Back to Journals » Vascular Health and Risk Management » Volume 12
Association between perceived lifetime risk of cardiovascular disease and calculated risk in a male population in Brazil
Authors Maciel de Lima Junior M , Rocha da Silva G, Salazar Jansem Filho S, Granja F
Received 5 March 2016
Accepted for publication 13 April 2016
Published 22 June 2016 Volume 2016:12 Pages 279—286
DOI https://doi.org/10.2147/VHRM.S107874
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
Mário Maciel de Lima Jr,1,2 Glaciane Rocha da Silva,3 Sebastião Salazar Jensem Filho,2 Fabiana Granja3
1Department of Urology, Coronel Mota Hospital, Roraima, 2Cathedral College, 3Biodiversity Research Center, Federal University of Roraima (CBio/UFRR), Roraima, Brazil
Aim: Cardiovascular disease is the major cause of morbidity and mortality across the world. Despite health campaigns to improve awareness of cardiovascular risk factors, there has been little improvement in cardiovascular mortality. In this study, we sought to examine the association between cardiovascular risk factors and people’s perception on cardiovascular risk.
Methods: This was an epidemiological, cross-sectional, descriptive, prospective study of Masonic men aged >40 years in Boa Vista, Brazil. Participants completed a health survey, which included three questions about perception of their stress level, overall health status, and risk of a heart attack. In addition, demographic and biological data were collected.
Results: A total of 101 Masonic men took part in the study; their mean age (± standard deviation) was 55.35±9.17 years and mean body mass index was 28.77±4.51 kg/m2. Answers to the lifestyle questionnaire suggested an overall healthy lifestyle, including good diet and moderate exercise, although despite this ~80% were classified as overweight or obese. The majority of participants felt that they had a low stress level (66.3%), good overall general health (63.4%), and were at low risk of having a heart attack (71.3%). Masons who were overweight were significantly more likely to perceive themselves to be at risk of a heart attack (P=0.025).
Conclusion: Despite over half of participants having a moderate to high risk of cardiovascular disease according to traditional risk factors, less than a third perceived themselves to be at high risk. Public health campaigns need to better communicate the significance of traditional cardiovascular risk in order to improve awareness of risk among the general population.
Keywords: cardiovascular disease, cardiovascular risk factors, overweight, stress level
Introduction
Cardiovascular disease (CVD) is the primary cause of morbidity and mortality across the Western world.1 Although our ability to diagnose and treat CVD has significantly improved over recent decades, this has not translated to improvements in cardiovascular mortality. CVD therefore remains a major and growing concern.1 Strategies to further reduce both the development of and related morbidity and mortality are urgently required.
One of the major advances in the efforts to reduce cardiovascular mortality has been the development of risk calculators, such as the Framingham risk score.2 The Framingham risk calculator takes into account known risk factors for CVD such as age, sex, history of smoking and diabetes, blood pressure, and cholesterol levels to calculate the 10-year risk probability of developing CVD for a given patient.3,4 Given that a number of these factors, such as smoking and high cholesterol, are modifiable, these have become the target of health campaigns to lower the prevalence of CVD. However, despite governments putting huge resources into such campaigns, the benefit has not been realized, and CVD remains a growing concern across the globe.5 Of note, a recent report by the World Health Organization suggested that much of the growth in CVD mortality is driven by lower and middle-income countries, where prevalence is growing rapidly, while in higher income countries, there is the suggestion that campaigns may be beginning to have some impact.1
One of the drawbacks of the Framingham risk calculator is that it is only able to project 10-year (ie, short term) risk, and as such a large number in the population, for example, those aged younger than 50 years, will be classified as low risk, despite potentially having multiple risk factors for high lifetime risk of CVD. Identifying risk as early as possible in an individual’s life course may be key to ensuring maximum time to modify high-risk behaviors and therefore maximum probability of reducing risk and preventing the onset of CVD. More recently, therefore, efforts have focused on developing better long-term risk tools to accurately define a person’s lifetime risk of developing CVD.6–8 A recent study by Petr et al9 examined the relationship between calculated lifetime risk and an individual’s perception of their own lifetime risk. They found that perception of risk varies considerably and is more likely to be influenced by personal factors than by traditional cardiovascular risk factors. This suggests that more effective risk communication strategies are required to help the public to understand the importance and relevance of traditional cardiovascular risk factors.
We were interested to examine the perception of cardiovascular health in a male population in Brazil and to examine the relationship with traditional cardiovascular risk factors.
