Back to Journals » Patient Preference and Adherence » Volume 8
Assessing the mobility of the mandibular condyle by sonography
Authors Chen H, Wu S, Lu C, You J, Lai C
Received 10 August 2014
Accepted for publication 3 September 2014
Published 15 October 2014 Volume 2014:8 Pages 1419—1425
DOI https://doi.org/10.2147/PPA.S72532
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Johnny Chen
Han-Yu Chen,1 Shyi-Kuen Wu,1 Chuan-Chin Lu,1,2 Jia-Yuan You,3 Chung-Liang Lai4
1Department of Physical Therapy, Hungkuang University, Taichung, Taiwan; 2Department of Rheumatology, Taichung Hospital, Department of Health, Taiwan; 3Department of Physical Therapy, I-Shou University, Kaohsiung, Taiwan; 4Department of Physical Medicine and Rehabilitation, Taichung Hospital, Department of Health, Taiwan
Purpose: Traditionally, the measurement of the maximal mouth opening was regarded as the mobility of the temporomandibular joint. The information, however, was not reliable. Sonography was often used to diagnose disc displacement in the temporomandibular joint and its validity was well established. The tool was also appropriate for measuring the outcome of temporomandibular disorders management. Therefore, the purpose of the study was to examine completely the reliability and error for evaluating the mobility of the mandibular condyle by sonography. In addition, the existing methods were modified to improve the repeatability.
Patients and methods: The reliability examinations included between-image and within-image explorations to represent the reliabilities of the image capturing and the mobility measuring, respectively. Sixty-two subjects were recruited to receive ultrasonic examination for condylar mobility. The images of the condyle in mouth closing and opening were captured and the horizontal displacement of the condyles was measured as the anterior translation of the condyle. To confirm that the probe did not move during mouth opening, a marker was placed between the skin and the ultrasonic probe as the landmark.
Results: The results demonstrated that the intrarater and interrater reliabilities in the within-image test were 0.986 and 0.970 and the reliabilities in the between-image test were 0.904 and 0.857, respectively. The standard errors of measurement in the within-image and between-image tests were 0.04 cm and 0.09 cm, respectively.
Conclusion: Sonography is a reliable tool to assess condylar mobility and can be used to measure the treatment outcome for temporomandibular disorders.
Keywords: temporomandibular disorders, sonography, mandibular condyle, reliability
Introduction
Temporomandibular disorders (TMDs) are a common orofacial disease.1 In epidemiological reports, there are approximately 10%–15% of adults with TMD.2 The clinical symptoms are pain, clicking, limitation of mouth opening, or deviation of mouth-opening movement.3 Joint pain and limitation of mouth opening are especially going to critically affect mastication, speaking, and other oral functions in a patient’s daily life. Many studies were designed to examine the effectiveness of treatment for TMD. The results of the systematic reviews, however, showed that the findings must be interpreted with caution due to invalid or unreliable outcome measures.4,5 The maximal mouth opening is often measured to show the treatment outcome. Therefore, a tool to evaluate the motion of the temporomandibular joint (TMJ) is necessary for the outcome measures of TMD management.
Traditionally, the distance between the tips of the upper and lower incisors was measured by a caliper,6 slide gauge,7 tape measure,8 or millimeter ruler9 as the range of the mouth opening. Furthermore, the total vertical opening was also measured to indicate the range of the mouth opening.5 Several studies, however, had found a difference in the maximal mouth opening between subjects with different skeleton and occlusion morphology.10,11 Therefore, scholars suggested that the maximal mouth opening cannot provide reliable information regarding TMJ mobility.12,13 Moreover, the symptoms of TMD are often associated with the asymmetric and deviated motion of a lower jaw during mouth opening. Therefore, limitation of lateral movement away from the affected side and the deviation of the mandible to the affected side during mouth opening will be found.14 The measurement of the distance between the upper and lower incisors or the total vertical opening without considering the jaw deviation may cause some errors such that the mobility of TMJ cannot be actually represented by the distance. The increment of the distance measured from the upper incisor to the lower incisor might be found in the exacerbation of the deviation. Conversely, the reduction of the distance might also be obtained when the deviation was improved by increasing the mobility of hypomobile TMJ. These conditions will mislead the outcome measure of TMD management.
