Back to Journals » Clinical Interventions in Aging » Volume 16
Association Between High-Sensitivity Troponin T on Admission and Organ Dysfunction During Hospitalization in Patients Aged 80 Years and Older with Hip Fracture: A Single-Centered Prospective Cohort Study
Authors Qin ZJ , Wu QY, Deng Y, Li X, Wei XD , Tang CJ, Jia JF
Received 22 January 2021
Accepted for publication 12 March 2021
Published 6 April 2021 Volume 2021:16 Pages 583—591
DOI https://doi.org/10.2147/CIA.S303246
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Zhi-Jun Qin,1 Qian-Yun Wu,1 Yang Deng,1 Xia Li,2 Xuan-Di Wei,2 Cheng-Jie Tang,3 Jun-Feng Jia3
1Department of Intensive Care Unit, Sichuan Provincial Orthopedic Hospital, Chengdu, Sichuan, People’s Republic of China; 2Department of General Medicine, Sichuan Provincial Orthopedic Hospital, Chengdu, Sichuan, People’s Republic of China; 3Department of Geriatric Orthopedics, Sichuan Provincial Orthopedic Hospital, Chengdu, Sichuan, People’s Republic of China
Correspondence: Zhi-Jun Qin
Department of Intensive Care Unit, Sichuan Provincial Orthopedic Hospital, No. 132, West First Section, First Ring Road, Chengdu City, Sichuan Province, 610041, People’s Republic of China
Tel +86 − 18728179291
Email [email protected]
Background: Prognostic evaluation of elderly patients with hip fracture is an issue that has been highly concerned by clinicians. Only a few studies have focused on organ dysfunction after hip fracture in the elderly. This study aimed to investigate the association between high-sensitivity troponin T (hs-TnT) at admission and organ dysfunction during hospitalization in elderly patients with hip fracture.
Methods: We enrolled 168 patients with hip fracture who were aged 80 years and older at Geriatric Orthopaedic Center of Sichuan Provincial Orthopedic Hospital between January 2020 and August 2020. Baseline characteristics, perioperative information, and short-term clinical outcomes were analyzed.
Results: Of the 208 patients admitted during the study period, 168 met the inclusion criteria; of these, 91 (54.2%) had higher hs-TnT than the 99th percentile in the normal population. After adjustment for confounders, elevated hs-TnT was independently associated with multiple organ dysfunction syndrome in the elderly (MODSE) (adjusted OR, 5.76; 95% CI, 1.74– 19.10; P = 0.004), heart dysfunction (adjusted OR, 7.48; 95% CI, 2.17– 25.82; P = 0.001), MODS severity score > 3 (adjusted OR, 5.22; 95% CI, 1.32– 20.60; P = 0.018), and length of hospital stay > 14 days (adjusted OR, 2.38; 95% CI, 1.05– 5.36; P = 0.037).
Conclusion: Increased hs-TnT on admission is an independent risk factor for MODSE after hip fracture in patients aged 80 years and older. Effective measures should be applied to avoid progression of MODSE from pre-failure stage to failure stage.
Keywords: high-sensitivity troponin T, hip fracture, multiple organ dysfunction syndrome in the elderly, short-term outcomes
Introduction
As the aging process accelerated, hip fracture in the elderly has become a global issue where prevalence in China is increasing fourfold per decade and nearly 30% of these are 80 years and older. Surgical intervention should be performed within 48 hours after fracture to reduce complications and mortality in these patients, and a large number of clinical practices have also confirmed the significant benefit of early surgery.1–3 However, the preoperative pathophysiological changes in the elderly are a critical part that has to be carefully considered. Inadequate preoperative assessment or optimization inevitably increases perioperative complications, while “overassessment” often leads to delayed or lost timing of surgery.