Methods
This study was an epidemiological, cross-sectional, descriptive, prospective study with a quantitative approach to information.
Data collection
Demographics and health habits
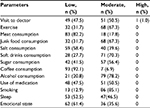
A 13-question questionnaire was constructed to obtain relevant information from participants about their health habits. Questions were agreed by a consensus process by the research team. Demographic data were also collected. Questions offered a variety of relevant set responses (Figure 1).
  | Figure 1 Graphical representation of (A) perceived stress, (B) perceived health status, and (C) perceived heart attack risk in the study population. |
Perceived health status
In order to examine the levels of stress and perceived health, the following three self-report questions were used, 1) On a scale of 1–5, how would you rate your stress level? (1= no stress at all and 5= extremely high stress; 2) How would you say you general health is? (excellent, very good, good, fair, or poor; 3) On a scale of 1–5, how likely is it that you will have a heart attack in your lifetime? (1= least likely and 5= most likely). For the purposes of analysis, high perceived stress was defined as a score of 4 or 5; low perceived stress was defined as a score of 1–3; high perceived health was defined as excellent, very good, or good; low perceived health was defined as fair or poor; low perception of heart attack risk was defined as a score of 1–3; and high perception of heart attack risk was defined as a score of 4 or 5 (Figure 1).
Physical examination
A physical examination was conducted for each participant, which included height, weight, abdominal circumference, systolic and diastolic pressure, and pulse rate.
Biological samples
Blood samples were also taken from all participants. Low-density lipoprotein (LDL), high-density lipoprotein (HDL), cholesterol, blood glucose, and prostate-specific antigen (PSA) levels were measured according to standard clinical laboratory procedures.
Sample population
To ensure that the results of the study were accurately reflective of the representative sample, a simple random convenience sample was collected at the men’s health campaign (Blue November in 2013). Participants were enrolled into the study if they fulfilled the following criteria: men, aged ≥40 years, member of Masonic lodge, and agree to participate in the study by signing the informed consent form.
Ethical considerations
The study was conducted to comply with the code of ethics and was approved by the Ethics Committee of the Federal University of Roraima (number: 1799613.2.0000.5302, 12/18/2013). Informed consent was obtained from all participants, and the welfare and interest of all respondents were taken into consideration throughout the study.
Data description
The qualitative data from the questionnaire were entered into a specifically designed Microsoft Excel spreadsheet. Statistical analysis was conducted using SPSS Version 22 (IBM Corporation, Armonk, NY, USA). Descriptive statistics were used to present the demographic and survey data according to the questionnaire categories. The risk of developing coronary artery disease was calculated according to the Framingham score.4 Data were compared between participants with and without biological sample data using Student’s t-test and the chi-square tests. Risk factors associated with medium and high risks for the development of coronary artery disease risk were examined. Correlations between the physical, demographic, social, cultural, economic, and health history with the severity of hypertension factors were explored. To examine correlation of risk with the survey data, each variable was grouped into three classes – low, medium, and high where, for example, low represented no caffeine intake, medium represented moderate caffeine intake, and high represented frequent/high caffeine intake. Correlations were examined using the chi-square test, with Cramer’s V correction for multiple categories. Correlations between biological variables were examined using Pearson’s r bivariate correlation coefficient. Significance was set at the P<0.05 level.
Results
Within Boa Vista, there are 820 masons, residing in 100 lodges. A total of 135 men participated in this study. Of these, 34 were below the age of 40 years and were therefore excluded from the analyses herein. The average age of the study population was 55.35±9.17 years, with a range of 40–80 years. The majority of participants were single (71.3%) or in a stable union (17.8%), had dark (37.6%) or brown (30.7%) skin, and reported to be Catholic (71.3%). Half of participants had completed high-grade school (49.5%).
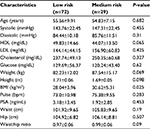
The participants had an average height of 1.71±0.06 m, an average weight of 83.72±13.12 kg, and an average body mass index (BMI) of 28.77±4.51 kg/m2 (Table 1). The majority of masons were classified as either overweight (41.2%, n=40) or obese (36.1%, n=35), with only a fifth of masons having a BMI in the normal range (21.6%, n=21) and none classified as underweight. The mean abdominal circumference of participants was 102.92±11.37 cm, with a range of 81–156 cm. The average systolic pressure was 144.78±19.63 mmHg, average diastolic pressure was 84.82±10.54 mmHg, and the average heart rate was 73.68±10.60 beats/min. The majority of participants (n=58, 59.8%) were classified as prehypertensive (systolic pressure >120 mmHg or diastolic pressure >80 mmHg), while 33% (n=32) were classified as hypertensive (systolic pressure >140 mmHg or diastolic pressure >90 mmHg).
