Back to Journals » Clinical Ophthalmology » Volume 12
Assessment of corneal hysteresis measured by the ocular response analyzer as a screening tool in patients with glaucoma
Authors Schweitzer JA, Ervin M , Berdahl JP
Received 13 March 2018
Accepted for publication 9 July 2018
Published 18 September 2018 Volume 2018:12 Pages 1809—1813
DOI https://doi.org/10.2147/OPTH.S168032
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Justin A Schweitzer,1 Molly Ervin,2 John P Berdahl1
1Vance Thompson Vision, Sioux Falls, SD, USA; 2Sanford School of Medicine, University of South Dakota, Sioux Falls, SD, USA
Background: Corneal hysteresis (CH) is used to determine the level of risk of patients developing glaucoma, categorized as suspect, mild, moderate and severe.
Methods: This is a retrospective review of 126 consecutive eyes presenting, for the first time, at a glaucoma subspecialty clinic. All eyes at initial examination underwent measurement of CH and intraocular pressure using the Goldmann applanation tonometry (IOPgat). Eyes were classified as CH<10 (n=51) or CH≥10 (n=75) and categorized into glaucoma suspect, mild, moderate, or severe glaucoma based on 24-2 Humphrey visual field testing. Additional data included number of topical glaucoma medications.
Results: Of the eyes classified as a CH<10, 45.5% had moderate or severe glaucoma, and 11.8% of eyes with a CH≥10 had moderate or severe glaucoma. In the CH≥10 group, the mean IOPgat was 19.5 mmHg ± 4.72 mmHg (P<0.01) on 1 ± 1.26 (P<0.01) medications in the moderate/severe glaucoma group and 20.13 mmHg ± 4.95 mmHg (P<0.01) on 0.60 ± 0.95 (P<0.01) medications in the glaucoma suspect/mild glaucoma group. In the CH<10 group, mean IOPgat was 20.47 mmHg ± 7.56 mmHg (P<0.01) on 1.79 ± 1.17 (P<0.01) medications in the moderate/severe glaucoma group. Mean IOPgat was 17.54 mmHg ± 5.48 mmHg (P<0.01) on 0.63 ± 0.83 (P<0.01) medications in the glaucoma suspect/mild glaucoma group.
Conclusion: Moderate to severe glaucoma is 2.9 (P<0.01) times more likely to occur in eyes that measure a CH<10 compared to eyes that measure a CH≥10. Although not statistically significant, suspect or mild glaucoma is more common in eyes that measure a CH≥10. Eyes in the CH<10 moderate/severe glaucoma group had statistically significant higher IOPgat (P<0.01) compared to the CH<10 suspect/mild glaucoma group. Measuring CH at initial presentation can help predict the severity of glaucoma.
Keywords: intraocular pressure, visual fields, and corneal biomechanics
Introduction
The most significant risk factor for glaucoma is intraocular pressure (IOP). Treating IOP decreases the incidence of glaucoma1 and its progression.2–4 There are many other risk factors that need to be considered in the management of glaucoma. The biomechanical characteristics of the cornea, especially central corneal thickness (CCT), play a role in the accuracy of IOP measurement and glaucoma risk. The Ocular Hypertension Treatment Study ignited much discussion regarding the role that CCT has on the risk for glaucoma development or progression.5 Along with that discussion there has been speculation that the biomechanical characteristics of the cornea may reflect the vulnerability of the optic nerve head to glaucoma.6 The cornea, sclera, peripapillary ring, and lamina cribrosa, in an individual eye, are essentially made from extracellular matrix coded by the same genes resulting in collagen formation.7 There is speculation that an eye with a more deformable cornea might also have an optic disc that is more likely to suffer glaucomatous damage from raised IOP.6 With increasing age, both the cornea8,9 and the lamina10–12 become more rigid, stiffer, and less resilient. Age-related changes of the connective tissue could be similar in the cornea8 and lamina and because corneal hysteresis (CH) declines with age. The Reichert ocular response analyzer (ORA) (Ametek Reichert Technologies, Depew, NY, USA) measures CH and has been associated with progressive visual field worsening in glaucoma patients.13 A low CH is seen in patients who have glaucoma.13 Patients with a low CH are more likely to respond to topical medications,14 so knowing a patient’s CH can aid in making treatment decisions.
Glaucoma accounts for 9%–12% of all cases of blindness in the United States, with more than 120,000 people blind from this disease.15 It is estimated that over 3 million Americans have glaucoma.16 The challenge faced by all eye care providers when managing this disease is identifying how severe each individual case is, and the likelihood, as well as the rapidity of progression. Measurement of CH with the ORA can aid in determining the risk level of patients presenting with glaucoma, and thus help determine the appropriate treatment interventions.