Arthrokinematic movements of TMJ involve rolling, distraction, anterior gliding, and medial, lateral gliding of the mandibular condyle relative to the mandibular fossa of the temporal bone.15 Furthermore, joint mobilization techniques are used to increase the mobility of distraction and gliding of the mandibular condyle to correct TMJ disorders.16 Consequently, the displacement of the mandibular condyle may indicate the magnitude of the mouth opening and be used to examine the outcome of joint mobilization techniques. Because of the difficulty of measuring directly on the surface, it is important to find a simple and convenient tool to detect the mobility of the mandibular condyle.
Sonography is a fast, less expensive,17 no radiation, and noninvasive technique enabling dynamic imaging of the TMJ.18,19 Several studies compared magnetic resonance imaging and sonography in the diagnosis of TMD20–22 and demonstrated that the sensitivity, specificity, and accuracy were 64%–78%, 75%–78%, and 70%–78%, respectively, in closed mouth and 61%–68%, 63%–88%, and 65%–77%, respectively, in open mouth.23–25 Moreover, a recent study reported that sonography has higher sensitivity for the evaluation of individual condylar sliding than clinical measurement of maximum interincisal movements and is a sensitive tool for assessing joint function.12 Investigation into the reliability of measuring the gliding of the mandibular condyle was, however, rare. Therefore, the purpose of the study was to establish the reliability for evaluating the motion of the mandibular condyle by sonography.
Materials and methods
Subjects
Thirty-eight subjects (28 female, ten male; mean age 36.1±8.3 years) with unilateral TMD were recruited according to the research diagnostic criteria (RDC)/TMD criteria26 by an experienced physical therapist and their clinical symptoms of pain, click, and limited mouth opening corresponding with the RDC/TMD Axis I diagnosis of disc displacement with reduction (group IIa) and without reduction with limited opening (group IIb). Their affected sides were tested. Exclusion criteria were the subjects having one of the following conditions: rheumatic diseases, recent trauma, and wearing a stabilization splint or dental braces for orthodontics. The condylar movements were limited in these groups of patients. Therefore, if the limited condylar movement can be detected by sonography, this technology can be applied in clinical practice to observe general condylar movement. In addition, 24 nonsymptomatic subjects (nine female, 15 male; mean age 33.5±7.8 years) were recruited to correct the basic data of condylar mobility measured by sonography. Both sides were measured and the averages were obtained. All subjects were fully informed of the test procedures and the purpose of the study. Written informed consent approved by the Ethics Committee of the author’s university was obtained from all subjects.
Detection of condylar motion
Condylar motion was assessed by ultrasound apparatus (SonoSite 180 Plus; SonoSite Inc., Bothwell, WA, USA). The probe (5–10 MHz, linear array) was placed on the joint site transversely at the level of the zygomatic arch. The picture of the condyle as the mouth closed was captured and recorded after viewing the clear condyle. Holding the probe on the same site afterward, the subject was instructed to open his or her mouth as wide and as gently as possible. Similarly, the picture of the condyle as the mouth opened was captured and recorded after the clear condyle was viewed. An echoabsorptive marker X was placed between the skin and the ultrasonic probe as a means to confirm that the probe did not move during mouth opening. The subject was examined in a sitting position. The examiner stood behind the subject with one hand holding the probe to execute the examination and another hand placed on the temporal area of the untested side to fix the subject’s head. Before examining, the subject was instructed to practice mouth opening and closing three times to confirm that the mouth movement would not be interrupted by the fixation. The recorded pictures were transported to the personal computer to await further analysis.
Image processing
The software CorelDRAW X5 was used to process all the images. The mouth-closed image was put above the mouth-opened image and lined up with the shadow of the marker X. Two separate vertical lines were drawn through the centers of the condyles on these two images. The horizontal distance of these two vertical lines was measured and converted to the actual value in proportion to the scale and regarded as the anterior translation of the mandibular condyle during mouth opening (Figure 1).