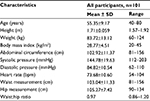  | Table 1 Physical characteristics of study population Abbreviation: SD, standard deviation. |
The survey data from the study are summarized in Table 2. Overall, the masons who participated in the study reported to adhere to a healthy lifestyle. The majority (64.4%) reported to exercise three or more times a week, with only a third taking no exercise apart from normal daily activity. Most (82.2%) avoided the consumption of red meat, while no participants reported high consumption or excessive addition of salt to foods. Similarly, none of the masons reported excessive consumption of soft drinks, sugar, or alcohol, although most consumed these items in moderate amounts approximately three times per week. Coffee consumption was also extremely low, with 92.1% reporting to never or rarely drinking coffee. The majority (85.1%) smoked occasionally, with only 12.9% reporting to have never smoked or to have smoked for a short time >5 years ago. Use of medication was uncommon, with no masons reporting daily use of medication. Most (52.5%) slept without any difficulties, and most were rarely nervous or stressed (61.4%). No masons reported to have had previous signs of depression or panic. Only one participant reported to regular visits to their doctor, with half only visiting when absolutely necessary, and the remaining 47.5% visiting between every 6 months and 12 months.
  | Table 2 Summary of survey data for all participants |
In order to understand the relationship between perceived and actual health status, the masons also answered three questions about their levels of stress and perceived health status. The majority of masons had low perceived stress (66.3%, n=67), high perception of their overall general health (63.4%, n=64), and low perceived risk of heart attack (71.3%, n=72). There was a significant relationship between the outcomes of the three questions. Masons who perceived a high level of stress and masons who perceived a lower overall level of general health were significantly more likely to have a high perceived risk of heart attack (P=0.003 and P=0.041, respectively). Masons who perceived a high level of stress were significantly more likely to have a lower perception of their overall health (P<0.001).
All participants underwent blood testing for cholesterol, HDL, LDL, glucose, and PSA levels. Results of these tests are presented in Table 3. The majority of participants had levels that fell within the desirable ranges (cholesterol ≥240 mg/dL, 91.9%, n=49/101; HDL <40 mg/dL, 83.6%, n=31/101; LDL <100 mg/dL, 53.2%, n=16/101; glucose 60–99 mg/dL, 68.8%, n=29/101; and PSA [total] <2.5 ng/mL, 85.8%, n=77/101).
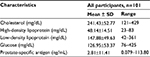  | Table 3 Biological characteristics of study population Abbreviation: SD, standard deviation. |
Biological and physical data were used to calculate the Framingham risk score for the population. Framingham scores ranged from -3 to 12, with a mean score of 3.86±3.16. A total of 38 participants (42.2%) had a score between -3 and 5, which equates to a low (<10%) risk of CVD, 43 participants (47.8%) had a score between 6 and 8, equating to a medium (11%–18%) risk, and nine participants (10.0%) had a score of 9 or more, equating to a high (>20%) risk of CVD.
We examined the relationship of demographic, physical, and biological factors to Framingham risk score and to responses to the “stress” tests. As would be expected since they are used for the calculation of Framingham score, age and systolic pressure were significantly associated with cardiovascular risk (Table 4). There was also a significant relationship with heart rate (P=0.002). There was a trend toward an association with glucose levels, although this did not reach significance perhaps due to the very small number of respondents classed as having a high Framingham risk. No association was found between cardiovascular risk and height, weight, or BMI, although there was a significant relationship with waist:hip ratio (P=0.048). No associations with Framingham risk were observed with any of the demographic factors or with responses to any of the 13 survey questions.
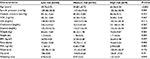
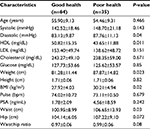
No significant differences were found in demographic and biological characteristics with relationship to level of perceived stress. However, participants who rated their overall general health as regular or bad were more likely to be overweight (P=0.023), have larger waist measurements (P=0.030), higher diastolic pressure (P=0.04), and lower HDL (P=0.011) measurements (Table 5). Masons who were overweight were also significantly more likely to perceive themselves to be at risk of a heart attack (P=0.025), although no differences were observed in any other variables (Table 6). There was no correlation between perceived stress, perceived health status, or perceived risk of a heart attack and Framingham risk score.