In this study, we used CH measured by the ORA to determine risk level of new patients presenting as glaucoma suspect, mild glaucoma, moderate glaucoma, or severe glaucoma.
Methods
Patients
Data from the charts of 63 subjects, 126 eyes, presenting to a glaucoma subspecialty clinic for the first time between 2013 and 2014 were used in a retrospective review. All measurements included were measured at their first visit. Subjects only underwent measurement of CH of both eyes at their initial examination. Both eyes of each patient were included in the study. All types of glaucoma were included. Patients were classified as glaucoma suspect, mild, moderate, or severe glaucoma based on a 24–2 Humphrey Visual Field, and the staging system from the American Glaucoma Society.17 Eyes were classified as having a CH<10 or a CH≥10. In the suspect/mild glaucoma group with CH<10, the mean age was 62.3, with 21 females and 20 males. In the suspect/mild group with CH≥10, the mean age was 61.95, 32 females and 13 males. In the moderate/severe group with CH<10, the mean age was 73.7, 27 females and 7 males. In the moderate/severe group with CH≥10, the mean age was 69.5, with 6 females and 0 males. The subjects were all of Caucasian descent. The region this study was performed in is very homogenous, and this study may not be representative of more diverse regions.
Visual fields
Glaucoma patients were categorized as glaucoma suspect, mild, moderate, or severe glaucoma based on the staging system from the American Glaucoma Society. In this system, a glaucoma suspect is a patient with at least 1 risk factor. Risk factors include family history, race, elevated IOP, optic disk appearance and thin CCT. Patients with optic nerve abnormalities that are consistent with glaucoma but do not have visual field irregularities with white-on-white visual field tests or irregularities found only on short-wavelength automated perimetry were classified as having mild glaucoma. Moderate glaucoma patients were found to have optic nerve irregularities consistent with glaucoma as well as glaucomatous visual field irregularities in only 1 hemifield. Patients in the severe glaucoma category have all of the glaucomatous characteristics as moderate glaucoma patients, but visual field irregularities in both hemifields and/or loss within 5 degrees of fixation in at least 1 hemifield.17
CH
Hysteresis was measured by using the Reichert ORA. This device has previously been explained in detail.6 An air puff is used to create concavity in the cornea as well as an optical sensor that measures the concavity of the cornea. Timed together, the rising and falling pressures that cause the cornea to cave in and out are derived. The difference between the pressures is called hysteresis.
Statistical analysis
Data was recorded and analyzed using Microsoft Excel. Paired t-tests were used to find the statistical significance of the correlation between CH, IOPgat and the number of medications. The chi-squared test was used to find the statistical significance between patients in their respective glaucoma category and whether they had CH<10 or CH≥10.
Ethics approval
The University of South Dakota Institutional Review Board did not require us to obtain patient consent as this study was done in a retrospective manner. We obtained a waiver and de-identified patients before data analysis occurred.
Results
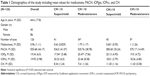
There were 126 eyes used in the study. The demographics of the patients are shown in Table 1.
Eyes in the moderate and severe glaucoma category were 2.9 times more likely to have a CH<10 compared to eyes that measured a CH≥10. This was statistically significant (P<0.01). Eight eyes with moderate/severe glaucoma had CH≥10. Thirty-four eyes with moderate/severe glaucoma had a CH<10. Eyes in the suspect and mild category were more likely to have CH≥10, but it was not statistically significant (P>0.05). Forty-three eyes with mild glaucoma/glaucoma suspect had a CH≥10. Forty-one eyes with mild glaucoma/glaucoma suspect had a CH<10.
Eyes in the CH<10 moderate/severe glaucoma group had a mean IOPgat of 20.47 mmHg (±7.56). When compared to the mean IOPgat of 17.54 mmHg (±7.56) in the CH<10 suspect/mild glaucoma group, there was statistical significance. Eyes in the CH<10 moderate/severe glaucoma group had statistically significant higher IOPgat (P<0.01) compared to the CH<10 glaucoma suspect/mild glaucoma group.