The procedures of locating the positions and measuring the displacement between two mandibular condyles in mouth closing and opening were repeated twice on different days by the same examiner for testing the intrarater reliability; these were conducted twice in a day by two separate examiners for testing the interrater reliability. The reliability of examining the same image from one subject indicated the within-image investigation while the different images from the same subject indicated the between-image investigation to represent the reliabilities of the mobility measuring and the image capturing, respectively. Two examiners, who were physical therapists with experience of sonographic assessment for 1.5 years and 1 year, respectively, spent 2 weeks before formal examination becoming familiar with operating the ultrasound apparatus, associating the anatomy atlas with the sonography, and interpreting images. The flow chart of the reliability examination is shown in Figure 2.
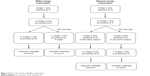  | Figure 2 Flow chart of the reliability examination. |
Statistical analysis
All data were analyzed using the Statistical Package for Social Sciences (SPSS for Windows, Version 11.0; SPSS Inc., Chicago, IL, USA). One-way analysis of variance was used to test the difference among the three groups in within-image or between-image examinations. The intraclass correlation coefficients (ICCs) were calculated for reliability, and the stability and consistency of the parameters measurement were examined by standard error of measurement (SEM) and coefficient of variation (CV). The descriptive data were demonstrated with mean ± standard deviation. The sonography was expected to be a measurement tool of treatment outcome, so the minimal detectable difference (MDD) would also be estimated. The MDD was calculated using the following formula:
| (1) |
Results
The mean condylar translations in within-image and between-image examinations for each group are presented in Table 1. The mean translation of the mandibular condyle obtained from the subjects in group IIb was significantly smaller than that from the subjects in group IIa and the nonsymptomatic group in within-image as well as between-image examinations. The results of intrarater reliability, interrater reliability, SEM, CV, and MDD95% in the within-image and between-image tests are summarized in Table 2. The ICCs of the intrarater reliability in both the within-image and between-image situations and the interrater reliability in the within-image situation were all excellent (ICC >0.9). The interrater reliability in the between-image situation was good (ICC >0.8). The values of the SEMs and MDDs95% in the within-image situation were smaller than those in the between-image situation. The CV in the within-image, however, was greater than that in the between-image situation.
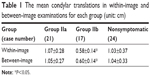  | Table 1 The mean condylar translations in within-image and between-image examinations for each group (unit: cm) |
Discussion
The results of the current study show the excellent reliabilities of sonography to assess the mobility of the mandibular condyle. Nevertheless, the magnitudes of the mandibular condylar anterior translation were different for all subjects in the present study due to the different severities of limitation in range of mouth opening. Consequently, the patients’ diverse conditions caused the larger CVs, which were 39.3% and 34.3% for intrarater within-image and between-image assessments, respectively. In addition, the SEM indicated the stability of repeated responses over time. The study revealed that the intrarater SEMs were 0.04 cm and 0.09 cm for the within-image and between-image assessments, respectively. The values can be used to estimate for the entire group, based on the confidence interval (CI) as expressed in the following equation:
95% CI = observed score ± 1.96 * SEM | (2) |
Therefore, the within-image and between-image intrarater SEMs will fall in this range of observed score ±0.08 and 0.18 with the 95% CI, respectively. Furthermore, to address the outcome of treatment, the observed differences from before to after treatment must reflect true change and not simply random measurement error.27 The SEM is also the most common statistic used to determine the MDD, the smallest change above the threshold of error expected in the measurement. MDD95% means that 95% of stable subjects present a random variation of less than this amount when tested on multiple occasions. The intrarater MDD95% in the current study was 0.11 cm for within-image assessment. People can expect 95% of stable subjects in this population to show random variation of <0.11 cm in repeated trials of the within-image assessment. Therefore, as the intrarater within-image sonography was used to assess the mandibular condylar translation before and after intervention, a change of ≥0.11 cm would be considered true change.
