Back to Journals » Open Access Surgery » Volume 14
Assessment of Manual Intraoperative Anesthesia Record-Keeping Practice at Dilla University Referral Hospital, Dilla, Ethiopia
Authors Zemedkun A , Mulugeta H , Getachew H, Destaw B, Mola S , Milkias M
Received 21 December 2020
Accepted for publication 4 February 2021
Published 16 February 2021 Volume 2021:14 Pages 1—7
DOI https://doi.org/10.2147/OAS.S298387
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Luigi Bonavina
Abebayehu Zemedkun, Hailemariam Mulugeta, Hailemariam Getachew, Belete Destaw, Simeneh Mola, Mesay Milkias
Department of Anesthesiology, College of Health Sciences and Medicine, Dilla University, Dilla, Ethiopia
Correspondence: Abebayehu Zemedkun
College of Health Sciences and Medicine, Dilla University, P.O Box: 419, Dilla, Ethiopia
Tel +251900053426
Email [email protected]
Introduction: Clinical record-keeping is a crucial part of professional practice and the delivery of quality healthcare. Poor intraoperative recording contributes to poor patient safety and unavailability of data in cases of medico-legal review or research purpose. Additionally, such records may provide an invaluable guide to subsequent practitioners involved with the patients’ management.
Method and Materials: A descriptive study was conducted at Dilla University Referral Hospital from October 1 to November 30, 2020. Fifty-one intraoperative record indicators were developed and those requiring a definition for completeness were predefined. The expected completion rate was 100% for all indicators. Indicators with > 90% completion rate were marked as acceptable and completion rate of < 50% was considered as areas of the critical need for improvement. SPSS version 20 was used for data analysis.
Results: A total of 164 intraoperative anesthesia record tools were reviewed, and none of the indicators had a completion rate of 100%. The intraoperative anesthesia record tools completion rate was > 90% for documentation of sex, procedure starting time, name of the procedure, dose/volume and route of a specific drug given, standards of monitoring used, intraoperative blood pressure, and pulse rate record with time. Patient identity, name of professionals, baseline oxygen saturation, unit of measures of baseline vital signs, patient’s status on transfer, the total amount of each drug administered, intraoperative electrocardiographic rhythm, total amount of blood loss, total amount of urine output, and postoperative management plan were among indicators found below average (< 50%) completion rate.
Conclusion and Recommendation: Most of the indicators for manual intraoperative anesthesia recording were found incomplete and below the standards. Different strategies like regular feedback and monitoring to improve the practice have to be instituted. Introducing an electronic recording system may also help to overcome the problem.
Keywords: intraoperative, documentation, practice, data quality, anesthesia
Introduction
Clinical record keeping is a crucial part of professional practice and the delivery of quality healthcare.1 Anesthesia documentation represents detailed information of the patient’s anesthesia care during pre-anesthesia assessment and evaluation, informed consent, intraoperative services, and postanesthesia care. The primary purpose of anesthesia documentation is to capture accurate and comprehensive information to communicate a patient’s anesthetic experience. Additionally, a formal record of anesthesia care is also referenced for medico-legal purposes, quality improvement, research purposes, and review by external organizations.2–4
Anesthetists are predisposed to different medico-legal issues. Some of the causes out of many are poor recording, and communication with other staff, patients, and relatives.5,6 To contribute to accuracy in medical records and to facilitate any future necessary chart review, anesthetists should ensure that accurate and thorough documentation is accomplished in all preoperative, intraoperative, and postoperative phases of anesthesia-related care.7,8
The intraoperative phase is a very stressful and busy moment for the anesthesia provider with the monitoring of critically ill patients and some teaching-learning activities that they may forget to record or record with poor quality. This may contribute to poor patient safety, unavailability of data in cases of medico-legal review or research purpose, afterward, which might breach continuity of care as it impairs the flow of patient information among practitioners.5,6,9–11 Workload, use of tools or manual recording, practitioner interest, and availability of information are some of the factors which affect the quality and practice of documentation.12 Furthermore, different studies showed that the level of manual anesthetic record completeness was substandard compared with the recommendations of the World Federation of Societies of Anaesthesiologists (WFSA) and Association of Anaesthetists of Great Britain and Ireland (AAGBI).7,12
Even though most of the hospitals in Ethiopia including Dilla University Referral Hospital (DURH) use manual (non-electronic) intraoperative anesthesia record tool (IART), the practice and completeness of the tool were not evaluated. The objective of this study was to assess the manual intraoperative anesthesia record keeping practice and completeness of the IARTs at DURH.