Discussion
CH has been of interest in glaucoma for many years. Recently, several studies have reported that CH can be helpful for predicting the development of glaucoma and its progression.6,13,18,19 Studies that included healthy subjects20–22 found that mean values for CH fall in the range of 10.1–10.9 mmHg. A study of 15 healthy subjects who underwent a 24-hour assessment of IOP, CCT, and CH found that both IOP and CCT showed 24-hour variability. In contrast, CH was found to be stable throughout the 24-hour period, with no significant variation at all.23
The optic nerve head, specifically the lamina cribrosa, is the main site of injury in glaucoma.24,25 The mechanism of glaucomatous damage to the optic nerve head has been thought of as mechanical vs vascular for a long time, but only recently has consideration been given to thinking of the optic nerve head as a biomechanical structure. With this thought process, the impact of IOP-related stresses on the optic nerve head tissue and its blood supply at all levels of IOP are considered.26 This means that the biomechanical response of the optic nerve head tissue, as well as what occurs mechanically and blood flow related secondary to the response, will determine the optic nerve head’s susceptibility to IOP-related damage.
There are some key clinical studies that have supported the role of CH measurement and its role in glaucoma care. Congdon et al identified CH as a risk factor for glaucoma and its progression.13 They provided a retrospective report of 230 glaucoma patients and suspects that showed associations between patient age, lack of treatment, and CH and glaucoma progression. Park et al looked at CH and its role in normal-tension glaucoma.27 They divided the study patients into a group with a CH>10.1 mmHg, and a group with a CH<10.1 mmHg. This was similar to the way we divided our patient groups in regards to CH. Park et al27 found that the risk of progression was 67% in the eyes with a CH<10.1 and only 35% in eyes with a CH>10.1. They concluded that CH can be utilized independently of IOP and CCT as a prognostic factor for glaucoma progression in normal-tension glaucoma. In our study, eyes that were classified as having a CH<10 were 3.85 times more likely to have moderate to severe glaucoma than glaucoma suspects, or have mild glaucoma. Eyes that had a CH≥10, although not statistically significant, trended towards being a glaucoma suspect or mild glaucoma rather than having moderate or severe glaucoma. Our study assessed the level of glaucoma present in the patient, which does differ from the Park et al study,27 which assessed progression. Progression and level of glaucoma present are equally important in management and treatment.
Anand et al studied asymmetric primary open-angle glaucoma in a prospective manner.28 They evaluated Goldmann IOP, CCT, number of glaucoma medications, and CH. The only factor that differed between eyes was CH, and the difference was statistically significant. The study concluded that CH can help in identifying the inferior eye in asymmetric primary open-angle glaucoma. De Moraes et al evaluated the rate of visual field progression in relation to CH.18 The study included 152 eyes and found that eyes progressed faster with lower mean CCT (525 vs 542) and lower CH (7.5 vs 9.0). The study concluded that glaucomatous eyes with low CH and low CCT not only are at risk for progression, but will progress at a faster rate.
Debate exists on how to use CH in a clinical setting and whether it is a truly independent risk factor for glaucoma susceptibility. Clinical cross-sectional studies have shown that it is negatively associated with IOP and positively associated with CCT.8,29 This means a low CH reading could be viewed as a substitute measure for either high IOP or thin CCT, two factors that are already known to be associated with glaucomatous progression. CH has also been found to decrease with age,30,31 with increasing age being a risk factor for glaucoma. The question then arises as to whether CH is truly an independent risk factor for glaucoma, or simply a substitute measure for other factors. We are not claiming it is an independent risk factor in this study but believe it can play a role in assessing risk level of glaucoma present. This can aid in how aggressive treatment decisions need to be and can assist in management decisions in glaucoma patients.
Acknowledgment
This study was presented at American Optometric Association Meeting 2015 Poster Session, June 2015, Seattle Washington.
Disclosure
Dr Justin A Schweitzer is a consultant and speaker for Ametek Reichert Technologies. The authors report no other conflicts of interest in this work.