In previous applications on TMJ, sonography was often used for diagnosis; for example, the diagnoses of anterior disc displacement, joint effusion, and condylar erosion and the relational sensitivity, specificity, and accuracy have been reported.28 Few investigations, however, were to examine the reliability of sonography to assess TMJ, except for the evaluation of the disc position.29 Past studies concerning the condylar motion included description of the track,30 the mean measurement difference,20 and the absolute and relative error12 without providing any data of reliability or agreement. The present study examined completely the reliabilities of sonography to assess the condylar motion, including the intrarater and interrater reliabilities with the within-image and between-image conditions. This was because the identification of the condyle would be affected by the quality of the images even if they were from the same subject. Therefore, the complete examination for reliability was focused not only on the image interpretation but also on the image capture ability. The results demonstrated that the within-image reliabilities were better than the between-image reliabilities regardless of interrater or intrarater examinations. The intrarater within-image reliability was almost 0.99 with higher reliability and lower SEM; therefore, this type of assessment was suggested in clinical application. Moreover, the possible reason for the higher ICCs obtained in the current study was that the identification of the skeleton (condyle) was easier than that of the muscle when compared with the measurement of local cross-sectional dimensions of the masseter.31
The mean translation of the mandibular condyle with merging the data of group IIa and IIb in the current study, which were 0.85±0.33 cm and 0.85±0.29 cm in within-image and between-image examinations, respectively, was similar to the results of the investigation conducted by Landes and Sader.12 The authors reported that the mean translation of the condyle for the symptomatic patients whose symptoms included disc displacement with and without reduction was 0.9±0.39 cm. In the nonsymptomatic investigation, the mean condylar translations were 1.03±0.37 cm and 1.04±0.33 cm in within-image and between-image examinations, respectively, which was also similar to 1.09±0.36 cm obtained from asymptomatic subjects with Angle Class III in the previous study.12 The measurements, however, were different between these two sonographic studies. The Landes and Sader study measured the distance, but the current study measured the horizontal displacement, from two identical condylar locations during mouth opening. According to the placement of the probe, the horizontal displacement indicated the anterior translation, and the vertical displacement indicated the medial or lateral translation of the condyle. To assess the treatment outcome of manual joint mobilization techniques, including the anterior gliding and medial and lateral gliding in clinical application,16 it is necessary to examine the condylar mobility along the direction of treatment.
Another characteristic of the study was the image capturing and processing. A marker X was set between the skin and the probe as a landmark to certify that the probe did not move during mouth opening.32–34 If movement occurred, the displacement measurement would be influenced. The shadow of the marker X in the image was regarded as the reference to line up the mouth-closing and mouth-opening images to increase the accuracy of measurement.
The motions of mandibular condyle include anterior translation, inferior translation, and lateral and medial translation during mouth opening. Only the anterior translation was measured in the study because this motion can be observed in the scanning field, as the probe was placed horizontally along the level of the zygomatic arch and the tracks were consistent for all subjects. In the pilot study, the probe was also placed vertically along the level of the ramus to observe the inferior translation of the mandibular condyle.20 However, the track of the condylar motion was often out of the scanning field while the mouth was open, due to the greater anterior translation. Moreover, in the symptomatic TMJ, the occurrences of medial or lateral translations were inconsistent. Therefore, the last two motions of the mandibular condyle were not measured in the present study. In future work, the examination of these two motions may be improved by way of replacing the type of ultrasound probe and changing the strategy of subject classification.
As an assessment tool for TMJ, there were some limitations for sonography. Firstly, the inferior translation of the condylar motion is not easily observed, and that will lead to the restriction of inferior translation not being detected and the treatment outcome of the distraction technique not being measured. Secondly, both TMJs should move simultaneously and symmetrically in normal function. If the restriction occurred in one joint, another would also have an abnormal performance. In general, however, it is rare to have two ultrasound apparatuses to observe the two joints simultaneously. This question can perhaps be resolved by establishing the relationship between the lateral or medial condylar translation and the deviation of the mouth opening.