Methods and Materials
A descriptive study was conducted from October 1 to November 30, 2020 to assess the manual intraoperative anesthesia record keeping practice and completeness of the IARTs at DURH.
Dilla University Referral Hospital is located at Dilla town, Gedeo zone, South Nation, Nationalities and Peoples Region, in Southern part of Ethiopia at a distance of 360 km from Addis Ababa, the capital of the country. The hospital delivers comprehensive surgical care for admissions from surgical ward, emergency department, gynecology and obstetrics, pediatrics and orthopedic wards with full functioning four operating theatres. On average about 1200 patients undergo elective and emergency operation per year.
The currently available manual intraoperative anesthesia recording sheet has been in use at the DURH for more than seven (7) years. In the hospital, photocopy of IARTs is always kept in the operation theatre and the original record is attached to the patient’s chart. From IART of elective and emergency surgeries performed in the past one year at DURH, non-probabilistic (convenient) sampling technique was used to select 164 IARTs to assess the practice of manual intraoperative anesthesia record keeping. Since we evaluated the existing practice, and service delivered by fixed number of anesthesia staffs, we assumed the sample size gives sufficient information about the manual intraoperative anesthesia recording practice of DURH. To review these tools, checklist was developed based on a combination of criteria outlined by the American society of anesthesiologists (ASA),13 Australian and New Zealand College of Anesthetists (ANZCA),14 and mainly from the manual intraoperative record sheet of DURH. It was pilot tested and changes were made before the actual data collection. Fifty-one indicators were developed and checked as “Yes” for complete documentation or, “Incomplete” for partial documentation and “No” if left blank. The completeness of indicators was defined by components of the indicators (Table 1). The expected completion rate was 100% for all indicators. Indicators with >90% completion rate were marked as acceptable and completion rate of <50% was considered as areas of critical need improvement. The checklist was divided into 4 main parts based on the components of our hospital’s IART: completeness of the patients’ identity and baseline clinical information, intraoperative patient information, intraoperative medication, equipment and monitoring, and completeness of postoperative care. In DURH, Information like vital signs (BP, PR, and SPO2) is usually recorded on the IARTs from the integrated monitor. Other information are recorded from the patients chart, directly from the patient and other sources of information as needed.
 |
Table 1 Indicators Drawn from ASA, ANZCA and IART Used at Dilla University Referral Hospital |
Consent was waived by Dilla University institutional review board since we used secondary data. The data were collected after getting permission from the Dilla university referral hospital. The study was conducted in accordance with the declaration of Helsinki. All data were accessed, compiled, and secured by avoiding personal identifications and all the data were accessed for only the authors. Anonymity and confidentiality were secured at every step of this research. The data were checked, coded, entered, and cleaned using SPSS version 20. Descriptive analysis was performed. Narratives and tables were used to present the data and findings were expressed in the form of frequencies and percentages.
Result
A total of 164 manually filled IARTs were included in this audit from patients who had undergone surgery in DURH. Out of these, 71 (43.3%) and 93 (56.7%) were operated on under general and spinal anesthesia, respectively.
Indicators Related to Patient Identity, Preoperative, and Baseline Clinical Information
In the majority of IARTs, 149 (90.9%), the name of the patients including their last names was not recorded. In only 5 (3%) of the record sheets; the patients’ first, middle, and last names were recorded. In the remaining 10 (6.1%) of IARTS, the field for patient’s identity was left blank. The age of the patient was incomplete in a large number of IARTs, 139 (84.7%). Only on 16 (9.8%) of the tools, it was recorded in years or months. In the remaining 9 (5.5%) IARTs, the age of the patients was not recorded. The card numbers of patients were recorded in 140 (85.4%) of the reviewed tools and information about preoperative evaluation completeness was checked for 111 (67.7%) patients (Table 2).
