 1993;11(5):696–704. | ||
Shakoor N, Agrawal A, Block JA. Reduced lower extremity vibratory perception in osteoarthritis of the knee. Arthritis Rheum. 2008;59(1):117–121. | ||
Thorlund JB, Shakoor N, Ageberg E, Sandal LF, Block JA, Roos EM. Vibratory perception threshold in young and middle-aged patients at high risk of knee osteoarthritis compared to controls. Arthritis Care Res (Hoboken). 2012;64(1):144–148. | ||
Cronström A, Ageberg E. Association between sensory function and medio-lateral knee position during functional tasks in patients with anterior cruciate ligament injury. BMC Musculoskelet Disord. 2014;15(1):430. | ||
Hewitt BA, Refshauge KM, Kilbreath SL. Kinesthesia at the knee: the effect of osteoarthritis and bandage application. Arthritis Rheum. 2002;47(5):479–483. | ||
Hassan BS, Mockett S, Doherty M. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis. 2001;60(6):612–618. | ||
Sandal LF. Reliability and construct validity of vibratory perception threshold testing [Master thesis]. Copenhagen, Denmark: University of southern Denmark; 2011. | ||
Shakoor N, Lee KJ, Fogg LF, et al. The relationship of vibratory perception to dynamic joint loading, radiographic severity, and pain in knee osteoarthritis. Arthritis Rheum. 2012;64(1):181–186. | ||
Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61(7):617–622. | ||
Noback C, Strominger N, Demarest R, Ruggiero D. The human nervous system: structure and function. 6th ed. Totowa, NJ: Human Press; 2005. | ||
Gilman S. Joint position sense and vibration sense: anatomical organisation and assessment. J Neurol Neurosurg Psychiatry. 2002;73(5):473–477. | ||
Gokeler A, Benjaminse A, Hewett TE, et al. Proprioceptive deficits after ACL injury: are they clinically relevant? Br J Sports Med. 2012;46(3):180–192. | ||
Roos EM, Roos HP, Ekdahl C, Lohmander LS. Knee injury and Osteoarthritis Outcome Score (KOOS) – validation of a Swedish version. Scand J Med Sci Sports. 1998;8(6):439–448. | ||
Ageberg E, Björkman A, Rosen B, Roos EM. Principles of brain plasticity in improving sensorimotor function of the knee and leg in patients with anterior cruciate ligament injury: a double-blind randomized exploratory trial. BMC Musculoskelet Disord. 2012;13(1):68. | ||
Shakoor N, Lee KJ, Fogg LF, Block JA. Generalized vibratory deficits in osteoarthritis of the hip. Arthritis Rheum. 2008;59(9):1237–1240. | ||
Frenette B, Mergler D, Ferraris J. Measurement precision of a portable instrument to assess vibrotactile perception threshold. Eur J Appl Physiol Occup Physiol. 1990;61(5–6):386–391. | ||
Ageberg E, Björkman A, Rosen B, Lundborg G, Roos EM. Principles of brain plasticity in improving sensorimotor function of the knee and leg in healthy subjects: a double-blind randomized exploratory trial. BMC Musculoskelet Disord. 2009;10:99. | ||
Ageberg E, Thomee R, Neeter C, Silbernagel KG, Roos EM. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum. 2008;59(12):1773–1779. | ||
Gustavsson A, Neeter C, Thomee P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):778–788. | ||
Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM. Knee injury and osteoarthritis outcome score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage. 2016;24(8):1317–1329. | ||
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. | ||
Westlake KP, Wu Y, Culham EG. Velocity discrimination: reliability and construct validity in older adults. Hum Mov Sci. 2007;26(3):443–456. | ||
Grob KR, Kuster MS, Higgins SA, Lloyd DG, Yata H. Lack of correlation between different measurements of proprioception in the knee. J Bone Joint Surg Br. 2002;84(4):614–618. | ||
de Jong A, Kilbreath SL, Refshauge KM, Adams R. Performance in different proprioceptive tests does not correlate in ankles with recurrent sprain. Arch Phys Med Rehabil. 2005;86(11):2101–2105. | ||
Risberg MA, Beynnon BD, Peura GD, Uh BS. Proprioception after anterior cruciate ligament reconstruction with and without bracing. Knee Surgery Sports Traumatol Arthrosc. 1999;7(5):303–309. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.