The placement of the probe in the current work was the same as that in the Landes and Sader12 study. Three movements of the mouth, including open, protrusion, and mediotrusion, were examined in their study, however, while only open movement was tested in our work. The main reason was the difference of the subject inclusion criteria. In the Landes and Sader study, the Angle classification method was used to classify TMD patients for three levels of occlusion with the alignment of teeth and bite, which were structural factors. The RDC/TMD criteria, however, were used in the present study to classify TMD patients with the click sound production and limitation in mouth opening, which were functional factors. To consider sonography as the measurement tool of treatment outcome, the functional improvement will be more important than the structural change. Therefore, the RDC/TMD criteria were used and the mouth-opening movement was examined in the current study.
Conclusion
Assessment of the mandibular condylar mobility by sonography has the advantage of real-time and dynamic observation with high reproducibility and low SEM. The results of the present study can be regarded as the reference for the clinical application of sonography to measure the mandibular condylar mobility and show that sonography is a reliable tool to measure the treatment outcome for patients with TMD.
Acknowledgment
This work was supported by grants from Hungkuang University (number: HK-100-B-08), Taichung, Taiwan.
Disclosure
No conflict of interest exists in the submission of this manuscript, and the manuscript is approved by all authors for publication.
References
Romero-Reyes M, Uyanik JM. Orofacial pain management: current perspectives. J Pain Res. 2014;21(7):99–115. | ||
Macfarlane TV, Glenny AM, Worthington HV. Systematic review of population-based epidemiological studies of orofacial pain. J Dent. 2001;29(7):451–467. | ||
Peck CC, Murray GM, Gerzina TM. How does pain affect jaw muscle activity? The Integrated Pain Adaptation Model. Aust Dent J. 2008;53(3):201–207. | ||
McNeely ML, Armijo Olivo S, Magee DJ. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther. 2006;86(5):710–725. | ||
Medlicott MS, Harris SR. A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorder. Phys Ther. 2006;86(7):955–973. | ||
Oliveira-Campelo NM, Rubens-Rebelatto J, Martí N-Vallejo FJ, Alburquerque-Sendí NF, Fernández-de-Las-Peñas C. The immediate effects of atlanto-occipital joint manipulation and suboccipital muscle inhibition technique on active mouth opening and pressure pain sensitivity over latent myofascial trigger points in the masticatory muscles. J Orthop Sports Phys Ther. 2010;40(5):310–317. | ||
Nicolakis P, Erdogmus B, Kopf A, et al. Effectiveness of exercise therapy in patients with internal derangement of the temporomandibular joint. J Oral Rehabil. 2001;28(12):1158–1164. | ||
Foster ME, Gray RJ, Davies SJ, Macfarlane TV. Therapeutic manipulation of the temporomandibular joint. Br J Oral Maxillofac Surg. 2000;38(6):641–644. | ||
Goulet JP, Clark GT, Flack VF, Liu C. The reproducibility of muscle and joint tenderness detection methods and maximum mandibular movement measurement for the temporomandibular system. J Orofac Pain. 1998;12(1):17–26. | ||
Lewis RP, Buschang PH, Throckmorton GS. Sex differences in mandibular movements during opening and closing. Am J Orthod Dentofac Orthop. 2001;120(3):294–303. | ||
Naeije M. Local cinematic and anthropometric factors related to the maximum mouth opening in healthy individuals. J Oral Rehab. 2002;29(6):534–539. | ||
Landes CA, Sader R. Sonographic evaluation of the ranges of condyle translation and of temporomandibular joint space as well as first comparison with symptomatic joints. J Craniomaxillofac Surg. 2007;35(8):374–381. | ||