Indicators Related to Intraoperative Information
Name of the surgeon, name of the anesthetist, and name of the circulator/scrub nurses had an incomplete record in 127 (77.4%), 123 (75%), and 116 (70.7%) of the tools, respectively. Either the middle name or the titles of the professionals were not recorded. Name of the surgeon (15.9%), name of anesthetist (18.3%), and name of circulator/scrub nurse (15.3%) were recorded completely. The IARTs completion rate of anesthesia and surgery starting times were 149 (90.9%) and 148 (90.2%), respectively (Table 3).
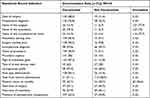 |
Table 3 Intraoperative Anesthesia Record Completion Rate Regarding Intraoperative Patient Information at Dilla University Referral Hospital. (Frequency and Percentage (n (%))), N= 164 |
Indicators Related to Intraoperative Medication, Equipment, and Monitoring
Among the reviewed IARTs, the site of IV cannula recording was incomplete in 69 (42.1%) of the tools. In only 60 (36.6%) of the IARTs, the exact anatomic site of the cannulation was recorded while it was not recorded in 35 (21.3%) of the tools. The intraoperative ECG rhythm record was complete in only 30 (35.3%) of the IARTs (ie, it was recorded in the whole intraoperative period) and 40 (47.1%) of the tools had no ECG rhythm recorded (Table 4).
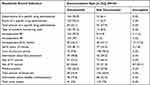 |
Table 4 Intraoperative Anesthesia Record Completion Rate About Intraoperative Medication, Equipment and Monitoring at Dilla University Referral Hospital (Frequency and Percentage (n (%))), N= 164 |
The completion rates of the IARTs were >90% for the dose/volume, route of a specific drug administered, intraoperative PR, and intraoperative BP record (93.9%, 93.3%, 97%, and 93.9%, respectively). The completion rates were below average for the other important indicators. For instance, the records of the total amount of urine output, information about care of pressure points, and the total amount of blood loss revealed 25%, 9.8%, and 35.4%, respectively (Table 4).
Indicators Related to Postoperative Plan and Order
This review of IARTs showed a below-average completion rate of postoperative pain management plan, 23 (14%), Postoperative fluid management plan, 13 (7.9%), and Postoperative nausea and vomiting management plan, 2 (1.2%). In 96 (58.5%) of the tools, a postoperative monitoring plan was forwarded.
Discussion
The study revealed that none of the indicators of IARTs had a completion rate of 100%. Patient identity, name of professionals, baseline oxygen saturation, unit of measures of baseline vital signs, total fluid volume administered, patient’s status on transfer, the total amount of each drug administered, intraoperative electrocardiographic rhythm, total amount of blood loss, total amount of urine output, and postoperative management plan were among indicators found below average (<50%) completion rate.
While it may be expected that demographic information and patient identification would be the most frequently documented data group, it was surprising to find that only a few tools (3%) have the complete name of the patient recorded in this study. The patient’s weight and BMI were not recorded in 88.4% and 98.8% of the IARTs, respectively. This indicates that the anesthetists placed minimal emphasis on the calculation of accurate drug doses, ventilation parameters, airway equipment size, and fluid requirement which directly affects the quality of anesthesia delivery and perioperative patient outcome. This finding was in line with previous studies from Ethiopia12 and Nigeria15 that showed a poor completion rate of demographic information of anesthesia record tools.
Baseline PR, BP, and SPO2 were recorded for 95 (57.9%), 103 (62.8%), and 78 (47.6%) of the IARTs, respectively. A clinical audit in Gondar, Ethiopia showed that pre-induction vital signs were recorded in 37.5% of patients.7 This might affect both the intraoperative management of the patients and lead to poor communication among different professionals.