No relationship was observed between perceived risk of a heart attack and marital status, religion, number of children, or skin color. Similarly, there was no relationship between any of these factors and perceived stress and perceived health status. We also analyzed the relationship between questionnaire answers and perceived and actual health status. We found that masons who did not feel anxious were significantly more likely to perceive themselves to be not at risk of a heart attack (P=0.029). There was a trend toward people who did not have difficulties in sleeping, reporting overall better health (P=0.056). Masons who did not exercise were more likely to report that they perceived their overall health to be good (P=0.044). As may be expected, there was a statistically significant relationship between the two stress questions, with people answering that they were never or rarely anxious more likely to report low overall stress levels (P=0.023).
The strength of association between biological variables was further examined using Pearson’s r bivariate correlation coefficient. Age was found to be positively correlated with systolic pressure (P=0.002, r=0.306), PSA levels (P=0.028, r=0.220), and waist:hip ratio (P=0.006, r=0.272). Both diastolic and systolic pressures were positively correlated with weight (P=0.001, r=0.341 and P<0.001, r=0.343, respectively) and abdominal circumference (P<0.001, r=0.434 and P<0.001, r=-0.429, respectively), while diastolic pressure was also positively correlated with glucose levels (P=0.031, r=0.216). Abdominal circumference was positively correlated with heart rate (P=0.007, r=0.267) and, as may be expected, waist:hip ratio (P<0.001, r=0.761). Heart rate was positively correlated with glucose levels (P=0.002, r=0.305), cholesterol was positively correlated with LDL levels (P<0.001, r=0.849), and HDL levels were negatively correlated with waist:hip ratio (P=0.025, r=-0.225).
Discussion
In this study of Masonic men from Boa Vista, we found that perceived health level, including perceived stress and perceived risk of a heart attack, was in general not related to traditional risk factors for CVD. This study builds on our previous study of men in Boa Vista, which found a high incidence of obesity and hypertension, and suggested that within Boa Vista, Brazil, these were two key areas on which health campaigns for reducing CVD should focus.
We found some differences between our two studies. The Masonic men in this study were in general heavier and had a worse health profile, including higher systolic and diastolic pressures and higher cholesterol and glucose levels than in our previous study, which provided a more general picture of men’s health in Boa Vista. Consequently, a greater proportion of the men in our study had a moderate or high Framingham risk score, with only 39% classified as low risk compared to 59% in our previous study. Despite this, we observed an opposite trend in terms of responses to the lifestyle questionnaire. Masonic men were more likely to report that they exercised regularly and perceived themselves to have a healthier diet, with low consumption of red meat, junk food, and sugar, and were less likely to smoke or consume alcohol. It is unclear whether the Masonic populations have a belief that their diet is perhaps healthier than it really is, or if there are other factors that may result in reduced health status, despite an apparently healthy lifestyle.
Our findings are in line with previous studies, which have suggested that an “optimism bias” exists in which people underestimate their own risk of CVD.10 One study demonstrated that while women were more aware of CVD as a major cause of mortality, the majority had failed to translate this information into determining their own risk of CVD.11 While the only association with perceived risk that we observed in our study was with obesity, previous studies have identified association of perceived risk with race, socioeconomic status, and family history.12–15 However, in line with previous studies, we did find that people who perceived their overall general health to be lower were more likely to perceive themselves to have a higher risk of CVD.
There were limitations to this study. The study population was fairly small and as a result there were only a small number of men within certain categories; as such, results should be interpreted with some caution. There are some factors, such as insulin sensitivity and family history of CVD, which we were unable to collect and which may also be important. It is possible that associations were missed due to the limited study size. Further work is required to generalize the findings of this study across the male population within Brazil. The selection of masons in this study may have introduced some bias within the study, due to the uniqueness of this population and potential deviations from the general population. This is reflected in the differences observed between the characteristics of the men included in this study and those included in our previous study. Moreover, it is perceived that multivariable analysis may be useful to evaluate the prevalence of metabolic syndrome in the study population and the effect of family history of CVD, high self-reported stress, and low perceived health. However, we are unable to undertake this analysis as such data were not collected and will be undertaken in future.