Many evaluation systems have now been applied for the prediction for postoperative complications and mortality risk in hip fracture, and some studies also use clinical laboratory findings at admission (such as hemoglobin concentration, peripheral blood lymphocyte count, etc.) as predictors for postoperative adverse events.4–7 hs-TnT, as a marker of myocardial injury, has been widely used in the diagnosis and prognostic evaluation of acute coronary syndrome(ACS) and has been confirmed to be associated with the prognosis of many non-coronary diseases such as sepsis, chronic obstructive pulmonary disease, and acute ischemic stroke.8–12 However, there are little studies on the effect of hs-TnT on the short-term prognosis of elderly patients with hip fracture. The purpose of this study was to investigate the association between hs-TnT and organ dysfunction and provide early warning to patients aged 80 years and older with hip fracture.
Methods
Study Design and Population
This is a single-centered prospective observational cohort study that included consecutive elderly patients with femoral neck or intertrochanteric fracture admitted to the Geriatric Orthopaedic Center of Sichuan Provincial Orthopedic Hospital, Chengdu, China between January 2020 and August 2020. The inclusion criteria were: patients diagnosed with femoral neck or intertrochanteric fracture and aged ≥ 80 years; history of definite trauma. The exclusion criteria were: pathological fracture caused by bone tumor, osteoma-like lesion; periprosthetic fracture, old fracture; previous ipsilateral hip fracture or surgery history; polytrauma and multiple fractures; the interval from fracture to surgery (time-to-surgery) exceeded 14 days; conservative intervention (non-surgical treatment); discharge against medical advice or transfer to another hospital during hospitalization; lack of follow-up data on the 28th day after surgery. Plasma hs-TnT was measured using the Elecsys Troponin T hs STAT assay (Roche, Germany, Lot 48,625,201) on a Cobas instrument. The manufacturer’s recommended 99th percentile level of hs-TnT is 14 pg/mL. Based on the hs-TnT values at admission, patients were divided into low-risk group (hs-TnT ≤ 14 pg/mL, group L) and high-risk group (hs-TnT > 14 pg/mL, group H).
The study was approved by the Ethics Commission of Sichuan Orthopaedic Hospital (approval number, KY2020-032-01) and the requirement for informed consent was exempted since this was an observational study where no attempt was made to change the standard of care.
Data Collection
The Geriatric Orthopaedic Center of Sichuan Provincial Orthopedic Hospital contains 108 beds and consists of three medical units (general ward, High Dependency Unit, and Intensive Care Unit), where the co-management model is implemented by orthopedic surgeons, physicians, and intensivists. Patients aged 80 years and older with hip fracture are routinely admitted to the Intensive Care Unit for postoperative monitoring and treatment on the day of surgery. On the first postoperative day, patients are downgraded to High Dependency Unit or general ward unless the occurrence of conditions requiring organ function support.
All data were prospectively measured and recorded in electronic medical records. Admission baseline status contained demographic data, type of fracture, comorbidities, function grading of vital organs, and vital signs. In addition, red cell distribution width (RDW), as an indicator of a patient’s physiologic reserve, was included in the evaluation of baseline status.13 Perioperative information included time-to-surgery, duration of operation, non-surgical intervention on the day of surgery and laboratory findings on the first day after surgery. We identified organ dysfunction during hospitalization as the primary clinical outcome, including the occurrence of single organ dysfunction and MODSE. In addition, MODS severity score, length of hospital stay (LOS) and 28-day mortality were collected.