Our study depicted that Only in few numbers of the IARTs, the name of the surgeon (15.9%), name of anesthetist (18.3%), and name of circulator/scrub nurse (15.3%) were recorded in the full name (first, second and last name). This was inconsistent with previous studies.7,16 The difference could have resulted from their consideration of the first and middle names as the full name of the professionals. Besides, the completion rate for total fluid volume administered, the patients’ status on transfer, and grade of laryngoscopic view were below average. This poor practice of documentation hugely deviated from the expected completion rate, so that, it would compromise the peri-operative surgical and anesthesia service quality, and may subsequently affect patient outcome. Relatively higher completion of IARTs of anesthesia starting time 149 (90.9%), and Surgery starting time 148 (90.2%) were seen in our study.
Even though information about the name of the surgical procedure was documented in >90% of IARTs, lower completion rate was seen for information about the intraoperative diagnosis, the urgency of the procedure, type of anesthesia given, type of airway devises used, the total time of surgery, and the total time of anesthesia. A similar finding was seen from Nigeria.16 This poor documentation might impact the subsequent management of patients and communication among different health care professionals.
Documentation of vital signs including clear units of measurement is a key component of intraoperative anesthesia recording.3 Even though, intraoperative BP and HR showed a completion rate of >90%, the recording practice for intraoperative ECG rhythm was below average (35.3%), which may impair early detection and management of intraoperative complications or events. Ige et al (2020) found that vital signs consisting of blood pressure and pulse rate were documented in 475 (58.93%) of the patient’s record.16 This difference could be due to the sample size, or eligibility criteria of the studies. Other studies also showed below-average completion rate of intraoperative vital sign record.7,10 This could be explained that they might have used a vital sign as a single variable or indicator. In our case, the completion rate of each component of the vital signs was assessed separately.
This study found that the IARTs completion rate was poor (below 50%) for information like the total amount of urine output, patient catheterization, total amount of blood loss, site of IV cannulation, eye protection, and care of pressure points and total amount of a specific drug given. This shows that the intraoperative patient monitoring and management were substandard in the majority of parameters which might contribute to poor perioperative patient outcomes in addition to compromising patient satisfaction. On the other hand, the IARTs recording rate was >90% for standards of monitoring used, dose/volume, and route of a specific drug given. This finding was in agreement with the previous studies.7,10,16
The AAGBI states that “the anesthetist must formally hand over the care of a patient to a recovery room nurse or other appropriately trained members of staff”.3 Even though postoperative order and management are one of the core components of perioperative patient management; our study found a very poor practice. This finding was in line with previous studies.3,7 This poor practice might significantly affect patient handover to other staff which in turn affects the subsequent management of the patient in post-anesthesia care unit or wards. Additionally, it might affect patient outcomes after surgery and anesthesia.
Generally, the practice of manual intraoperative anesthesia record keeping in our study was found poor with incomplete recording or no recording at all in most of the tools. In comparison with computerized record-keeping, manual record-keeping resulted in loss of clinically relevant information. Anesthesia information management system (AIMS) showed multiple advantages including improved accuracy of data collection for clinical documentation and research, enhanced quality of care and improved regulatory compliance.5,15,17 Therefore, introducing an electronic-based recording system in our case may improve patient safety, record keeping and patient management practice.
Although documenting of patient’s height, warming measures, heat moisture exchanger, completeness of anesthesia safety checklist, and peripheral nerve block detail are recommended as part of intraoperative anesthesia recording, the DURH recording tool lacks these assessment indicators.
Conclusion
Most of the indicators for intraoperative anesthesia recording were found incomplete and below the standards. Patient socio-demographic characteristics, professional’s identity, and intraoperative monitoring are among the contents of IARTs with poor completion rate.
Recommendation
The practice of manual intraoperative anesthesia record-keeping was poor. We recommend Different strategies like regular feedback and monitoring to improve the standards of documentation of this often neglected, but the essential scope of our clinical practice has to be instituted. Introducing an electronic recording system may also help to overcome the problem.