Despite the limitations of the study, our findings have important implications. We observed that although over half of participants had a moderate to high risk of CVD according to traditional risk factors, less than a third perceived themself to be at high risk. Previous studies have indicated that awareness of cardiovascular risk level is an important motivating factor for people to make lifestyle changes in order to reduce their cardiovascular risk, such as improved diet or increased exercise.16–19 However, in people with low perception of their risk, motivation is considerably reduced.20 Our study suggests that despite health campaigns to increase public awareness of cardiovascular risk factors in Brazil, this has not translated into people’s perception of their own risk.
CVD has been the leading cause of death in Brazil for over half a century. Although improvements in health care have led to a reduction in cardiovascular mortality over recent years, it remains responsible for 31% of all deaths and 42% of noncommunicable disease deaths.21 CVD is also responsible for 8.3% of hospitalizations and represents a major cost to the health-care system.21 In order to improve cardiovascular health among men in Brazil, work is needed to ensure that public health campaigns communicate the significance of traditional cardiovascular risk factors in a way that improves the awareness of risk among the general population and leads to a more accurate perception of risk by individuals.
Acknowledgments
We acknowledge the assistance of Magna Bezerra Feitosa in the collection of data. Additionally, this work was done with institutional support of Roraima’s mason, and there was no external funding.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organisation [webpage on the Internet]. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: World Health Organisation; 2008. Available from: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf. Accessed January 20, 2015. | ||
Dawber TR, Meadors GF, Moore FE Jr. Epidemiological approaches to heart disease: the Framingham Study. Am J Public Health Nations Health. 1951;41(3):279–281. | ||
Kannel WB, McGee D, Gordon T. A general cardiovascular risk profile: the Framingham Study. Am J Cardiol. 1976;38(1):46–51. | ||
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847. | ||
Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. | ||
Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935–2959. | ||
Mosca L, Banka CL, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115(11):1481–1501. | ||
National Cholesterol Education Program. Expert panel on detection E, treatment of high blood cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood Cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. | ||
Petr EJ, Ayers CR, Pandey A, et al. Perceived lifetime risk for cardiovascular disease (from the Dallas Heart Study). Am J Cardiol. 2014;114(1):53–58. | ||
Webster R, Heeley E. Perceptions of risk: understanding cardiovascular disease. Risk Manag Healthc Policy. 2010;3:49–60. | ||
Kling JM, Miller VM, Mankad R, et al. Go Red for Women cardiovascular health-screening evaluation: the dichotomy between awareness and perception of cardiovascular risk in the community. J Womens Health (Larchmt). 2013;22(3):210–218. | ||
Avis NE, Smith KW, McKinlay JB. Accuracy of perceptions of heart attack risk: what influences perceptions and can they be changed? Am J Public Health. 1989;79(12):1608–1612. | ||
Kreuter MW, Strecher VJ. Changing inaccurate perceptions of health risk: results from a randomized trial. Health Psychol. 1995;14(1):56–63. | ||
Marteau TM, Kinmonth AL, Pyke S, Thompson SG. Readiness for lifestyle advice: self-assessments of coronary risk prior to screening in the British family heart study. Family Heart Study Group. Br J Gen Pract. 1995;45(390):5–8. | ||
van der Weijden T, Bos LB, Koelewijn-van Loon MS. Primary care patients’ recognition of their own risk for cardiovascular disease: implications for risk communication in practice. Curr Opin Cardiol. 2008;23(5):471–476. | ||
Grover SA, Lowensteyn I, Joseph L, et al. Discussing coronary risk with patients to improve blood pressure treatment: secondary results from the CHECK-UP study. J Gen Intern Med. 2009;24(1):33–39. | ||
Grover SA, Lowensteyn I, Joseph L, et al. Patient knowledge of coronary risk profile improves the effectiveness of dyslipidemia therapy: the CHECK-UP study: a randomized controlled trial. Arch Intern Med. 2007;167(21):2296–2303. | ||
Mosca L, Mochari H, Christian A, et al. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113(4):525–534. | ||
Benner JS, Erhardt L, Flammer M, et al. A novel programme to evaluate and communicate 10-year risk of CHD reduces predicted risk and improves patients’ modifiable risk factor profile. Int J Clin Pract. 2008;62(10):1484–1498. | ||
Mochari-Greenberger H, Mills T, Simpson SL, Mosca L. Knowledge, preventive action, and barriers to cardiovascular disease prevention by race and ethnicity in women: an American Heart Association national survey. J Womens Health (Larchmt). 2010;19(7):1243–1249. | ||
Ribeiro AL, Duncan BB, Brant LC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular health in Brazil: trends and perspectives. Circulation. 2016;133(4):422–433. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.