Organ Function Assessment
It is part of preoperative management for all elderly patients with hip fracture to receive basal organ function assessment on admission, which is performed by two experienced physicians. Information on basal organ function was obtained from either the patients or their main caregivers. Stages of Heart Failure, modified British Medical Research Council dyspnoea scale (mMRC), Water Swallow Test (WST), Mini-Mental State Examination (MMSE) and Barthel Index were used to evaluate cardiac, respiratory, swallowing, cognitive function and self-care ability of patients, respectively.14–16 The diagnostic criteria for single organ dysfunction or MODSE during hospitalization and MODS severity score were based on the Diagnostic Criteria for Multiple Organ Dysfunction Syndrome in the Elderly (MODSE) (draft, 2003) and Replacing “Lushan conference in 1995” guideline of the staging diagnosis and severity score standard of multiple organ dysfunction syndrome (2015) (Table 1).17,18 As pulmonary artery wedge pressure (PAWP) was not readily available in daily clinical practice, we used lung ultrasound findings as an alternative to PAWP referring to the previous study.19
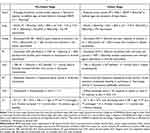 |
Table 1 Diagnostic Criteria for MODSEa |
Statistical Analysis
Patient characteristics were reported as means with standard deviations (normal distribution) or medians with interquartile ranges (skewed data), and we used the Student’s t-test or Mann–Whitney U-test to compare differences between group L and group H, as appropriate. Categorical variables were expressed as percentages and compared using the Chi-squared test. The associations between hs-TnT and clinical outcomes were estimated with univariate and multivariate logistic regression models and reported as odds ratios (ORs) with 95% confidence intervals (CIs). Considering the collinearity between Stages of Heart Failure, and chronic heart disease and hs-TnT, as well as between mMRC and chronic lung disease, the multivariate regression model included the following covariates: age, sex, type of fracture, time-to-surgery, hypertension, diabetes, chronic central nervous system disease, chronic kidney disease, mMRC, WST, MMSE, Barthel index, RDW, vital signs. Statistical analyses were performed using SPSS24.0 software and significance was assumed at P < 0.05.
Results
01-JAN-2020 to 31-AUG-2020, 208 patients aged 80 years and older with hip fracture were hospitalized in the Geriatric Orthopaedic Center of Sichuan Orthopaedic Hospital, among which 6 patients did not undergo surgical treatment, 9 patients had fracture at other sites, 8 patients had periprosthetic fracture, 13 patients had time-to-surgery exceeded 14 days, and 4 patients were discharged against medical advice. Forty patients were excluded, and a total of 168 patients were finally included in the statistical analysis. Among the included patients, 46 (27.4%) were male and 122 (72.6%) were female, aged 80–99 years, with a mean age of (86.0 ± 4.4) years, and all patients were admitted for hip fractures due to falls. The value of 168 patients at admission was 16.0 (11.0, 14.0) pg/mL, the minimum and maximum values were 5 pg/mL and 294 pg/mL, respectively, and 91 cases (54.2%) were higher than the reference value. None of the patients had definite evidence of acute coronary syndrome (ACS) during hospitalization. According to the hs-TnT level at admission, 168 patients were divided into group L (n = 77) and group H (n = 91).
Compared with group L, group H had older age (P = 0.001), more males (P < 0.001), more chronic kidney disease (P = 0.016), higher proportion in stages B and C of heart failure (P < 0.001), and worse swallowing and cognitive function on admission (P = 0.014, 0.004, respectively) (Table 2).
 |
Table 2 Baseline Characteristics and Differences Between Low-Risk Group and High-Risk Group |
The following parameters were significantly higher/longer on the first postoperative day in group H: time-to-surgery (P = 0.029), neutrophil-to-lymphocyte ratio (NLR) (P < 0.001), prothrombin time (P = 0.024), international normalized ratio (P = 0.024), pro-brain natriuretic peptide (pro-BNP) (P < 0.001), hs-TnT (P < 0.001), procalcitonin (P = 0.027), interleukin-6 (P = 0.022), creatinine (P = 0.001), cystatin C (P < 0.001), and blood uric acid (P = 0.008); the following parameters were significantly lower: peripheral blood lymphocyte count (P = 0.003), and standard bicarbonate (P = 0.007) (Table 3).