References
Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701–713. | ||
Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E. Early Manifest Glaucoma Trial Group. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003;121:48–56. | ||
Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Collaborative Normal-Tension Glaucoma Study Group. Am J Ophthalmol. 1998;126(4):487–497. | ||
Collaborative Normal-Tension Glaucoma Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1998;126(4):498–505. | ||
Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714–720. | ||
Wells AP, Garway-Heath DF, Poostchi A, Wong T, Chan KC, Sachdev N. Corneal hysteresis but not corneal thickness correlates with optic nerve surface compliance in glaucoma patients. Invest Ophthalmol Vis Sci. 2008;49(8):3262–3268. | ||
Grytz R, Girkin CA, Libertiaux V, Downs JC. Perspectives on biomechanical growth and remodeling mechanisms in glaucoma. Mech Res Commun. 2012;42:92–106. | ||
Kotecha A, Elsheikh A, Roberts CR, Zhu H, Garway-Heath DF. Corneal thickness- and age-related biomechanical properties of the cornea measured with the ocular response analyzer. Invest Ophthalmol Vis Sci. 2006;47(12):5337–5347. | ||
Elsheikh A, Wang D, Brown M, et al. Assessment of corneal biomechanical properties and their variation with age. Curr Eye Res. 2007;32(1):11–19. | ||
Albon J, Farrant S, Akhtar S, et al. Connective tissue structure of the tree shrew optic nerve and associated ageing changes. Invest Ophthalmol Vis Sci. 2007;48(5):2134–2144. | ||
Albon J, Karwatowski WS, Avery N, Easty DL, Duance VC. Changes in the collagenous matrix of the aging human lamina cribrosa. Br J Ophthalmol. 1995;79(4):368–375. | ||
Albon J, Purslow PP, Karwatowski WS, Easty DL. Age related compliance of the lamina cribrosa in human eyes. Br J Ophthalmol. 2000;84(3):318–323. | ||
Congdon NG, Broman AT, Bandeen-Roche K, Grover D, Quigley HA. Central corneal thickness and corneal hysteresis associated with glaucoma damage. Am J Ophthalmol. 2006;141(5):868–875. | ||
Agarwal DR, Ehrlich JR, Shimmyo M, Radcliffe NM. The relationship between corneal hysteresis and the magnitude of intraocular pressure reduction with topical prostaglandin therapy. Br J Ophthalmol. 2012;96(2):254–257. | ||
National Institutes of Health. Quigley and Vitale. Invest Ophthalmol Vis Sci. 1997. | ||
The Eye Diseases Prevalence Research Group. Prevent Blindness America. Arch Ophthalmol. 2004. | ||
Fellman R, et al. Know the New Glaucoma Staging Codes. American Glaucoma Society, Eye Net. 2011;1. Available from: https://www.americanglaucomasociety.net//client_data/files/2013/324_eyenetoctober2011newglaucomacodes.pdf. Accessed August 5, 2015. | ||
de Moraes CV, Hill V, Tello C, Liebmann JM, Ritch R. Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma. 2012;21(4):209–213. | ||
Medeiros FA, Meira-Freitas D, Lisboa R, Kuang TM, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013;120(8):1533–1540. | ||
Shah S, Laiquzzaman M, Bhojwani R, Mantry S, Cunliffe I. Assessment of the biomechanical properties of the cornea with the ocular response analyzer in normal and keratoconic eyes. Invest Ophthalmol Vis Sci. 2007;48(7):3026–3031. | ||
Carbonaro F, Andrew T, Mackey DA, Spector TD, Hammond CJ. The heritability of corneal hysteresis and ocular pulse amplitude: a twin study. Ophthalmology. 2008;115(9):1545–1549. | ||
Laiquzzaman M, Bhojwani R, Cunliffe I, Shah S. Diurnal variation of ocular hysteresis in normal subjects: relevance in clinical context. Clin Exp Ophthalmol. 2006;34(2):114–118. | ||
Kida T, Liu JH, Weinreb RN. Effect of 24-hour corneal biomechanical changes on intraocular pressure measurement. Invest Ophthalmol Vis Sci. 2006;47(10):4422–4426. | ||
Quigley H, Anderson DR. The dynamics and location of axonal transport blockade by acute intraocular pressure elevation in primate optic nerve. Invest Ophthalmol. 1976;15(8):606–616. | ||
Quigley HA, Addicks EM, Green WR, Maumenee AE. Optic nerve damage in human glaucoma. II. The site of injury and susceptibility to damage. Arch Ophthalmol. 1981;99(4):635–649. | ||
Burgoyne CF, Downs JC, Bellezza AJ, Suh JK, Hart RT. The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog Retin Eye Res. 2005;24(1):39–73. | ||
Park JH, Jun RM, Choi KR. Significance of corneal biomechanical properties in patients with progressive normal-tension glaucoma. Br J Ophthalmol. 2015;99(6):746–751. | ||
Anand A, de Moraes CG, Teng CC, Tello C, Liebmann JM, Ritch R. Lower corneal hysteresis predicts laterality in asymmetric open angle glaucoma. Invest Ophthalmol Vis Sci. 2010;51(12):6514–6518. | ||
Kotecha A, Russell RA, Sinapis A, Pourjavan S, Sinapis D, Garway-Heath DF. Biomechanical parameters of the cornea measured with the Ocular Response Analyzer in normal eyes. BMC Ophthalmol. 2014;14(1):11. | ||
Lau W, Pye D. A clinical description of Ocular Response Analyzer measurements. Invest Ophthalmol Vis Sci. 2011;52(6):2911–2916. | ||
Leite MT, Alencar LM, Gore C, et al. Comparison of corneal biomechanical properties between healthy blacks and whites using the Ocular Response Analyzer. Am J Ophthalmol. 2010;150(2):163–168. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.