Travers KH, Buschang PH, Hayasaki H, Throckmorton GS. Associations between incisor and mandibular condylar movements during maximum mouth opening in humans. Arch Oral Biol. 2000;45(4):267–275. | ||
Kurita H, Kurashina K, Ohtsuka A. Efficacy of a mandibular manipulation technique in reducing the permanently displaced temporomandibular joint disc. J Oral Maxillofac Surg. 1999;57(7):784–787. | ||
Neumann DA. Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation. St Louis, MO: Mosby; 2002. | ||
Kaltenborn FM. Manual Mobilization of the Joints. Volume I: The Extremities. 5th ed. Oslo, Norway: Olaf Norlis Bokhandel; 1999. | ||
Hayashi T, Ito J, Koyama J, Yamada K. The accuracy of sonography for evaluation of internal derangements of the temporomandibular joint in asymptomatic elementary school children: comparison with MR and CT. AJNR Am J Neuroradiol. 2001;22(4):728–734. | ||
Melchiorre D, Calderazzi A, Maddali Bongi S, et al. A comparison of ultrasonography and magnetic resonance imaging in the evaluation of temporomandibular joint involvement in rheumatoid arthritis and psoriatic arthritis. Rheumatology. 2003;42(5):673–676. | ||
Tvrdy P. Methods of imaging in the diagnosis of temporomandibular joint disorders. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2007;151(1):133–136. | ||
Landes C, Walendzik H, Klein C. Sonography of the temporomandibular joint from 60 examinations and comparison with MRI and axiography. J Craniomaxillofac Surg. 2000;28(6):352–361. | ||
Elias FM, Birman EG, Matsuda CK, Olivira IR, Jorge WA. Ultrasonographic findings in normal temporomandibular joint. Braz Oral Res. 2006;20(1):25–32. | ||
Kaya K, Dulgeroglu D, Unsal-Delialioglu S, et al. Diagnostic value of ultrasonography in the evaluation of the temporomandibular joint anterior disc displacement. J Craniomaxillofac Surg. 2010;38(5):391–395. | ||
Jank S, Rudisch A, Bodner G, Brandlmaier I, Gerhard S, Emshoff R. High-resolution ultrasonography of the TMJ: helpful diagnostic approach for patients with TMJ disorders? J Craniomaxillofac Surg. 2001;29(6):366–371. | ||
Tognini F, Manfredini D, Melchiorre D, Bosco M. Comparison of ultrasonography and magnetic resonance imaging in the evaluation of temporomandibular joint disc displacement. J Oral Rehabil. 2005;32(4):248–253. | ||
Cakir-Ozkan N, Sarikaya B, Erkorkmaz U, Akturk Y. Ultrasonographic evaluation of disc displacement of the temporomandibular joint compared with magnetic resonance imaging. J Oral Maxillofac Surg. 2010;68(5):1075–1080. | ||
Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6(4):301–355. | ||
Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River, NJ: Pearson Education, Inc., 2009. | ||
Melis M, Secci S, Ceneviz C. Use of ultrasonography for the diagnosis of temporomadibular joint disorders: a review. Am J Dent. 2007;20(2):73–78. | ||
Emshoff R, Jank S, Rudisch A, Walch C, Bodner G. Error patterns and observer variations in the high-resolution ultrasonography imaging evaluation of the disk position of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(3):369–375. | ||
Braun S, Hicken JS. Ultrasound imaging of condylar motion: a preliminary report. Angle Orthod. 2000;70(5):383–386. | ||
Bertram S, Bodner G, Rudisch A, Brandlmaier I, Emshoff R. Effect of scanning level and muscle condition on ultrasonographic cross-sectional measurements of the anterior masseter muscle. J Oral Rehabil. 2003;30(4):430–435. | ||
Kubo K, Kawakami Y, Kanehisa H, Fukunaga T. Measurement of viscoelastic properties of tendon structures in vivo. Scand J Med Sci Sports. 2002;12(1):3–8. | ||
Maganaris CN, Reeves ND, Rittweger J, et al. Adaptive response of human tendon to paralysis. Muscle Nerve. 2006;33(1):85–92. | ||
Reeves ND, Narici MV, Maganaris CN. Myotendinous plasticity to ageing and resistance exercise in humans. Exp Physiol. 2006;91(3):483–498. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.