 |
Table 3 Perioperative Information and Differences Between Low-Risk Group and High-Risk Group |
The lung, central nervous system (CNS), and heart were the most commonly involved organs (Figure 1). Respiratory dysfunction was mainly induced by infection, delirium was the main manifestation of CNS dysfunction, and cardiac dysfunction was almost an acute exacerbation of chronic heart disease. The incidences of MODSE and heart dysfunction in group H were significantly higher than those in group L (P = 0.002, 0.006, respectively). Thirty-nine patients (23.2%) met the diagnostic criteria for MODSE, 35 remained in the pre-failure stage and 4 eventually progressed to the failure stage. Three of the 4 patients in the failure stage died within 28 days, including 2 cases of respiratory failure with cardiogenic shock and 1 case of massive cerebral infarction with respiratory failure.
Patients with MODSE, single organ dysfunction (except lung, peripheral circulation, gastrointestinal tract, coagulation system), MODS severity score > 3 and LOS > 14 days had significantly higher mean hs-TnT values on admission (Table 4). After adjustment for confounders (age, sex, type of fracture, time-to-surgery, hypertension, diabetes, chronic CNS disease, chronic kidney disease, mMRC, WST, MMSE, Barthel index, RDW, vital signs), elevated hs-TnT was independently associated with MODSE (adjusted OR, 5.76; 95% CI, 1.74–19.10; P = 0.004), heart dysfunction (adjusted OR, 7.48; 95% CI, 2.17–25.82; P = 0.001), MODS severity score > 3 (adjusted OR, 5.22; 95% CI, 1.32–20.60; P = 0.018), and length of hospital stay > 14 days (adjusted OR, 2.38; 95% CI, 1.05–5.36; P = 0.037) (Table 4).
 |
Table 4 Admission High-Sensitivity Troponin T and Perioperative Outcomes |
Discussion
In elderly patients with hip fracture, the functional status of vital organs is the important prerequisite of surgical treatment, the basis of enhanced recovery after surgery, and the goal and guidance of restoring lower limb function. These patients are inevitably associated with chronic organ dysfunction prior to injury, and MODSE after injury and/or surgery is mostly a continuation or exacerbation on a chronic basis. Unlike adult MODS, MODSE has its particularities including organ aging, comorbidities, decreased physiological reserves of many organs, insidious symptoms and signs, and protracted course, etc.20 Wang et al proposed diagnostic criteria for MODSE according to the characteristics of elderly patients, in which MODSE was divided into pre-failure and failure stages.17 The criteria for MODSE were met in 23.2% of the cases in this study, and although most of them (89.7%) were in the pre-failure stage, a high 28-day mortality (75%) occurred once MODSE progressed to the failure stage. It is therefore to be certain that effective early warning system/indicator on MODSE would be important components in preoperative assessment and management. At present, there are many studies of the prediction on short- or long-term mortality in elderly patients with hip fracture, and the early warning system/indicator on perioperative MODSE has rarely been reported.4–7 In addition, the conceptualization of “adverse events” or “complications” in the aforementioned study was difficult to define and standardize. As a classical marker of myocardial injury, hs-TnT has been widely used in the diagnosis, stratification and prognostic evaluation of ACS. Moreover, a variety of pathological factors can lead to myocardial injury and hs-TnT should be considered an organ-specific rather than disease-specific biomarker.21 Low-level elevated hs-TnT is prevalent in elderly non-ACS patients.22 Previous studies showed that hs-TnT was higher than 14 pg/mL in 40–50% of elderly hospitalized non-ACS patients and 79% of elderly residents in a nursing home.23,24 This study found that hs-TnT values of 168 patients at admission ranged from 5 to 294 pg/mL with a median of 16.0 pg/mL, and 54.2% of the cases exceeded 14 pg/mL. In addition to poor baseline conditions, factors such as acute trauma, blood loss, and pain caused by hip fracture may be associated with hs-TnT abnormalities at admission.