Limitation of the Study
This is a single-center study and difficult to generalize for other hospitals. Also, we used secondary data that may lack completeness.
Abbreviations
AAGBI, Association of Anesthetists of Great Britain and Ireland; ANZCA, Australian and New Zealand College of Anesthetists; ASA, American Society of Anesthesiologists; BMI, body mass index; BP, blood pressure; DURH, Dilla University Referral Hospital; ECG, electrocardiograph; IART, Intraoperative Anesthesia Record Tools; IV, intravenous; PR, pulse rate; SPO2, oxygen saturation.
Data Sharing Statement
All the required documents available at the hand of the corresponding author and can be supplied upon request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published. And All Authors have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was obtained for this work.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Mathioudakis A, Rousalova I, Gagnat AA, Titus C. How to keep good clinical records. Breathe. 2016;12(4):371–375. doi:10.1183/20734735.018016
2. Kadry B, Feaster WW, Macario A, Ehrenfeld JM. Anesthesia information management systems: past, present, and future of anesthesia records. Mt Sinai J Med. 2012;79:154–165. doi:10.1002/MSJ
3. Raymer K. The anesthetic record: how content and design influence function in anesthetic practice and beyond. J Anesth Clin Res. 2011;4(2):1–7. doi:10.4172/2155-6148
4. Pirie S. Documentation and record keeping. Open Learn Zo. 2011;21(1).
5. Van Schalkwyk JM, Lowes D, Frampton C, Merry AF. Does manual anaesthetic record capture remove clinically important data? Br J Anaesth. 2011;107(4):546–552. doi:10.1093/bja/aer163
6. Parakh SC. Legal aspects of anaesthesia practice. Indian J Anaesth. 2008;52(3):247–257.
7. Gebremedhn EG, Nagaratnam V. Audit on anaesthetic record completeness at a university teaching hospital operation theater of low-resource setting. J Anesth Crit Care Open Access Audit. 2017;8(2):2–6. doi:10.15406/jaccoa.2017.08.00298
8. Statement on documentation of anesthesia care: American society of anesthesiologists; 2018:1–3.
9. Feldman JM. Do anesthesia information systems increase malpractice exposure? Results of a survey. Anesth Analg. 2004;99:840–843. doi:10.1213/01.ANE.0000130259.52838.3B
10. Raff M. An audit of anaesthetic record keeping. South Afr J Anaesth Analog. 2003;9(3):7–9. doi:10.1080/22201173.2003.10873005
11. Gibbs RF. The present and future medicolegal importance of record keeping in anesthesia and intensive care: the case for automation. J Clin Monit. 1989;5(4):251–255. doi:10.1007/BF01618257
12. Woldegerima Y, Kemal S. Clinical audit on the practice of documentation at preanesthetic evaluation in a specialized university hospital. Int J Surg Open. 2019;16:1–5. doi:10.1016/j.ijso.2018.10.006
13. ASA. Statement on Documentation of Anesthesia Care. American Society of Anesthesiologists (ASA); 2018.
14. Australian and New Zealand College of Anaesthetists Professional Document PS06. Guideline on the anaesthesia record: recommendation; 2020.
15. Palaniswamy SR, Jain V, Chakrabarti D, Bharadwaj S. Completeness of manual data recording in the anaesthesia information management system: A retrospective audit of 1000 neurosurgical cases. Indian J Anaesth. 2019;63(10):797–804. doi:10.4103/ija.IJA
16. Ige FO, Adesina K, Fatoba M. Completeness of manual anaesthesia records in a tertiary facility in Nigeria. J Med Trop. 2017;19(2):86–89. doi:10.4103/jomt.jomt
17. Shear TD, Deshur M, Lapin B, et al. Documentation and treatment of intraoperative hypotension: electronic anesthesia records versus paper anesthesia records. J Med Syst. 2017;86(41):1–8. doi:10.1007/s10916-017-0737-0
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