In this study, patients were divided into two groups based on the 99th percentile in the normal population of hs-TnT and only low-level increased hs-TnT was found in group H. However, there were significant differences in baseline status of admission, perioperative conditions and short-term clinical outcomes between two groups. It was noteworthy that these differences showed a strong inherent relationship and exhibited the continuity of disease development. Differences in baseline status can be explained as follows: although the symptoms were insidious, cardiac failure with preserved ejection fraction was extremely common with increasing age, which often resulted in marked hemodynamic disturbance and was more likely to adversely affect renal function and cognitive competence.25,26 Definitions such as “cardiorenal syndrome” and “cardiogenic dementia” indicated the interconnection between various organ functions.27 Swallowing disorder was similarly associated with advanced age, cognitive impairment and poor cardiac and pulmonary function, and might be aggravated by prolonged bed rest, malnutrition, and debilitation after fracture.28–30 Secondly, higher pro-BNP, hs-TnT, creatinine, cystatin C, serum uric acid and lower standard bicarbonate on the first postoperative day indicated poorer cardiac and renal function in group H. These laboratory findings might be either continuation of chronic organ dysfunction before fracture or signs of subsequent MODSE. Notably, the NLR on the first postoperative day was at a high level in all patients[7.6 (5.1, 10.2)], the rise of NLR was more significant [8.9 (6.2, 11.3)] in group H, accompanied by increased inflammation indicators and decreased peripheral blood lymphocyte count. NLR is considered to be a comprehensive variable reflecting systemic inflammation-immune status and has been demonstrated to be associated with various pathological factors including chronic heart failure, chronic kidney disease, dementia, osteoporosis and even fracture itself. With the increase of NLR, the incidence of postoperative myocardial injury and infection increased exponentially.31 Abnormalities in NLR might clarify that patients in group H had worse baseline status and clinical prognosis from the perspective of systemic inflammation-immunity. Finally, the incidence of MODSE in group H rose significantly with a higher MODS severity score and longer hospital stay. Meanwhile, the incidence of heart dysfunction also increased significantly in group H, which became one of the main components of MODSE. MODSE initiated either in the period between fracture and surgery or within several days after hip fracture surgery. Patients in the pre-failure stage generally had a good prognosis if early and appropriate management was implemented, but a very high 28-day mortality occurred once they progressed to the failure stage. Therefore, effective preoperative assessment and management are important means to block or delay the MODSE process. As an independent factor for MODSE, heart dysfunction, MODS severity score > 3 and LOS > 14 days, increased hs-TnT may be regarded as an early warning indicator of short-term poor prognosis in hip fracture patients aged 80 years and older.
There are several limitations that deserve consideration: First, the 28-day mortality was not powered to assess and the association between 28-day mortality and hs-TnT was not evaluated because of the small sample size. Second, some patients were excluded from the study due to factors such as conservative treatment and prolonged time-to-surgery, and the clinical characteristics and short-term prognosis of such patients may require further study. Finally, despite statistical adjustments, there remained a possibility of residual confounding in all observational studies.
Conclusion
In summary, a low-level increase of hs-TnT at admission was not uncommon, which could be used as an early warning indicator for perioperative MODSE in patients aged 80 years and older with hip fracture. Patients with elevated hs-TnT had worse vital organ functions at baseline and were more likely to be induced to MODSE by acute stress factors such as trauma, surgery and blood loss. Effective measures should be applied to avoid the occurrence of MODSE failure stage.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Commission of Sichuan Orthopaedic Hospital (approval number, KY2020-032-01) and the requirement for informed consent was exempted. We confirmed that all procedures followed were in accordance with the Helsinki Declaration and patient data was maintained with confidentiality.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Leer-Salvesen S, Engesæter LB, Dybvik E, Furnes O, Kristensen TB, Gjertsen JE. Does time from fracture to surgery affect mortality and intraoperative medical complications for hip fracture patients? An observational study of 73 557 patients reported to the Norwegian hip fracture register. Bone Joint J. 2019;101-B(9):1129–1137. doi:10.1302/0301-620X.101B9.BJJ-2019-0295.R1
2. Beaupre LA, Khong H, Smith C, et al. The impact of time to surgery after hip fracture on mortality at 30- and 90-days: does a single benchmark apply to all? Injury. 2019;50(4):950–955. doi:10.1016/j.injury.2019.03.031
3. Espinosa KA, Gélvez AG, Torres LP, García MF, Peña OR. Pre-operative factors associated with increased mortality in elderly patients with a hip fracture: a cohort study in a developing country. Injury. 2018;49(6):1162–1168. doi:10.1016/j.injury.2018.04.007
4. Jonsson MH, Bentzer P, Turkiewicz A, Hommel A. Accuracy of the physiological and operative severity score for the enUmeration of mortality and morbidity score and the Nottingham risk score in hip fracture patients in Sweden – a prospective observational study. Acta Anaesthesiol Scand. 2018;62(8):1057–1063. doi:10.1111/aas.13131
5. Johns WL, Strong B, Kates S, Patel NK. POSSUM and P-POSSUM scoring in hip fracture mortalities. Geriatr Orthop Surg Rehabil. 2020;11:2151459320931674. doi:10.1177/2151459320931674
6. Laulund AS, Lauritzen JB, Duus BR, Mosfeldt M, Jørgensen HL. Routine blood tests as predictors of mortality in hip fracture patients. Injury. 2012;43(7):1014–1020. doi:10.1016/j.injury.2011.12.008
7. Yin P, Lv H, Li Y, et al. Hip fracture patients who experience a greater fluctuation in RDW during hospital course are at heightened risk for all-cause mortality: a prospective study with 2-year follow-up. Osteoporos Int. 2018;29(7):1559–1567. doi:10.1007/s00198-018-4516-7
8. de Groot B, Verdoorn RC, Lameijer J, van der Velden J. High-sensitivity cardiac troponin T is an independent predictor of inhospital mortality in emergency department patients with suspected infection: a prospective observational derivation study. Emerg Med J. 2014;31(11):882–888. doi:10.1136/emermed-2013-202865
9. Høiseth AD, Brynildsen J, Hagve TA, et al. The influence of heart failure co-morbidity on high-sensitivity troponin T levels in COPD exacerbation in a prospective cohort study: data from the akershus cardiac examination (ACE) 2 study. Biomarkers. 2016;21(2):173–179. doi:10.3109/1354750X.2015.1126645
10. Neukamm A, Einvik G, Didrik høiseth A, et al. The prognostic value of measurement of high-sensitive cardiac troponin T for mortality in a cohort of stable chronic obstructive pulmonary disease patients. BMC Pulm Med. 2016;16(1):164. doi:10.1186/s12890-016-0319-9
11. He L, Wang J, Dong W. The clinical prognostic significance of hs-cTnT elevation in patients with acute ischemic stroke. BMC Neurol. 2018;18(1):118. doi:10.1186/s12883-018-1121-5
12. Duchnowski P, Hryniewiecki T, Kuśmierczyk M, Szymański P. High-sensitivity troponin T predicts postoperative cardiogenic shock requiring mechanical circulatory support in patients with valve disease. Shock. 2020;53(2):175–178. doi:10.1097/SHK.0000000000001360
13. Duchnowski P, Hryniewiecki T, Kuśmierczyk M, Szymanski P. Red cell distribution width as a predictor of multiple organ dysfunction syndrome in patients undergoing heart valve surgery. Biol Open. 2018;7(10):bio036251. doi:10.1242/bio.036251
14. Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119(14):e391–e479. doi:10.1161/CIRCULATIONAHA.109.192065
15. Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988;93(3):580–586. doi:10.1378/chest.93.3.580
16. Nogueira D, Reis E. Swallowing disorders in nursing home residents: how can the problem be explained? Clin Interv Aging. 2013;8:221–227. doi:10.2147/CIA.S39452
17. Wang SW, Wang JD, Chen KJ, Wang YT, Wang XD, Mu CS. Diagnostic criteria of multiple organ dysfunction syndrome in elderly (Draft, 2003). Chin Crit Care Med. 2004;16(1):1. doi:10.3760/cma.j.issn.1003-0603.2004.01.001
18. Chinese Society of Combining Traditional Chinese and Western Medicine Professional Committee of Emergency Medicine. [Replacing “Lushan conference in 1995” guideline of the staging diagnosis and severity score standard of multiple organ dysfunction syndrome (2015)]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2016;28(2):99–101. Chinese. doi:10.3760/cma.j.issn.2095-4352.2016.02.002
19. Gargani L, Pang PS, Frassi F, et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: a lung ultrasound study. Cardiovasc Ultrasound. 2015;13:40. doi:10.1186/s12947-015-0033-4
20. Duchnowski P, Szymański P, Kuśmierczyk M, Hryniewiecki T. Usefulness of FRAIL scale in heart valve diseases. Clin Interv Aging. 2020;15:1071–1075. doi:10.2147/CIA.S239054
21. Park KC, Gaze DC, Collinson PO, Marber MS. Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc Res. 2017;113(14):1708–1718. doi:10.1093/cvr/cvx183
22. Zhang SJ, Wang Q, Cui YJ, et al. High-sensitivity cardiac troponin T in geriatric inpatients. Arch Gerontol Geriatr. 2016;65:111–115. doi:10.1016/j.archger.2016.03.010
23. Wu W, Li DX, Wang Q, Xu Y, Cui YJ. Relationship between high-sensitivity cardiac troponin T and the prognosis of elderly inpatients with non-acute coronary syndromes. Clin Interv Aging. 2018;13:1091–1098. doi:10.2147/CIA.S157048
24. Cardinaels EP, Daamen MA, Bekers O, et al. Clinical interpretation of elevated concentrations of cardiac troponin T, but not troponin I, in nursing home residents. J Am Med Dir Assoc. 2015;16(10):884–891. doi:10.1016/j.jamda.2015.06.026
25. Steinberg BA, Zhao X, Heidenreich PA, et al. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126(1):65–75. doi:10.1161/CIRCULATIONAHA.111.080770
26. de Pablos L, Jorge-Brito RA, Amarnani V, Jiménez-Sosa A, Harmand MG, Domínguez-Rodríguez A. Delirium in patients with heart failure: influence of attendance times in an emergency department. Rev Esp Cardiol (Engl Ed). 2019;72(1):82–84. doi:10.1016/j.rec.2017.10.045
27. Cannon JA, Moffitt P, Perez-Moreno AC, et al. Cognitive impairment and heart failure: systematic review and meta-analysis. J Card Fail. 2017;23(6):464–475. doi:10.1016/j.cardfail.2017.04.007
28. Yatabe N, Takeuchi K, Izumi M, et al. Decreased cognitive function is associated with dysphagia risk in nursing home older residents. Gerodontology. 2018;35(4):376–381. doi:10.1111/ger.12366
29. Ghannouchi I, Speyer R, Doma K, Cordier R, Verin E. Swallowing function and chronic respiratory diseases: systematic review. Respir Med. 2016;117:54–64. doi:10.1016/j.rmed.2016.05.024
30. Suttrup I, Warnecke T. Dysphagia in parkinson’s disease. Dysphagia. 2016;31(1):24–32. doi:10.1007/s00455-015-9671-9
31. Fisher A, Srikusalanukul W, Fisher L, Smith P. The neutrophil to lymphocyte ratio on admission and short-term outcomes in orthogeriatric patients. Int J Med Sci. 2016;13(8):588–602. doi:10.7150/ijms.15445
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

